
Every child in the United States has a right to a public education, this includes children with Autism and other disabilities. The Individuals with Disabilities Education Act (IDEA), is the federal law that guarantees a free and appropriate public education in the least restrictive environment for every student with a disability. The law’s 2004 reauthorization (P.L. 108-446) further defined children’s rights to educational services and strengthened the role of parents/care providers in their children’s educational planning process. This means that the education for students enrolled in public school should come at no cost and should be appropriate for their age, ability, and developmental level.
The law specifies that educational placement should be on an individual basis, not solely on the diagnosis or category of disability.
Parents/care providers have a voice in the educational process. But keep in mind that IDEA requires that an appropriate educational program be provided, but not necessarily the one that is “ideal” for every child. It is important that parents/care providers work with the school to get the educational support and services the student needs.
Educational planning for students with Autism often addresses a wide range of skill development, including academics, communication and language, social skills, self-help skills, behavioral issues, self-advocacy, and leisure-related skills. It’s important to consult with professionals trained specifically in Autism to help a child benefit from their school program. Obtaining a range of opinions is also useful.

- The National Center for Education Statistics maintains a large database of special education demographics.
- The United States Department of Education has dedicated special education statistic resources.
- Approximately 11% of special education students in the United States receive education under the eligibility of Autism.

IEP Information
The Individualized Education Program (IEP) is a written document that outlines a child’s education. As the name implies, the education program should be tailored to the individual student to provide the maximum benefit. The keyword is individual . A program that is appropriate for one child with Autism may not be right for another.
The IEP is the cornerstone for the education of a child with a disability. It should identify the services a child needs so that he/she will meet their learning objectives during the school year. It is also a legal document that outlines:
- The child’s special education plan (goals for the school year)
- Services needed to help the child meet those goals
- A method for evaluating the student’s progress
The objectives, goals, and selected services are not just a collection of ideas on how the school may educate a child; the school district must educate your child in accordance with the IEP.
To develop an IEP, the local education agency officials and others involved in the child’s educational program meet to discuss education-related goals. By law, the following people must be invited to attend the IEP meeting:
- One or both of the child’s parents/care providers
- The child’s teacher or prospective teacher
- A representative of the public agency (local education agency), other than the child’s teacher, who is qualified to provide or supervise the provision of special education
- The child, if appropriate
- Other individuals at the discretion of the parent(s)/care provider(s) or agency (e.g. a physician, advocate, or neighbor)
IEP meetings must be held at least once annually, but may be held more often if needed. Parents/care providers may request a review or revision of the IEP at any time. While teachers and school personnel may come prepared for the meeting with an outline of goals and objectives, the IEP is not complete until it has been thoroughly discussed and all parties agree to the terms of the written document. Parents/care providers are entitled to participate in the IEP meeting as equal participants with suggestions and opinions regarding their child’s education. They may bring a list of suggested goals and objectives as well as additional information that may be pertinent to the IEP meeting.
The local education agency (LEA) must attempt to schedule the IEP meeting at a time and place agreeable to both school staff and parents/care providers. School districts must notify parents/care providers in a timely manner so that they will have an opportunity to attend. The notification must indicate the purpose of the meeting (i.e., to discuss transition services, behavior problems interfering with learning, academic growth).
Learn more about:
- The IEP Meeting
- Related Services
- Teacher/Staff Requirements
- Goals/Objectives/Evaluation

After an evaluation has been done, the IEP meeting will be scheduled. Parents/care providers are entitled by law to attend and participate in this meeting, and must be given ample notification of the time and place. Parents/care providers should also request a copy of the evaluation results prior to the meeting so you have time to review them.
When preparing for your IEP meeting, consider the following:
- What is your vision for your child – for the future as well as the next school year?
- What are your child’s strengths, needs, and interests?
- What are your major concerns about his/her education?
- What has and has not worked in your child’s education thus far?
- Does the evaluation fit with what you know about your child?
- Are there any special factors to consider, such as communication needs or a positive behavioral intervention plan?
While the IEP meeting is meant to develop an education plan for the student, it is also an opportunity for families to share information about their child and their expectations and what techniques have worked at home. If for some reason parents/care providers disagree with the proposed IEP, there is recourse.
Content of the IEP
The IEP should address all areas in which a child needs educational assistance. These can include academic and non-academic goals if the services to be provided will result in educational benefit for the child. All areas of projected need, such as social skills (playing with other children, responding to questions), functional skills (dressing, crossing the street), and related services (occupational, speech, or physical therapy) can also be included in the IEP.
The IEP (see statute text ) should list the setting in which the services will be provided and the professionals who will provide the service. Content of an IEP must include the following:
- A statement of the child’s present level of educational performance. This should include both academic and nonacademic aspects of his/her performance.
- A statement of specific, well-defined goals that the student may reasonably accomplish within the next 12 months. These goals should directly relate to a student’s disability-related needs, and include baseline data supported by the student’s present level of academic and functional performance. It must be clear how goal progress will be monitored and reported
- If your child takes an alternative assessment aligned with alternate achievement standards (ex: Common Core Essential Elements), their IEP goals must include a description of short-term benchmarks or objectives. These objectives help parents/caregivers and educators know whether a student is progressing, or is in need of additional support.
- A description of all specific special education and related services, including individualized instruction and related support and services to be provided (e.g., occupational, physical, and speech therapy; transportation; recreation). This includes the extent to which the child will participate in regular educational programs.
- The initiation date and duration of each of the services, as determined above, to be provided (this can include extended school year services). You may include the person who will be responsible for implementing each service.
- If your child is 16 years of age or older, the IEP must include a description of transition services (a coordinated set of activities to assist the student in movement from school to post-secondary education, employment, or other activities).
Post-Secondary
Transition planning.
Planning for transitions and life after high school is imperative. This is the process that prepares students for adult life after they leave high school. Transition is the bridge between school programming and adult life that might include higher education, employment, independent living, and participation in adult life in the community.
Transition services are mandated under IDEA for children with disabilities ages 16 and up. An Individualized Transition Plan (ITP) is developed for each student. The ITP identifies the desired and expected outcomes for each student and their families once they leave school as well as the support needed to achieve these outcomes.
- The Center on Secondary Education for Students with Autism Spectrum Disorders : The Center on Secondary Education for Students with Autism Spectrum Disorder (CSESA) is a research and development project funded by the U.S. Department of Education that focuses on developing, adapting, and studying a comprehensive school and community-based education program for high school students who experience Autism.
- The National Technical Assistance Center on Transition : The Collaborative (NTACT:C) is a Technical Assistance Center co-funded by the U.S. Department of Education’s Office of Special Education Programs (OSEP) and the Rehabilitation Services Administration (RSA).
Info & Resources
Many adults with Autism pursue higher education, earning degrees in their preferred field of study. Many colleges have resources dedicated to supporting students with disabilities such as the student disability service center which may be a component of the college program or additive programs such as the College Internship Program that support students attending colleges and universities. There are also programs available that offer social, academic, career, and life skills support for students who have an intellectual disability that may co-occur with Autism and are not pursuing an academic degree. Information about this type of programming support can be found here .
The experience of attending college or university is a big transition for every student. For students with Autism it may require careful planning to ensure adequate support is in place. Unlike in high school, college and university students must disclose their need for accommodations for instructors and engage in self-advocacy to ensure appropriate accommodations.
Accessing the campus disability support center and inquiring about options for support is an excellent first step. Some of the accommodations that are commonly provided at colleges and universities include: testing accommodations, audio recording of lectures, note-taking services, assistive technologies such as speech to text software, priority class registration, and even housing modifications.
- Each college has a unique culture. Assessing the fit for the individual is important. Size, location, types of support, and academic programming should all be considered. Many adults with Autism report a great college experience, and with a little planning and preparation this can be true for you as well.
- Think College : Think College is a national organization dedicated to developing, expanding, and improving inclusive higher education options for people with intellectual disability.
- College Internship Program : The College Internship Program (CIP) is a private young adult transition program for individuals 18-26 with Autism, ADHD, and other learning differences offering comprehensive and specialized services.
- The Office of Special Education and Rehabilitation Services has an excellent information resource on transition services.
Connect to support from the Autism Society

6110 Executive Boulevard Suite 305 Rockville, Maryland 20852
1 (800) 328-8476 [email protected]
Information
Subscribe to our newsletter, accredited seals.
© 2024 Autism Society

Autism Spectrum Disorder
The National Institute of Mental Health (NIMH) , a component of the National Institutes of Health ( NIH ), is a leading federal funder of research on ASD .
What is autism spectrum disorder?
Autism spectrum disorder (ASD) refers to a group of complex neurodevelopment disorders caused by differences in the brain that affect communication and behavior. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)—a guide created by the American Psychiatric Association used to diagnose health conditions involving changes in emotion, thinking, or behavior (or a combination of these)—people with ASD can experience:
- Challenges or differences in communication and interaction with other people
- Restricted interests and repetitive behaviors
- Symptoms that may impact the person's ability to function in school, work, and other areas of life
ASD can be diagnosed at any age but symptoms generally appear in early childhood (often within the first two years of life). Doctors diagnose ASD by looking at a person's behavior and development. The American Academy of Pediatrics recommends that all children get screened for developmental delays and behaviors often associated with ASD at their 18- and 24-month exams.
The term “spectrum” refers to the wide range of symptoms, skills, and levels of ability in functioning that can occur in people with ASD. ASD affects every person differently; some may have only a few symptoms and signs while others have many. Some children and adults with ASD are fully able to perform all activities of daily living and may have gifted learning and cognitive abilities while others require substantial support to perform basic activities. A diagnosis of ASD includes Asperger syndrome, autistic disorder, childhood disintegrative disorder, and pervasive developmental disorder not otherwise specified that were once diagnosed as separate disorders.
In addition to differences or challenges with behavior and difficulty communicating and interacting with others, early signs of ASD may include, but are not limited to:
- Avoiding direct eye contact
- Delayed speech and language skills
- Challenges with nonverbal cues such as gestures or body language
- Showing limited interest in other children or caretakers
- Experiencing stress when routines change
Scientists believe that both genetics and environment likely play a role in ASD. ASD occurs in every racial and ethnic group, and across all socioeconomic levels. Males are significantly more likely to develop ASD than females.
People with ASD also have an increased risk of having epilepsy. Children whose language skills regress early in life—before age 3—appear to have a risk of developing epilepsy or seizure-like brain activity. About 20 to 30 percent of children with ASD develop epilepsy by the time they reach adulthood.
Currently, there is no cure for ASD. Symptoms of ASD can last through a person's lifetime, and some may improve with age, treatment, and services. Therapies and educational/behavioral interventions are designed to remedy specific symptoms and can substantially improve those symptoms. While currently approved medications cannot cure ASD or even treat its main symptoms, there are some that can help with related symptoms such as anxiety, depression, and obsessive-compulsive disorder. Medications are available to treat seizures, severe behavioral problems, and impulsivity and hyperactivity.
How can I or my loved one help improve care for people with autism spectrum disorder?
Consider participating in a clinical trial so clinicians and scientists can learn more about ASD and related conditions. Clinical trials are studies that use human volunteers to look for new or better ways to diagnose, treat, or cure diseases and conditions.
All types of volunteers are needed—people with ASD, at-risk individuals, and healthy volunteers—of all different ages, sexes, races, and ethnicities to ensure that study results apply to as many people as possible, and that treatments will be safe and effective for everyone who will use them.
For information about participating in clinical research visit NIH Clinical Research Trials and You . Learn about clinical trials currently looking for people with ASD at Clinicaltrials.gov .
Where can I find more information about autism spectrum disorder? The following resources offer information about ASD and current research: American Academy of Pediatrics Centers for Disease Control and Prevention (CDC) Eunice Kennedy Shriver National Institute of Child Health and Human Development Interagency Autism Coordinating Committee (IACC) National Center for Advancing Translational Sciences National Institute on Deafness and Other Communication Disorders National Institute of Environmental Health Sciences The National Task Group on Intellectual Disabilities and Dementia Practices (NTG) Additional organizations offer information, research news, and other resources about ASD for individuals and caregivers, such as support groups. These organizations include: Association for Science in Autism Treatment Autism National Committee (AUTCOM) Autism Network International (ANI) Autism Research Institute (ARI) Autism Science Foundation Autism Society Autism Speaks, Inc.

- Copy/Paste Link Link Copied
Educational and School-Based Therapies for Autism
Children with autism are guaranteed free, appropriate public education under the federal laws of Public Law 108-177: Individuals with Disabilities Education Improvement Act (2004) , sometimes called "IDEA."
IDEA ensures that children diagnosed with certain disabilities or conditions, including autism spectrum disorder (ASD), get free educational services and educational devices to help them to learn as much as they can.
NICHD-funded researchers have also incorporated communications interventions for children with ASD within the classroom setting, with successful outcomes. Although the specific interventions used in the study are not a guaranteed part of IDEA, components from the program could provide an important evidence-based foundation for future school-based therapies. 1
IDEA Covers Children and Young Adults

Educational Environment
IDEA states that children must be taught in the "least restrictive environment, appropriate for that individual child." This means the teaching environment should:
- Be designed to meet a child's specific needs and skills
- Minimize restrictions on the child's access to typical learning experiences and interactions
Educating people with autism often includes a combination of one-on-one, small group, and regular classroom instruction.
Individualized Education Program (IEP)
The special education team in your child's school will work with you to design an IEP (also called an individualized education plan) for your child. 2 An IEP is a written document that:
- Lists individualized goals for your child
- Specifies the plan for services your child will receive
- Lists the developmental specialists who will work with your child
Qualifying for Special Education
To qualify for access to special education services, the child must be evaluated by the school system and meet specific criteria as outlined by federal and state guidelines. To learn how to have your child assessed for special services, you can:
- Contact a local school principal or special education coordinator
Consult a parents' organization to get information on therapeutic and educational services and how to get these services for a child. Visit the Resources and Publications: For Patients and Consumers section for a list of these organizations.
- Chang, Y. C., Shire, S. Y., Shih, W., Gelfand, C., & Kasari, C. (2016). Preschool deployment of evidence-based social communication intervention: JASPER in the classroom. Journal of Autism and Developmental Disorders, 46 (6), 2211–2223. Retrieved September 8, 2016, from http://www.ncbi.nlm.nih.gov/pubmed/26936161
Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- HIV and AIDS
- Hypertension
- Mental disorders
- Top 10 causes of death
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- Data collection tools
- Global Health Observatory
- Insights and visualizations
- COVID excess deaths
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Fact sheets /
- Autism – also referred to as autism spectrum disorder ̶ constitutes a diverse group of conditions related to development of the brain.
- About 1 in 100 children has autism.
- Characteristics may be detected in early childhood, but autism is often not diagnosed until much later.
- The abilities and needs of autistic people vary and can evolve over time. While some people with autism can live independently, others have severe disabilities and require life-long care and support.
- Evidence-based psychosocial interventions can improve communication and social skills, with a positive impact on the well-being and quality of life of both autistic people and their caregivers.
- Care for people with autism needs to be accompanied by actions at community and societal levels for greater accessibility, inclusivity and support.
Autism spectrum disorders (ASD) are a diverse group of conditions. They are characterized by some degree of difficulty with social interaction and communication. Other characteristics are atypical patterns of activities and behaviours, such as difficulty with transition from one activity to another, a focus on details and unusual reactions to sensations.
The abilities and needs of autistic people vary and can evolve over time. While some people with autism can live independently, others have severe disabilities and require life-long care and support. Autism often has an impact on education and employment opportunities. In addition, the demands on families providing care and support can be significant. Societal attitudes and the level of support provided by local and national authorities are important factors determining the quality of life of people with autism.
Characteristics of autism may be detected in early childhood, but autism is often not diagnosed until much later.
People with autism often have co-occurring conditions, including epilepsy, depression, anxiety and attention deficit hyperactivity disorder as well as challenging behaviours such as difficulty sleeping and self-injury. The level of intellectual functioning among autistic people varies widely, extending from profound impairment to superior levels.
Epidemiology
It is estimated that worldwide about 1 in 100 children has autism (1) . This estimate represents an average figure, and reported prevalence varies substantially across studies. Some well-controlled studies have, however, reported figures that are substantially higher. The prevalence of autism in many low- and middle-income countries is unknown.
Available scientific evidence suggests that there are probably many factors that make a child more likely to have autism, including environmental and genetic factors.
Extensive research using a variety of different methods and conducted over many years has demonstrated that the measles, mumps and rubella vaccine does not cause autism. Studies that were interpreted as indicating any such link were flawed, and some of the authors had undeclared biases that influenced what they reported about their research (2,3,4) .
Evidence also shows that other childhood vaccines do not increase the risk of autism. Extensive research into the preservative thiomersal and the additive aluminium that are contained in some inactivated vaccines strongly concluded that these constituents in childhood vaccines do not increase the risk of autism.
Assessment and care
A broad range of interventions, from early childhood and across the life span, can optimize the development, health, well-being and quality of life of autistic people. Timely access to early evidence-based psychosocial interventions can improve the ability of autistic children to communicate effectively and interact socially. The monitoring of child development as part of routine maternal and child health care is recommended.
It is important that, once autism has been diagnosed, children, adolescents and adults with autism and their carers are offered relevant information, services, referrals, and practical support, in accordance with their individual and evolving needs and preferences.
The health-care needs of people with autism are complex and require a range of integrated services, that include health promotion, care and rehabilitation. Collaboration between the health sector and other sectors, particularly education, employment and social care, is important.
Interventions for people with autism and other developmental disabilities need to be designed and delivered with the participation of people living with these conditions. Care needs to be accompanied by actions at community and societal levels for greater accessibility, inclusivity and support.
Human rights
All people, including people with autism, have the right to the enjoyment of the highest attainable standard of physical and mental health.
And yet, autistic people are often subject to stigma and discrimination, including unjust deprivation of health care, education and opportunities to engage and participate in their communities.
People with autism have the same health problems as the general population. However, they may, in addition, have specific health-care needs related to autism or other co-occurring conditions. They may be more vulnerable to developing chronic noncommunicable conditions because of behavioural risk factors such as physical inactivity and poor dietary preferences, and are at greater risk of violence, injury and abuse.
People with autism require accessible health services for general health-care needs like the rest of the population, including promotive and preventive services and treatment of acute and chronic illness. Nevertheless, autistic people have higher rates of unmet health-care needs compared with the general population. They are also more vulnerable during humanitarian emergencies. A common barrier is created by health-care providers’ inadequate knowledge and understanding of autism.
WHO resolution on autism spectrum disorders
In May 2014, the Sixty-seventh World Health Assembly adopted a resolution entitled Comprehensive and coordinated efforts for the management of autism spectrum disorders , which was supported by more than 60 countries.
The resolution urges WHO to collaborate with Member States and partner agencies to strengthen national capacities to address ASD and other developmental disabilities.
WHO response
WHO and partners recognize the need to strengthen countries' abilities to promote the optimal health and well-being of all people with autism. WHO's efforts focus on:
- increasing the commitment of governments to taking action to improve the quality of life of people with autism;
- providing guidance on policies and action plans that address autism within the broader framework of health, mental and brain health and disabilities;
- contributing to strengthening the ability of the health workforce to provide appropriate and effective care and promote optimal standards of health and well-being for people with autism; and
- promoting inclusive and enabling environments for people with autism and other developmental disabilities and providing support to their caregivers.
WHO Comprehensive mental health action plan 2013–2030 and World Health Assembly Resolution WHA73.10 for “global actions on epilepsy and other neurological disorders” calls on countries to address the current significant gaps in early detection, care, treatment and rehabilitation for mental and neurodevelopmental conditions, which include autism. It also calls for counties to address the social, economic, educational and inclusion needs of people living with mental and neurological disorders, and their families, and to improve surveillance and relevant research.
1 . Global prevalence of autism: A systematic review update. Zeidan J et al. Autism Research 2022 March.
2. Wakefield's affair: 12 years of uncertainty whereas no link between autism and MMR vaccine has been proved. Maisonneuve H, Floret D. Presse Med. 2012 Sep; French ( https://www.ncbi.nlm.nih.gov/pubmed/22748860 ).
3. Lancet retracts Wakefield’s MMR paper. Dyer C. BMJ 2010;340:c696. 2 February 2010 (https://pubmed.ncbi.nlm.nih.gov/20124366/)
4. Kmietowicz Z. Wakefield is struck off for the “serious and wide-ranging findings against him” BMJ 2010; 340 :c2803 doi:10.1136/bmj.c2803 ( https://www.bmj.com/content/340/bmj.c2803 )
Training for caregivers of children with development delays and disabilities
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Dev Disabil
- v.64(2); 2018
Autism spectrum disorders: identification, education, and treatment
Leslie ann bross.
a University of Kansas
Autism spectrum disorders: identification, education, and treatment , 4th edition, edited by ZagerDianne, CihakDavid F., and Stone-MacDonaldAngi, editors. . New York: Routledge; 2017. ISBN 978-1-138-01569-2
The fourth edition of Autism Spectrum Disorders: Identification, Education, and Treatment provides current and prospective professionals and researchers with a timely update of issues relevant to the field of autism. This new edition describes up-to-date trends and issues critical for the treatment of children, adolescents, and young adults with autism spectrum disorder (ASD). Many of the contributing authors are well recognized and emergent leaders within the field with expertise and knowledge about meeting the complex needs of learners with ASD. The book is organized into three sections. The first section is an overview of the field including changes in diagnostic criteria. The second section is comprised of chapters focused on evidence-based practices for infants up to the elementary/primary school years. The final section focuses on the needs of adolescents and young adults with autism, with specific attention to self-determination and universal design for learning. Readers will likely find this organization useful for finding information specific to their professional and research needs.
The first five chapters provide a thorough historical perspective of the field. The revised clinical diagnostic criteria published in the Diagnostic and Statistical Manual, 5th edition (American Psychological Association, 2013) are described in detail. Updates on assessment tools for accurate diagnosis are helpful to the reader. An overview of legislation and litigation issues related to individuals with ASD describes relevant law and example court cases. In addition, a summary of possible service delivery models is provided with substantial practical details for professionals. The global perspective chapter is a particularly welcomed addition from previous editions because of the overview of autism treatments described around the world.
Middle chapters provide descriptions of evidence-based practices to inform readers what intervention programs should include for children with autism from birth to elementary/primary school years. Specific interventions are described with applicable examples supported by current empirical research. The chapter on communication and language development includes the most current research on language and communication programming, including augmentative and alternative communication systems such as picture exchange communication system, speech generating devices and functional communication training. Professionals will find this content especially useful given that communication programming tends to be a very high priority for intervention programming. The chapter on managing appropriate behaviors provides a valuable overview of data collection procedures and behavior interventions grounded in principles of behavior consistent with applied behavior analysis. A new chapter on academic skills interventions rounds this section along with a chapter on social interaction competence.
The final section of the text includes chapters focused on transition to adulthood for adolescents and young adults with ASD. The importance of self-determination, student involvement in transition planning, and the recently proposed framework called universal design for transition is discussed in detail. Interdisciplinary collaboration is also a focus, along with current research and practice related to positive behavior supports and integrated employment. Professionals working with middle and high school students with ASD will particularly benefit from the overview of evidence-based practices in transition planning to address the persistently poor postsecondary outcomes of individuals with ASD.
Overall, the book will prove an excellent resource for professionals charged with daily service and support of learners with ASD, and psychiatric and other related medical professionals will find it a useful reference for their personal library. Researchers and teacher educators also will find this revision replete with current knowledge and evidence regarding demonstrably effective interventions. It is a highly recommended resource for any professional who will provide services to learners with autism.
NASET.org Home Page
Exceptional teachers teaching exceptional children.
- Overview of NASET
- NASET Leadership
- Directors' Message
- Books by the Executive Directors
- Mission Statement
- NASET Apps for iPhone and iPad
- NASET Store
- NASET Sponsors
- Marketing Opportunities
- Contact NASET
- Renew Your Membership
- Membership Benefits
- Frequently Asked Questions
- Membership Categories
- School / District Membership Information
- Gift Membership
- Membership Benefit for Professors Only
- NASET's Privacy Policy
- Forgot Your User Name or Password?
- Contact Membership Department
- Resources for Special Education Teachers
- Advocacy (Board Certification for Advocacy in Special Education) BCASE
- Board Certification in Special Education
- Inclusion - Board Certification in Inclusion in Special Education (BCISE) Program
- Paraprofessional Skills Preparation Program - PSPP
- Professional Development Program (PDP) Free to NASET Members
- Courses - Professional Development Courses (Free With Membership)
- Forms, Tables, Checklists, and Procedures for Special Education Teachers
- Video and Power Point Library
- IEP Development
- Exceptional Students and Disability Information
- Special Education and the Law
- Transition Services
- Literacy - Teaching Literacy in English to K-5 English Learners
- Facebook - Special Education Teacher Group
- NASET Sponsor's Products and Services
- ADHD Series
- Assessment in Special Education Series
- Autism Spectrum Disorders Series
- Back to School - Special Review
- Bullying of Children
- Classroom Management Series
- Diagnosis of Students with Disabilities and Disorders Series
- Treatment of Disabilities and Disorders for Students Receiving Special Education and Related Services
- Discipline of Students in Special Education Series
- Early Intervention Series
- Genetics in Special Education Series
- How To Series
- Inclusion Series
- IEP Components
- JAASEP - Research Based Journal in Special Education
- Lesser Known Disorders
- NASET NEWS ALERTS
- NASET Q & A Corner
- Parent Teacher Conference Handouts
- The Practical Teacher
- Resolving Disputes with Parents Series
- RTI Roundtable
- Severe Disabilities Series
- Special Educator e-Journal - Latest and Archived Issues
- Week in Review
- Working with Paraprofessionals in Your School
- Author Guidelines for Submission of Manuscripts & Articles to NASET
- SCHOOLS of EXCELLENCE
- Exceptional Charter School in Special Education
- Outstanding Special Education Teacher Award
- Board Certification Programs
- Employers - Job Posting Information
- Latest Job Listings
- Professional Development Program (PDP)
- Employers-Post a Job on NASET
- PDP - Professional Development Courses
- Board Certification in Special Education (BCSE)
- Board Certification in IEP Development (BCIEP)
- NASET Continuing Education/Professional Development Courses
- HONOR SOCIETY - Omega Gamma Chi
- Other Resources for Special Education Teaching Positions
- Highly Qualified Teachers
- Special Education Career Advice
- Special Education Career Fact Sheets
- FAQs for Special Education Teachers
- Special Education Teacher Salaries by State
- State Licensure for Special Education Teachers
Autism Spectrum Disorders
Autism spectrum disorders (pervasive developmental disorders).
Not until the middle of the twentieth century was there a name for a disorder that now appears to affect an estimated one of every five hundred children, a disorder that causes disruption in families and unfulfilled lives for many children. In 1943 Dr. Leo Kanner of the Johns Hopkins Hospital studied a group of 11 children and introduced the label early infantile autism into the English language. At the same time a German scientist, Dr. Hans Asperger, described a milder form of the disorder that became known as Asperger syndrome. Thus these two disorders were described and are today listed in the Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR (fourth edition, text revision) 1 as two of the five pervasive developmental disorders (PDD), more often referred to today as autism spectrum disorders (ASD). All these disorders are characterized by varying degrees of impairment in communication skills, social interactions, and restricted, repetitive and stereotyped patterns of behavior.
The autism spectrum disorders can often be reliably detected by the age of 3 years, and in some cases as early as 18 months. 2 Studies suggest that many children eventually may be accurately identified by the age of 1 year or even younger. The appearance of any of the warning signs of ASD is reason to have a child evaluated by a professional specializing in these disorders.
Parents are usually the first to notice unusual behaviors in their child. In some cases, the baby seemed "different" from birth, unresponsive to people or focusing intently on one item for long periods of time. The first signs of an ASD can also appear in children who seem to have been developing normally. When an engaging, babbling toddler suddenly becomes silent, withdrawn, self-abusive, or indifferent to social overtures, something is wrong. Research has shown that parents are usually correct about noticing developmental problems, although they may not realize the specific nature or degree of the problem.
The pervasive developmental disorders, or autism spectrum disorders, range from a severe form, called autistic disorder, to a milder form, Asperger syndrome. If a child has symptoms of either of these disorders, but does not meet the specific criteria for either, the diagnosis is called pervasive developmental disorder not otherwise specified (PDD-NOS). Other rare, very severe disorders that are included in the autism spectrum disorders are Rett syndrome and childhood disintegrative disorder. This brochure will focus on classic autism, PDD-NOS, and Asperger syndrome, with brief descriptions of Rett syndrome and childhood disintegrative disorder on the following page.
Rare Autism Spectrum Disorders
- Rett Syndrome
Rett syndrome is relatively rare, affecting almost exclusively females, one out of 10,000 to 15,000. After a period of normal development, sometime between 6 and 18 months, autism-like symptoms begin to appear. The little girl's mental and social development regresses—she no longer responds to her parents and pulls away from any social contact. If she has been talking, she stops; she cannot control her feet; she wrings her hands. Some of the problems associated with Rett syndrome can be treated. Physical, occupational, and speech therapy can help with problems of coordination, movement, and speech. Scientists sponsored by the National Institute of Child Health and Human Development have discovered that a mutation in the sequence of a single gene can cause Rett syndrome. This discovery may help doctors slow or stop the progress of the syndrome. It may also lead to methods of screening for Rett syndrome, thus enabling doctors to start treating these children much sooner, and improving the quality of life these children experience. *
Childhood Disintegrative Disorder
Very few children who have an autism spectrum disorder (ASD) diagnosis meet the criteria for childhood disintegrative disorder (CDD). An estimate based on four surveys of ASD found fewer than two children per 100,000 with ASD could be classified as having CDD. This suggests that CDD is a very rare form of ASD. It has a strong male preponderance. ** Symptoms may appear by age 2, but the average age of onset is between 3 and 4 years. Until this time, the child has age-appropriate skills in communication and social relationships. The long period of normal development before regression helps differentiate CDD from Rett syndrome.
The loss of such skills as vocabulary are more dramatic in CDD than they are in classical autism. The diagnosis requires extensive and pronounced losses involving motor, language, and social skills. *** CDD is also accompanied by loss of bowel and bladder control and oftentimes seizures and a very low IQ. *Rett syndrome. NIH Publication No. 01-4960. Rockville, MD: National Institute of Child Health and Human Development, 2001. Available at http://www.nichd.nih.gov/publications/pubskey.cfm?from=autism
**Frombonne E. Prevalence of childhood disintegrative disorder. Autism, 2002; 6(2): 149-157. ***Volkmar RM and Rutter M. Childhood disintegrative disorder: Results of the DSM-IV autism field trial. Journal of the American Academy of Child and Adolescent Psychiatry, 1995; 34: 1092-1095.
What Are the Autism Spectrum Disorders?
The autism spectrum disorders are more common in the pediatric population than are some better known disorders such as diabetes, spinal bifida, or Down syndrome. 2 Prevalence studies have been done in several states and also in the United Kingdom, Europe, and Asia. Prevalence estimates range from 2 to 6 per 1,000 children. This wide range of prevalence points to a need for earlier and more accurate screening for the symptoms of ASD. The earlier the disorder is diagnosed, the sooner the child can be helped through treatment interventions. Pediatricians, family physicians, daycare providers, professionals, and parents may initially dismiss signs of ASD, optimistically thinking the child is just a little slow and will "catch up." Although early intervention has a dramatic impact on reducing symptoms and increasing a child's ability to grow and learn new skills, it is estimated that only 50 percent of children are diagnosed before kindergarten .
All children with ASD demonstrate deficits in 1) social interaction, 2) verbal and nonverbal communication, and 3) repetitive behaviors or interests. In addition, they will often have unusual responses to sensory experiences, such as certain sounds or the way objects look. Each of these symptoms runs the gamut from mild to severe. They will present in each individual child differently. For instance, a child may have little trouble learning to read but exhibit extremely poor social interaction. Each child will display communication, social, and behavioral patterns that are individual but fit into the overall diagnosis of ASD.
Children with ASD do not follow the typical patterns of child development. In some children, hints of future problems may be apparent from birth. In most cases, the problems in communication and social skills become more noticeable as the child lags further behind other children the same age. Some other children start off well enough. Oftentimes between 12 and 36 months old, the differences in the way they react to people and other unusual behaviors become apparent. Some parents report the change as being sudden, and that their children start to reject people, act strangely, and lose language and social skills they had previously acquired. In other cases, there is a plateau, or leveling, of progress so that the difference between the child with autism and other children the same age becomes more noticeable.
ASD is defined by a certain set of behaviors that can range from the very mild to the severe. The following possible indicators of ASD were identified on the Public Health Training Network Webcast, Autism Among Us. 3
Possible Indicators of Autism Spectrum Disorders
- Does not babble, point, or make meaningful gestures by 1 year of age
- Does not speak one word by 16 months
- Does not combine two words by 2 years
- Does not respond to name
- Loses language or social skills
Some Other Indicators
- Poor eye contact
- Doesn't seem to know how to play with toys
- Excessively lines up toys or other objects
- Is attached to one particular toy or object
- Doesn't smile
- At times seems to be hearing impaired
Social Symptoms
From the start, typically developing infants are social beings. Early in life, they gaze at people, turn toward voices, grasp a finger, and even smile.
In contrast, most children with ASD seem to have tremendous difficulty learning to engage in the give-and-take of everyday human interaction. Even in the first few months of life, many do not interact and they avoid eye contact. They seem indifferent to other people, and often seem to prefer being alone. They may resist attention or passively accept hugs and cuddling. Later, they seldom seek comfort or respond to parents' displays of anger or affection in a typical way. Research has suggested that although children with ASD are attached to their parents, their expression of this attachment is unusual and difficult to "read." To parents, it may seem as if their child is not attached at all. Parents who looked forward to the joys of cuddling, teaching, and playing with their child may feel crushed by this lack of the expected and typical attachment behavior.
Children with ASD also are slower in learning to interpret what others are thinking and feeling. Subtle social cues—whether a smile, a wink, or a grimace—may have little meaning. To a child who misses these cues, "Come here" always means the same thing, whether the speaker is smiling and extending her arms for a hug or frowning and planting her fists on her hips. Without the ability to interpret gestures and facial expressions, the social world may seem bewildering. To compound the problem, people with ASD have difficulty seeing things from another person's perspective. Most 5-year-olds understand that other people have different information, feelings, and goals than they have. A person with ASD may lack such understanding. This inability leaves them unable to predict or understand other people's actions.
Although not universal, it is common for people with ASD also to have difficulty regulating their emotions. This can take the form of "immature" behavior such as crying in class or verbal outbursts that seem inappropriate to those around them. The individual with ASD might also be disruptive and physically aggressive at times, making social relationships still more difficult. They have a tendency to "lose control," particularly when they're in a strange or overwhelming environment, or when angry and frustrated. They may at times break things, attack others, or hurt themselves. In their frustration, some bang their heads, pull their hair, or bite their arms.
Communication Difficulties
By age 3, most children have passed predictable milestones on the path to learning language; one of the earliest is babbling. By the first birthday, a typical toddler says words, turns when he hears his name, points when he wants a toy, and when offered something distasteful, makes it clear that the answer is "no." Some children diagnosed with ASD remain mute throughout their lives. Some infants who later show signs of ASD coo and babble during the first few months of life, but they soon stop. Others may be delayed, developing language as late as age 5 to 9. Some children may learn to use communication systems such as pictures or sign language. Those who do speak often use language in unusual ways. They seem unable to combine words into meaningful sentences. Some speak only single words, while others repeat the same phrase over and over. Some ASD children parrot what they hear, a condition called echolalia . Although many children with no ASD go through a stage where they repeat what they hear, it normally passes by the time they are 3. Some children only mildly affected may exhibit slight delays in language, or even seem to have precocious language and unusually large vocabularies, but have great difficulty in sustaining a conversation. The "give and take" of normal conversation is hard for them, although they often carry on a monologue on a favorite subject, giving no one else an opportunity to comment. Another difficulty is often the inability to understand body language, tone of voice, or "phrases of speech." They might interpret a sarcastic expression such as "Oh, that's just great" as meaning it really IS great. While it can be hard to understand what ASD children are saying, their body language is also difficult to understand. Facial expressions, movements, and gestures rarely match what they are saying. Also, their tone of voice fails to reflect their feelings. A high-pitched, sing-song, or flat, robot-like voice is common. Some children with relatively good language skills speak like little adults, failing to pick up on the "kid-speak" that is common in their peers. Without meaningful gestures or the language to ask for things, people with ASD are at a loss to let others know what they need. As a result, they may simply scream or grab what they want. Until they are taught better ways to express their needs, ASD children do whatever they can to get through to others. As people with ASD grow up, they can become increasingly aware of their difficulties in understanding others and in being understood. As a result they may become anxious or depressed.
Repetitive Behaviors
Although children with ASD usually appear physically normal and have good muscle control, odd repetitive motions may set them off from other children. These behaviors might be extreme and highly apparent or more subtle. Some children and older individuals spend a lot of time repeatedly flapping their arms or walking on their toes. Some suddenly freeze in position.
As children, they might spend hours lining up their cars and trains in a certain way, rather than using them for pretend play. If someone accidentally moves one of the toys, the child may be tremendously upset. ASD children need, and demand, absolute consistency in their environment. A slight change in any routine—in mealtimes, dressing, taking a bath, going to school at a certain time and by the same route—can be extremely disturbing. Perhaps order and sameness lend some stability in a world of confusion.
Repetitive behavior sometimes takes the form of a persistent, intense preoccupation. For example, the child might be obsessed with learning all about vacuum cleaners, train schedules, or lighthouses. Often there is great interest in numbers, symbols, or science topics.
Problems That May Accompany ASD
Sensory problems. When children's perceptions are accurate, they can learn from what they see, feel, or hear. On the other hand, if sensory information is faulty, the child's experiences of the world can be confusing. Many ASD children are highly attuned or even painfully sensitive to certain sounds, textures, tastes, and smells. Some children find the feel of clothes touching their skin almost unbearable. Some sounds—a vacuum cleaner, a ringing telephone, a sudden storm, even the sound of waves lapping the shoreline—will cause these children to cover their ears and scream. In ASD, the brain seems unable to balance the senses appropriately. Some ASD children are oblivious to extreme cold or pain. An ASD child may fall and break an arm, yet never cry. Another may bash his head against a wall and not wince, but a light touch may make the child scream with alarm.
Intellectual Disability. Many children with ASD have some degree of mental impairment. When tested, some areas of ability may be normal, while others may be especially weak. For example, a child with ASD may do well on the parts of the test that measure visual skills but earn low scores on the language subtests.
Seizures. One in four children with ASD develops seizures, often starting either in early childhood or adolescence. 4 Seizures, caused by abnormal electrical activity in the brain, can produce a temporary loss of consciousness (a "blackout"), a body convulsion, unusual movements, or staring spells. Sometimes a contributing factor is a lack of sleep or a high fever. An EEG (electroencephalogram—recording of the electric currents developed in the brain by means of electrodes applied to the scalp) can help confirm the seizure's presence. In most cases, seizures can be controlled by a number of medicines called "anticonvulsants." The dosage of the medication is adjusted carefully so that the least possible amount of medication will be used to be effective.
Fragile X syndrome. This disorder is the most common inherited form of mental retardation. It was so named because one part of the X chromosome has a defective piece that appears pinched and fragile when under a microscope. Fragile X syndrome affects about two to five percent of people with ASD. It is important to have a child with ASD checked for Fragile X, especially if the parents are considering having another child. For an unknown reason, if a child with ASD also has Fragile X, there is a one-in-two chance that boys born to the same parents will have the syndrome. 5 Other members of the family who may be contemplating having a child may also wish to be checked for the syndrome.
Tuberous Sclerosis. Tuberous sclerosis is a rare genetic disorder that causes benign tumors to grow in the brain as well as in other vital organs. It has a consistently strong association with ASD. One to 4 percent of people with ASD also have tuberous sclerosis. 6
The Diagnosis of Autism Spectrum Disorders
Although there are many concerns about labeling a young child with an ASD, the earlier the diagnosis of ASD is made, the earlier needed interventions can begin. Evidence over the last 15 years indicates that intensive early intervention in optimal educational settings for at least 2 years during the preschool years results in improved outcomes in most young children with ASD. 2 In evaluating a child, clinicians rely on behavioral characteristics to make a diagnosis. Some of the characteristic behaviors of ASD may be apparent in the first few months of a child's life, or they may appear at any time during the early years. For the diagnosis, problems in at least one of the areas of communication, socialization, or restricted behavior must be present before the age of 3. The diagnosis requires a two-stage process. The first stage involves developmental screening during "well child" check-ups; the second stage entails a comprehensive evaluation by a multidisciplinary team. 7 ;
A "well child" check-up should include a developmental screening test. If your child's pediatrician does not routinely check your child with such a test, ask that it be done. Your own observations and concerns about your child's development will be essential in helping to screen your child.7 Reviewing family videotapes, photos, and baby albums can help parents remember when each behavior was first noticed and when the child reached certain developmental milestones. Several screening instruments have been developed to quickly gather information about a child's social and communicative development within medical settings. Among them are the Checklist of Autism in Toddlers (CHAT),8 the modified Checklist for Autism in Toddlers (M-CHAT),9 the Screening Tool for Autism in Two-Year-Olds (STAT),10 and the Social Communication Questionnaire (SCQ)11 (for children 4 years of age and older). Some screening instruments rely solely on parent responses to a questionnaire, and some rely on a combination of parent report and observation. Key items on these instruments that appear to differentiate children with autism from other groups before the age of 2 include pointing and pretend play. Screening instruments do not provide individual diagnosis but serve to assess the need for referral for possible diagnosis of ASD. These screening methods may not identify children with mild ASD, such as those with high-functioning autism or Asperger syndrome. During the last few years, screening instruments have been devised to screen for Asperger syndrome and higher functioning autism. The Autism Spectrum Screening Questionnaire (ASSQ),12 the Australian Scale for Asperger's Syndrome,13 and the most recent, the Childhood Asperger Syndrome Test (CAST),14 are some of the instruments that are reliable for identification of school-age children with Asperger syndrome or higher functioning autism. These tools concentrate on social and behavioral impairments in children without significant language delay. If, following the screening process or during a routine "well child" check-up, your child's doctor sees any of the possible indicators of ASD, further evaluation is indicated.
Comprehensive Diagnostic Evaluation The second stage of diagnosis must be comprehensive in order to accurately rule in or rule out an ASD or other developmental problem. This evaluation may be done by a multidisciplinary team that includes a psychologist, a neurologist, a psychiatrist, a speech therapist, or other professionals who diagnose children with ASD. Because ASDs are complex disorders and may involve other neurological or genetic problems, a comprehensive evaluation should entail neurologic and genetic assessment, along with in-depth cognitive and language testing. 7 In addition, measures developed specifically for diagnosing autism are often used. These include the Autism Diagnosis Interview-Revised (ADI-R) 15 and the Autism Diagnostic Observation Schedule (ADOS-G). 16 The ADI-R is a structured interview that contains over 100 items and is conducted with a caregiver. It consists of four main factors—the child's communication, social interaction, repetitive behaviors, and age-of-onset symptoms. The ADOS-G is an observational measure used to "press" for socio-communicative behaviors that are often delayed, abnormal, or absent in children with ASD. Still another instrument often used by professionals is the Childhood Autism Rating Scale (CARS). 17 It aids in evaluating the child's body movements, adaptation to change, listening response, verbal communication, and relationship to people. It is suitable for use with children over 2 years of age. The examiner observes the child and also obtains relevant information from the parents. The child's behavior is rated on a scale based on deviation from the typical behavior of children of the same age. Two other tests that should be used to assess any child with a developmental delay are a formal audiologic hearing evaluation and a lead screening. Although some hearing loss can co-occur with ASD, some children with ASD may be incorrectly thought to have such a loss. In addition, if the child has suffered from an ear infection, transient hearing loss can occur. Lead screening is essential for children who remain for a long period of time in the oral-motor stage in which they put any and everything into their mouths. Children with an autistic disorder usually have elevated blood lead levels. 7
Available Aids
When your child has been evaluated and diagnosed with an autism spectrum disorder, you may feel inadequate to help your child develop to the fullest extent of his or her ability. As you begin to look at treatment options and at the types of aid available for a child with a disability, you will find out that there is help for you. It is going to be difficult to learn and remember everything you need to know about the resources that will be most helpful. Write down everything. If you keep a notebook, you will have a foolproof method of recalling information. Keep a record of the doctors' reports and the evaluation your child has been given so that his or her eligibility for special programs will be documented. Learn everything you can about special programs for your child; the more you know, the more effectively you can advocate. For every child eligible for special programs, each state guarantees special education and related services. The Individuals with Disabilities Education Act (IDEA) is a Federally mandated program that assures a free and appropriate public education for children with diagnosed learning deficits. Usually children are placed in public schools and the school district pays for all necessary services. These will include, as needed, services by a speech therapist, occupational therapist, school psychologist, social worker, school nurse, or aide. By law, the public schools must prepare and carry out a set of instruction goals, or specific skills, for every child in a special education program. The list of skills is known as the child's Individualized Education Program (IEP). The IEP is an agreement between the school and the family on the child's goals. When your child's IEP is developed, you will be asked to attend the meeting. There will be several people at this meeting, including a special education professional, a representative of the public schools who is knowledgeable about the program, other individuals invited by the school or by you (you may want to bring a relative, a child care provider, or a supportive close friend who knows your child well). Parents play an important part in creating the program, as they know their child and his or her needs best. Once your child's IEP is developed, a meeting is scheduled once a year to review your child's progress and to make any alterations to reflect his or her changing needs. If your child is under 3 years of age and has special needs, he or she should be eligible for an early intervention program; this program is available in every state. Each state decides which agency will be the lead agency in the early intervention program. The early intervention services are provided by workers qualified to care for toddlers with disabilities and are usually in the child's home or a place familiar to the child. The services provided are written into an Individualized Family Service Plan (IFSP) that is reviewed at least once every 6 months. The plan will describe services that will be provided to the child, but will also describe services for parents to help them in daily activities with their child and for siblings to help them adjust to having a brother or sister with ASD. There is a list of resources at the back of the brochure that will be helpful to you as you look for programs for your child.
Treatment Options
There is no single best treatment package for all children with ASD. One point that most professionals agree on is that early intervention is important; another is that most individuals with ASD respond well to highly structured, specialized programs. Before you make decisions on your child's treatment, you will want to gather information about the various options available. Learn as much as you can, look at all the options, and make your decision on your child's treatment based on your child's needs. You may want to visit public schools in your area to see the type of program they offer to special needs children. Guidelines used by the Autism Society of America include the following questions parents can ask about potential treatments:
- Will the treatment result in harm to my child?
- How will failure of the treatment affect my child and family?
- Has the treatment been validated scientifically?
- Are there assessment procedures specified?
- How will the treatment be integrated into my child's current program?
Do not become so infatuated with a given treatment that functional curriculum, vocational life, and social skills are ignored.
The National Institute of Mental Health suggests a list of questions parents can ask when planning for their child:
- How successful has the program been for other children?
- How many children have gone on to placement in a regular school and how have they performed?
- Do staff members have training and experience in working with children and adolescents with autism?
- How are activities planned and organized?
- Are there predictable daily schedules and routines?
- How much individual attention will my child receive?
- How is progress measured?
- Will my child's behavior be closely observed and recorded?
- Will my child be given tasks and rewards that are personally motivating?
- Is the environment designed to minimize distractions?
- Will the program prepare me to continue the therapy at home?
- What is the cost, time commitment, and location of the program?
Among the many methods available for treatment and education of people with autism, applied behavior analysis (ABA) has become widely accepted as an effective treatment. Mental Health: A Report of the Surgeon General states, "Thirty years of research demonstrated the efficacy of applied behavioral methods in reducing inappropriate behavior and in increasing communication, learning, and appropriate social behavior." 18 The basic research done by Ivar Lovaas and his colleagues at the University of California, Los Angeles, calling for an intensive, one-on-one child-professional interaction for 40 hours a week, laid a foundation for other educators and researchers in the search for further effective early interventions to help those with ASD attain their potential. The goal of behavioral management is to reinforce desirable behaviors and reduce undesirable ones. 19 , 20 An effective treatment program will build on the child's interests, offer a predictable schedule, teach tasks as a series of simple steps, actively engage the child's attention in highly structured activities, and provide regular reinforcement of behavior. Parental involvement has emerged as a major factor in treatment success. Parents work with professionals and therapists to identify the behaviors to be changed and the skills to be taught. Recognizing that parents are the child's earliest professionals, more programs are beginning to train parents to continue the therapy at home. As soon as a child's disability has been identified, instruction should begin. Effective programs will teach early communication and social interaction skills. In children younger than 3 years, appropriate interventions usually take place in the home or a child care center. These interventions target specific deficits in learning, language, imitation, attention, motivation, compliance, and initiative of interaction. Included are behavioral methods, communication, occupational and physical therapy along with social play interventions. Often the day will begin with a physical activity to help develop coordination and body awareness; children string beads, piece puzzles together, paint, and participate in other motor skills activities. At snack time the professional encourages social interaction and models how to use language to ask for more juice. The children learn by doing. Working with the children are students, behavioral therapists, and parents who have received extensive training. In teaching the children, positive reinforcement is used. 21 Children older than 3 years usually have school-based, individualized, special education. The child may be in a segregated class with other autistic children or in an integrated class with children without disabilities for at least part of the day. Different localities may use differing methods but all should provide a structure that will help the children learn social skills and functional communication. In these programs, professionals often involve the parents, giving useful advice in how to help their child use the skills or behaviors learned at school when they are at home. 22 In elementary school, the child should receive help in any skill area that is delayed and, at the same time, be encouraged to grow in his or her areas of strength. Ideally, the curriculum should be adapted to the individual child's needs. Many schools today have an inclusion program in which the child is in a regular classroom for most of the day, with special instruction for a part of the day. This instruction should include such skills as learning how to act in social situations and in making friends. Although higher-functioning children may be able to handle academic work, they too need help to organize tasks and avoid distractions. During middle and high school years, instruction will begin to address such practical matters as work, community living, and recreational activities. This should include work experience, using public transportation, and learning skills that will be important in community living. 23 All through your child's school years, you will want to be an active participant in his or her education program. Collaboration between parents and educators is essential in evaluating your child's progress.
The Adolescent Years
Adolescence is a time of stress and confusion; and it is no less so for teenagers with autism. Like all children, they need help in dealing with their budding sexuality. While some behaviors improve during the teenage years, some get worse. Increased autistic or aggressive behavior may be one way some teens express their newfound tension and confusion.
The teenage years are also a time when children become more socially sensitive. At the age that most teenagers are concerned with acne, popularity, grades, and dates, teens with autism may become painfully aware that they are different from their peers. They may notice that they lack friends. And unlike their schoolmates, they aren't dating or planning for a career. For some, the sadness that comes with such realization motivates them to learn new behaviors and acquire better social skills.
Dietary and Other Interventions
In an effort to do everything possible to help their children, many parents continually seek new treatments. Some treatments are developed by reputable therapists or by parents of a child with ASD. Although an unproven treatment may help one child, it may not prove beneficial to another. To be accepted as a proven treatment, the treatment should undergo clinical trials, preferably randomized, double-blind trials, that would allow for a comparison between treatment and no treatment. Following are some of the interventions that have been reported to have been helpful to some children but whose efficacy or safety has not been proven.
Dietary interventions are based on the idea that 1) food allergies cause symptoms of autism, and 2) an insufficiency of a specific vitamin or mineral may cause some autistic symptoms. If parents decide to try for a given period of time a special diet, they should be sure that the child's nutritional status is measured carefully.
A diet that some parents have found was helpful to their autistic child is a gluten-free, casein-free diet. Gluten is a casein-like substance that is found in the seeds of various cereal plants—wheat, oat, rye, and barley. Casein is the principal protein in milk. Since gluten and milk are found in many of the foods we eat, following a gluten-free, casein-free diet is difficult.
A supplement that some parents feel is beneficial for an autistic child is Vitamin B6, taken with magnesium (which makes the vitamin effective). The result of research studies is mixed; some children respond positively, some negatively, some not at all or very little. 4
In the search for treatment for autism, there has been discussion in the last few years about the use of secretin, a substance approved by the Food and Drug Administration (FDA) for a single dose normally given to aid in diagnosis of a gastrointestinal problem. Anecdotal reports have shown improvement in autism symptoms, including sleep patterns, eye contact, language skills, and alertness. Several clinical trials conducted in the last few years have found no significant improvements in symptoms between patients who received secretin and those who received a placebo. 24
Medication Used In Treatment
Medications are often used to treat behavioral problems, such as aggression, self-injurious behavior, and severe tantrums, that keep the person with ASD from functioning more effectively at home or school. The medications used are those that have been developed to treat similar symptoms in other disorders. Many of these medications are prescribed "off-label." This means they have not been officially approved by the FDA for use in children, but the doctor prescribes the medications if he or she feels they are appropriate for your child. Further research needs to be done to ensure not only the efficacy but the safety of psychotropic agents used in the treatment of children and adolescents.
A child with ASD may not respond in the same way to medications as typically developing children. It is important that parents work with a doctor who has experience with children with autism. A child should be monitored closely while taking a medication. The doctor will prescribe the lowest dose possible to be effective. Ask the doctor about any side effects the medication may have and keep a record of how your child responds to the medication. It will be helpful to read the "patient insert" that comes with your child's medication. Some people keep the patient inserts in a small notebook to be used as a reference. This is most useful when several medications are prescribed.
Anxiety and depression. The selective serotonin reuptake inhibitors (SSRI's) are the medications most often prescribed for symptoms of anxiety, depression, and/or obsessive-compulsive disorder (OCD). Only one of the SSRI's, fluoxetine, (Prozac®) has been approved by the FDA for both OCD and depression in children age 7 and older. Three that have been approved for OCD are fluvoxamine (Luvox®), age 8 and older; sertraline (Zoloft®), age 6 and older; and clomipramine (Anafranil®), age 10 and older.4 Treatment with these medications can be associated with decreased frequency of repetitive, ritualistic behavior and improvements in eye contact and social contacts. The FDA is studying and analyzing data to better understand how to use the SSRI's safely, effectively, and at the lowest dose possible.
Behavioral problems . Antipsychotic medications have been used to treat severe behavioral problems. These medications work by reducing the activity in the brain of the neurotransmitter dopamine. Among the older, typical antipsychotics, such as haloperidol (Haldol®), thioridazine, fluphenazine, and chlorpromazine, haloperidol was found in more than one study to be more effective than a placebo in treating serious behavioral problems.25 However, haloperidol, while helpful for reducing symptoms of aggression, can also have adverse side effects, such as sedation, muscle stiffness, and abnormal movements. Placebo-controlled studies of the newer "atypical" antipsychotics are being conducted on children with autism. The first such study, conducted by the NIMH-supported Research Units on Pediatric Psychopharmacology (RUPP) Autism Network, was on risperidone (Risperdal®).26 Results of the 8-week study were reported in 2002 and showed that risperidone was effective and well tolerated for the treatment of severe behavioral problems in children with autism. The most common side effects were increased appetite, weight gain and sedation. Further long-term studies are needed to determine any long-term side effects. Other atypical antipsychotics that have been studied recently with encouraging results are olanzapine (Zyprexa®) and ziprasidone (Geodon®). Ziprasidone has not been associated with significant weight gain.
Seizures. Seizures are found in one in four persons with ASD, most often in those who have low IQ or are mute. They are treated with one or more of the anticonvulsants. These include such medications as carbamazepine (Tegretol®), lamotrigine (Lamictal®), topiramate (Topamax®), and valproic acid (Depakote®). The level of the medication in the blood should be monitored carefully and adjusted so that the least amount possible is used to be effective. Although medication usually reduces the number of seizures, it cannot always eliminate them.
Inattention and hyperactivity. Stimulant medications such as methylphenidate (Ritalin®), used safely and effectively in persons with attention deficit hyperactivity disorder, have also been prescribed for children with autism. These medications may decrease impulsivity and hyperactivity in some children, especially those higher functioning children.
Several other medications have been used to treat ASD symptoms; among them are other antidepressants, naltrexone, lithium, and some of the benzodiazepines such as diazepam (Valium®) and lorazepam (Ativan®). The safety and efficacy of these medications in children with autism has not been proven. Since people may respond differently to different medications, your child's unique history and behavior will help your doctor decide which medication might be most beneficial.
Adults With an Autism Spectrum Disorder
Some adults with ASD, especially those with high-functioning autism or with Asperger syndrome, are able to work successfully in mainstream jobs. Nevertheless, communication and social problems often cause difficulties in many areas of life. They will continue to need encouragement and moral support in their struggle for an independent life.
Many others with ASD are capable of employment in sheltered workshops under the supervision of managers trained in working with persons with disabilities. A nurturing environment at home, at school, and later in job training and at work, helps persons with ASD continue to learn and to develop throughout their lives.
The public schools' responsibility for providing services ends when the person with ASD reaches the age of 22. The family is then faced with the challenge of finding living arrangements and employment to match the particular needs of their adult child, as well as the programs and facilities that can provide support services to achieve these goals. Long before your child finishes school, you will want to search for the best programs and facilities for your young adult. If you know other parents of ASD adults, ask them about the services available in your community. If your community has little to offer, serve as an advocate for your child and work toward the goal of improved employment services. Research the resources listed in the back of this brochure to learn as much as possible about the help your child is eligible to receive as an adult.
Living Arrangements for the Adult with an Autism Spectrum Disorder
Independent living. Some adults with ASD are able to live entirely on their own. Others can live semi-independently in their own home or apartment if they have assistance with solving major problems, such as personal finances or dealing with the government agencies that provide services to persons with disabilities. This assistance can be provided by family, a professional agency, or another type of provider.
Living at home. Government funds are available for families that choose to have their adult child with ASD live at home. These programs include Supplemental Security Income (SSI), Social Security Disability Insurance (SSDI), Medicaid waivers, and others. Information about these programs is available from the Social Security Administration (SSA). An appointment with a local SSA office is a good first step to take in understanding the programs for which the young adult is eligible.
Foster homes and skill-development homes. Some families open their homes to provide long-term care to unrelated adults with disabilities. If the home teaches self-care and housekeeping skills and arranges leisure activities, it is called a "skill-development" home.
Supervised group living. Persons with disabilities frequently live in group homes or apartments staffed by professionals who help the individuals with basic needs. These often include meal preparation, housekeeping, and personal care needs. Higher functioning persons may be able to live in a home or apartment where staff only visit a few times a week. These persons generally prepare their own meals, go to work, and conduct other daily activities on their own.
Institutions. Although the trend in recent decades has been to avoid placing persons with disabilities into long-term-care institutions, this alternative is still available for persons with ASD who need intensive, constant supervision. Unlike many of the institutions years ago, today's facilities view residents as individuals with human needs and offer opportunities for recreation and simple but meaningful work.
Research into Causes and Treatment of Autism Spectrum Disorders
Research into the causes, the diagnosis, and the treatment of autism spectrum disorders has advanced in tandem. With new well-researched standardized diagnostic tools, ASD can be diagnosed at an early age. And with early diagnosis, the treatments found to be beneficial in recent years can be used to help the child with ASD develop to his or her greatest potential.
In the past few years, there has been public interest in a theory that suggested a link between the use of thimerosal, a mercury-based preservative used in the measles-mumps-rubella (MMR) vaccine, and autism. Although mercury is no longer found in childhood vaccines in the United States, some parents still have concerns about vaccinations. Many well-done, large-scale studies have now been done that have failed to show a link between thimerosal and autism. A panel from the Institute of Medicine is now examining these studies, including a large Danish study that concluded that there was no causal relationship between childhood vaccination using thimerosal-containing vaccines and the development of an autism spectrum disorder, 27 and a U.S. study looking at exposure to mercury, lead, and other heavy metals.
Research on the Biologic Basis of ASD
Because of its relative inaccessibility, scientists have only recently been able to study the brain systematically. But with the emergence of new brain imaging tools—computerized tomography (CT), positron emission tomography (PET), single photon emission computed tomography (SPECT), and magnetic resonance imaging (MRI), study of the structure and the functioning of the brain can be done. With the aid of modern technology and the new availability of both normal and autism tissue samples to do postmortem studies, researchers will be able to learn much through comparative studies.
Postmortem and MRI studies have shown that many major brain structures are implicated in autism. This includes the cerebellum, cerebral cortex, limbic system, corpus callosum, basal ganglia, and brain stem. 28 Other research is focusing on the role of neurotransmitters such as serotonin, dopamine, and epinephrine.
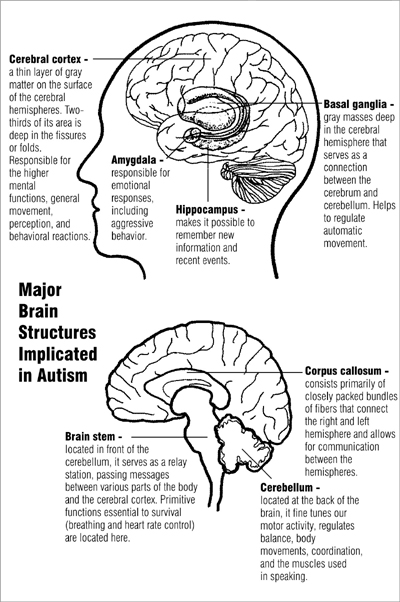
Research into the causes of autism spectrum disorders is being fueled by other recent developments. Evidence points to genetic factors playing a prominent role in the causes for ASD. Twin and family studies have suggested an underlying genetic vulnerability to ASD. 29 To further research in this field, the Autism Genetic Resource Exchange, a project initiated by the Cure Autism Now Foundation, and aided by an NIMH grant, is recruiting genetic samples from several hundred families. Each family with more than one member diagnosed with ASD is given a 2-hour, in-home screening. With a large number of DNA samples, it is hoped that the most important genes will be found. This will enable scientists to learn what the culprit genes do and how they can go wrong.
Another exciting development is the Autism Tissue Program (http://www.brainbank.org), supported by the Autism Society of America Foundation, the Medical Investigation of Neurodevelopmental Disorders (M.I.N.D.) Institute at the University of California, Davis, and the National Alliance for Autism Research. The program is aided by a grant to the Harvard Brain and Tissue Resource Center (http://www.brainbank.mclean.org), funded by the National Institute of Mental Health (NIMH) and the National Institute of Neurological Disorders and Stroke (NINDS). Studies of the postmortem brain with imaging methods will help us learn why some brains are large, how the limbic system develops, and how the brain changes as it ages. Tissue samples can be stained and will show which neurotransmitters are being made in the cells and how they are transported and released to other cells. By focusing on specific brain regions and neurotransmitters, it will become easier to identify susceptibility genes.
Recent neuroimaging studies have shown that a contributing cause for autism may be abnormal brain development beginning in the infant's first months. This "growth dysregulation hypothesis" holds that the anatomical abnormalities seen in autism are caused by genetic defects in brain growth factors. It is possible that sudden, rapid head growth in an infant may be an early warning signal that will lead to early diagnosis and effective biological intervention or possible prevention of autism. 30 For detailed information on autism spectrum disorders research, see NIMH research fact sheet, Autism Spectrum Disorders Research .
The Children's Health Act of 2000—What It Means to Autism Research
The Children's Health Act of 2000 was responsible for the creation of the Interagency Autism Coordinating Committee (IACC), a committee that includes the directors of five NIH institutes—the National Institute of Mental Health, the National Institute of Neurological Disorders and Stroke, the National Institute on Deafness and Other Communication Disorders (NIDCD), the National Institute of Child Health and Human Development (NICHD), and the National Institute of Environmental Health Sciences (NIEHS)—as well as representatives from the Health Resource Services Administration, the National Center on Birth Defects and Developmental Disabilities (a part of the Centers for Disease Control), the Agency for Toxic Substances and Disease Registry, the Substance Abuse and Mental Health Services Administration, the Administration on Developmental Disabilities, the Centers for Medicare and Medicaid Services, the U.S. Food and Drug Administration, and the U.S. Department of Education. The Committee, instructed by the Congress to develop a 10-year agenda for autism research, introduced the plan, dubbed a "matrix" or a "roadmap," at the first Autism Summit Conference in November 2003. The roadmap indicates priorities for research for years 1 to 3, years 4 to 6, and years 7 to 10.
The five NIH institutes of the IACC have established the Studies to Advance Autism Research and Treatment (STAART) Network, composed of eight network centers. They will conduct research in the fields of developmental neurobiology, genetics, and psychopharmacology. Each center is pursuing its own particular mix of studies, but there also will be multi-site clinical trials within the STAART network.
The STAART centers are located at the following sites:
- University of North Carolina, Chapel Hill Yale University, Connecticut University of Washington, Seattle University of California, Los Angeles Mount Sinai Medical School, New York Kennedy Krieger Institute, Maryland Boston University, Massachusetts University of Rochester, New York
A data coordination center will analyze the data generated by both the STAART network and the Collaborative Programs of Excellence in Autism (CPEA). This latter program, funded by the NICHD and the NIDCD Network on the Neurobiology and Genetics of Autism, consists of 10 sites. The CPEA is at present studying the world's largest group of well-diagnosed individuals with autism characterized by genetic and developmental profiles. The CPEA centers are located at:
- Boston University, Massachusetts University of California, Davis University of California, Irvine University of California, Los Angeles Yale University, Connecticut University of Washington, Seattle University of Rochester, New York University of Texas, Houston University of Pittsburgh, Pennsylvania University of Utah, Salt Lake City
The NIEHS has programs at:
- Center for Childhood Neurotoxicology and Assessment, University of Medicine & Dentistry, New Jersey The Center for the Study of Environmental Factors in the Etiology of Autism, University of California, Davis
1 American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR (fourth edition, text revision). Washington DC: American Psychiatric Association, 2000.
2 Filipek PA, Accardo PJ, Baranek GT, Cook Jr. EH, Dawson G, Gordon B, Gravel JS, Johnson CP, Kellen RJ, Levy SE, Minshew NJ, Prizant BM, Rapin I, Rogers SJ, Stone WL, Teplin S, Tuchman RF, Volkmar FR. The screening and diagnosis of autism spectrum disorders. Journal of Autism and Developmental Disorders, 1999; 29(2): 439-484.
3 Newschaffer CJ (Johns Hopkins Bloomberg School of Public Health). Autism Among Us: Rising Concerns and the Public Health Response [Video on the Internet]. Public Health Training Network, 2003 June 20. Available from: http://www.publichealthgrandrounds.unc.edu/autism/webcast.htm.
4 Volkmar FR. Medical Problems, Treatments, and Professionals. In: Powers MD, ed. Children with Autism: A Parent's Guide, Second Edition. Bethesda, MD: Woodbine House, 2000; 73-74.
5 Powers MD. What Is Autism? In: Powers MD, ed. Children with Autism: A Parent's Guide, Second Edition. Bethesda, MD: Woodbine House, 2000, 28.
6 Smalley SI, Autism and tuberous sclerosis. Journal of Autism and Developmental Disorders, 1998; 28(5): 407-414.
7 Filipek PA, Accardo PJ, Ashwal S, Baranek GT, Cook Jr. EH, Dawson G, Gordon B, Gravel JS, Johnson CP, Kallen RJ, Levy SE, Minshew NJ, Ozonoff S, Prizant BM, Rapin I, Rogers SJ, Stone WL, Teplin SW, Tuchman RF, Volkmar FR. Practice parameter: screening and diagnosis of autism. Neurology, 2000; 55: 468-479.
8 Baird G, Charman T, Baron-Cohen S, Cox A, Swettenham J, Wheelwright S, Drew A. A screening instrument for autism at 18 months of age: A 6-year follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry, 2000; 39: 694-702.
9 Robbins DI, Fein D, Barton MI, Green JA. The modified checklist for autism in toddlers: an initial study investigating the early detection of autism and pervasive developmental disorders. Journal of Autism and Developmental Disorders, 2001; 31(2): 149-151.
10 Stone WL, Coonrod EE, Ousley OY. Brief report: screening tool for autism in two-year-olds (STAT): development and preliminary data. Journal of Autism and Developmental Disorders, 2000; 30(6): 607-612.
11 Berument SK, Rutter M, Lord C, Pickles A, Bailey A. Autism Screening Questionnaire: diagnostic validity. British Journal of Psychiatry, 1999; 175: 444-451.
12 Ehlers S, Gillberg C, Wing L. A screening questionnaire for Asperger syndrome and other high-functioning autism spectrum disorders in school age children. Journal of Autism and Developmental Disorders, 1999; 29(2): 129-141.
13 Garnett MS, Attwood AJ. The Australian scale for Asperger's syndrome. In: Attwood, Tony. Asperger's Syndrome: A Guide for Parents and Professionals. London: Jessica Kingsley Publishers, 1997.
14 Scott FJ, Baron-Cohen S, Bolton P, Brayne C. The Cast (Childhood Asperger Syndrome Test): preliminary development of a UK screen for mainstream primary-school-age children. Autism, 2002; 2(1): 9-31.
15 Tadevosyan-Leyfer O, Dowd M, Mankoski R, Winklosky B, Putnam S, McGrath L, Tager-Flusberg H, Folstein SE. A principal components analysis of the autism diagnostic interview-revised. Journal of the American Academy of Child and Adolescent Psychiatry, 2003; 42(7): 864-872.
16 Lord C, Risi S, Lambrecht L, Cook EH, Leventhal BL, DiLavore PC, Pickles A, Rutter M. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 2000; 30(3): 205-230.
17 Van Bourgondien ME, Marcus LM, Schopler E. Comparison of DSM-III-R and childhood autism rating scale diagnoses of autism. Journal of Autism and Developmental Disorders, 1992; 22(4): 493-506.
18 Department of Health and Human Services. Mental Health: A Report of the Surgeon General. Rockville, MD: Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institute of Mental Health, 1999.
19 Lovaas OI. Behavioral treatment and normal educational and intellectual functioning in young autistic children. Journal of Consulting and Clinical Psychology, 1987; 55: 3-9.
20 McEachin JJ, Smith T, Lovaas OI. Long-term outcome for children with autism who received early intensive behavioral treatment. American Journal on Mental Retardation, 1993; 97: 359-372.
21 Couper JJ, Sampson AJ. Children with autism deserve evidence-based intervention. Medical Journal of Australia, 2003; 178: 424-425.
22 American Academy of Pediatrics Committee on Children With Disabilities. The pediatrician's role in the diagnosis and management of autistic spectrum disorder in children. Pediatrics, 2001; 107(5): 1221-1226.
23 Dunlap G, Foxe L. Teaching students with autism. ERIC EC Digest #E582, 1999 October.
24 Autism Society of America. Biomedical and Dietary Treatments (Fact Sheet) [cited 2004], 2003. Bethesda, MD: Autism Society of America. Available from: www.autism-society.org/site/PageServer .
25 McDougle CJ, Stigler KA, Posey DJ. Treatment of aggression in children and adolescents with autism and conduct disorder. Journal of Clinical Psychiatry, 2003; 64 (supplement 4): 16-25.
26 Research Units on Pediatric Psychopharmacology Network. Risperidone in children with autism and serious behavioral problems. New England Journal of Medicine, 2002; 347(5): 314-321.
27 Hviid A, Stellfeld M, Wohlfahrt J, Melbye M. Association between thimerosal-containing vaccine and autism. JAMA, 2003; 290(13): 1763-1766.
28 Akshoomoff N, Pierce K, Courchesne E. The neurobiological basis of autism from a developmental perspective. Development and Psychopathology, 2002; 14: 613-634.
29 Korvatska E, Van de Water J, Anders TF, Gershwin ME. Genetic and immunologic considerations in autism. Neurobiology of Disease, 2002; 9: 107-125.
30 Courchesne E. Carper R, Akshoomoff N. Evidence of brain overgrowth in the first year of life in autism. JAMA, 2003; 290(3): 337-344. NIH Publication No.04-5511 April 2004 Citation for this publication: Strock, Margaret (2004). Autism Spectrum Disorders (Pervasive Developmental Disorders). NIH Publication No. NIH-04-5511, National Institute of Mental Health, National Institutes of Health, U.S. Department of Health and Human Services, Bethesda, MD, 40 pp. http://www.nimh.nih.gov/publicat/autism.cfm
- Attention Deficit Hyperactive Disorder
- Early Intervention
- Emotional and Behavioral Disorders
- Generalized Anxiety
- Gifted and Talented
- Hearing Impairments
- Learning Disabilities
- Intellectual Disabilities
- Orthopedic Impairments
- Other Health Impairments
- Social Security and Disability Information and Benefits
- Speech and Language Impairments
- Traumatic Brain Injury and Neurological Impairment
- Visual Impairments
©2024 National Association of Special Education Teachers. All rights reserved
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Signs and Symptoms
- Living with Autism Spectrum Disorder
- Frequently Asked Questions (FAQs)
- Data and Statistics on Autism Spectrum Disorder
- Autism Materials and Resources
- Diagnosis ASD
- Information on ASD for Healthcare Providers
- Autism Acceptance Month Partner Toolkit
Related Topics:
- Show All Home
- 2023 Community Report on Autism
- Autism Data Visualization Tool
Information on Autism Spectrum Disorder for Families
At a glance.
This page has tools and information about autism spectrum disorder (ASD) for families.

Concerned about your child's development?
If you're concerned — act early , developmental milestone tools for parents, free learn the signs. act early. materials .

Links and resources for families
About autism spectrum disorder, developmental milestones, screening and diagnosis of asd, treatments for asd, living with asd, positive parenting tips, autism spectrum disorder (asd).
Autism spectrum disorder (ASD) is a developmental disability that can cause significant social, communication and behavioral challenges. CDC is committed to continuing to provide essential data on ASD and develop resources that help identify children with ASD as early as possible.
For Everyone
Health care providers, public health.
- Patient Care & Health Information
- Diseases & Conditions
- Autism spectrum disorder
Your child's doctor will look for signs of developmental delays at regular checkups. If your child shows any symptoms of autism spectrum disorder, you'll likely be referred to a specialist who treats children with autism spectrum disorder, such as a child psychiatrist or psychologist, pediatric neurologist, or developmental pediatrician, for an evaluation.
Because autism spectrum disorder varies widely in symptoms and severity, making a diagnosis may be difficult. There isn't a specific medical test to determine the disorder. Instead, a specialist may:
- Observe your child and ask how your child's social interactions, communication skills and behavior have developed and changed over time
- Give your child tests covering hearing, speech, language, developmental level, and social and behavioral issues
- Present structured social and communication interactions to your child and score the performance
- Use the criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association
- Include other specialists in determining a diagnosis
- Recommend genetic testing to identify whether your child has a genetic disorder such as Rett syndrome or fragile X syndrome
No cure exists for autism spectrum disorder, and there is no one-size-fits-all treatment. The goal of treatment is to maximize your child's ability to function by reducing autism spectrum disorder symptoms and supporting development and learning. Early intervention during the preschool years can help your child learn critical social, communication, functional and behavioral skills.
The range of home-based and school-based treatments and interventions for autism spectrum disorder can be overwhelming, and your child's needs may change over time. Your health care provider can recommend options and help identify resources in your area.
If your child is diagnosed with autism spectrum disorder, talk to experts about creating a treatment strategy and build a team of professionals to meet your child's needs.
Treatment options may include:
- Behavior and communication therapies. Many programs address the range of social, language and behavioral difficulties associated with autism spectrum disorder. Some programs focus on reducing problem behaviors and teaching new skills. Other programs focus on teaching children how to act in social situations or communicate better with others. Applied behavior analysis (ABA) can help children learn new skills and generalize these skills to multiple situations through a reward-based motivation system.
- Educational therapies. Children with autism spectrum disorder often respond well to highly structured educational programs. Successful programs typically include a team of specialists and a variety of activities to improve social skills, communication and behavior. Preschool children who receive intensive, individualized behavioral interventions often show good progress.
- Family therapies. Parents and other family members can learn how to play and interact with their children in ways that promote social interaction skills, manage problem behaviors, and teach daily living skills and communication.
- Other therapies. Depending on your child's needs, speech therapy to improve communication skills, occupational therapy to teach activities of daily living, and physical therapy to improve movement and balance may be beneficial. A psychologist can recommend ways to address problem behavior.
- Medications. No medication can improve the core signs of autism spectrum disorder, but specific medications can help control symptoms. For example, certain medications may be prescribed if your child is hyperactive; antipsychotic drugs are sometimes used to treat severe behavioral problems; and antidepressants may be prescribed for anxiety. Keep all health care providers updated on any medications or supplements your child is taking. Some medications and supplements can interact, causing dangerous side effects.
Managing other medical and mental health conditions
In addition to autism spectrum disorder, children, teens and adults can also experience:
- Medical health issues. Children with autism spectrum disorder may also have medical issues, such as epilepsy, sleep disorders, limited food preferences or stomach problems. Ask your child's doctor how to best manage these conditions together.
- Problems with transition to adulthood. Teens and young adults with autism spectrum disorder may have difficulty understanding body changes. Also, social situations become increasingly complex in adolescence, and there may be less tolerance for individual differences. Behavior problems may be challenging during the teen years.
- Other mental health disorders. Teens and adults with autism spectrum disorder often experience other mental health disorders, such as anxiety and depression. Your doctor, mental health professional, and community advocacy and service organizations can offer help.
Planning for the future
Children with autism spectrum disorder typically continue to learn and compensate for problems throughout life, but most will continue to require some level of support. Planning for your child's future opportunities, such as employment, college, living situation, independence and the services required for support can make this process smoother.
More Information
- Cognitive behavioral therapy
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Alternative medicine
Because autism spectrum disorder can't be cured, many parents seek alternative or complementary therapies, but these treatments have little or no research to show that they're effective. You could, unintentionally, reinforce negative behaviors. And some alternative treatments are potentially dangerous.
Talk with your child's doctor about the scientific evidence of any therapy that you're considering for your child.
Examples of complementary and alternative therapies that may offer some benefit when used in combination with evidence-based treatments include:
- Creative therapies. Some parents choose to supplement educational and medical intervention with art therapy or music therapy, which focuses on reducing a child's sensitivity to touch or sound. These therapies may offer some benefit when used along with other treatments.
- Sensory-based therapies. These therapies are based on the unproven theory that people with autism spectrum disorder have a sensory processing disorder that causes problems tolerating or processing sensory information, such as touch, balance and hearing. Therapists use brushes, squeeze toys, trampolines and other materials to stimulate these senses. Research has not shown these therapies to be effective, but it's possible they may offer some benefit when used along with other treatments.
- Massage. While massage may be relaxing, there isn't enough evidence to determine if it improves symptoms of autism spectrum disorder.
- Pet or horse therapy. Pets can provide companionship and recreation, but more research is needed to determine whether interaction with animals improves symptoms of autism spectrum disorder.
Some complementary and alternative therapies may not be harmful, but there's no evidence that they're helpful. Some may also include significant financial cost and be difficult to implement. Examples of these therapies include:
- Special diets. There's no evidence that special diets are an effective treatment for autism spectrum disorder. And for growing children, restrictive diets can lead to nutritional deficiencies. If you decide to pursue a restrictive diet, work with a registered dietitian to create an appropriate meal plan for your child.
- Vitamin supplements and probiotics. Although not harmful when used in normal amounts, there is no evidence they are beneficial for autism spectrum disorder symptoms, and supplements can be expensive. Talk to your doctor about vitamins and other supplements and the appropriate dosage for your child.
- Acupuncture. This therapy has been used with the goal of improving autism spectrum disorder symptoms, but the effectiveness of acupuncture is not supported by research.
Some complementary and alternative treatments do not have evidence that they are beneficial and they're potentially dangerous. Examples of complementary and alternative treatments that are not recommended for autism spectrum disorder include:
- Chelation therapy. This treatment is said to remove mercury and other heavy metals from the body, but there's no known link with autism spectrum disorder. Chelation therapy for autism spectrum disorder is not supported by research evidence and can be very dangerous. In some cases, children treated with chelation therapy have died.
- Hyperbaric oxygen treatments. Hyperbaric oxygen is a treatment that involves breathing oxygen inside a pressurized chamber. This treatment has not been shown to be effective in treating autism spectrum disorder symptoms and is not approved by the Food and Drug Administration (FDA) for this use.
- Intravenous immunoglobulin (IVIG) infusions. There is no evidence that using IVIG infusions improves autism spectrum disorder, and the FDA has not approved immunoglobulin products for this use.
Coping and support
Raising a child with autism spectrum disorder can be physically exhausting and emotionally draining. These suggestions may help:
- Find a team of trusted professionals. A team, coordinated by your doctor, may include social workers, teachers, therapists, and a case manager or service coordinator. These professionals can help identify and evaluate the resources in your area and explain financial services and state and federal programs for children and adults with disabilities.
- Keep records of visits with service providers. Your child may have visits, evaluations and meetings with many people involved in his or her care. Keep an organized file of these meetings and reports to help you decide about treatment options and monitor progress.
- Learn about the disorder. There are many myths and misconceptions about autism spectrum disorder. Learning the truth can help you better understand your child and his or her attempts to communicate.
- Take time for yourself and other family members. Caring for a child with autism spectrum disorder can put stress on your personal relationships and your family. To avoid burnout, take time out to relax, exercise or enjoy your favorite activities. Try to schedule one-on-one time with your other children and plan date nights with your spouse or partner — even if it's just watching a movie together after the children go to bed.
- Seek out other families of children with autism spectrum disorder. Other families struggling with the challenges of autism spectrum disorder may have useful advice. Some communities have support groups for parents and siblings of children with the disorder.
- Ask your doctor about new technologies and therapies. Researchers continue to explore new approaches to help children with autism spectrum disorder. See the Centers for Disease Control and Prevention website on autism spectrum disorders for helpful materials and links to resources.
Preparing for your appointment
Your child's health care provider will look for developmental problems at regular checkups. Mention any concerns you have during your appointment. If your child shows any signs of autism spectrum disorder, you'll likely be referred to a specialist who treats children with the disorder for an evaluation.
Bring a family member or friend with you to the appointment, if possible, to help you remember information and for emotional support.
Here's some information to help you prepare for your appointment.
What you can do
Before your child's appointment, make a list of:
- Any medications, including vitamins, herbs and over-the-counter medicines that your child is taking, and their dosages.
- Any concerns you have about your child's development and behavior.
- When your child began talking and reaching developmental milestones. If your child has siblings, also share information about when they reached their milestones.
- A description of how your child plays and interacts with other children, siblings and parents.
- Questions to ask your child's doctor to make the most of your time.
In addition, it may be helpful to bring:
- Notes of any observations from other adults and caregivers, such as babysitters, relatives and teachers. If your child has been evaluated by other health care professionals or an early intervention or school program, bring this assessment.
- A record of developmental milestones for your child, such as a baby book or baby calendar, if you have one.
- A video of your child's unusual behaviors or movements, if you have one.
Questions to ask your child's doctor may include:
- Why do you think my child does (or doesn't) have autism spectrum disorder?
- Is there a way to confirm the diagnosis?
- If my child does have autism spectrum disorder, is there a way to tell how severe it is?
- What changes can I expect to see in my child over time?
- What kind of special therapies or care do children with autism spectrum disorder need?
- How much and what kinds of regular medical care will my child need?
- What kind of support is available to families of children with autism spectrum disorder?
- How can I learn more about autism spectrum disorder?
Don't hesitate to ask other questions during your appointment.
What to expect from your child's doctor
Your child's doctor is likely to ask you a number of questions. Be ready to answer them to reserve time to go over any points you want to focus on. Your doctor may ask:
- What specific behaviors prompted your visit today?
- When did you first notice these signs in your child? Have others noticed signs?
- Have these behaviors been continuous or occasional?
- Does your child have any other symptoms that might seem unrelated to autism spectrum disorder, such as stomach problems?
- Does anything seem to improve your child's symptoms?
- What, if anything, appears to worsen symptoms?
- When did your child first crawl? Walk? Say his or her first word?
- What are some of your child's favorite activities?
- How does your child interact with you, siblings and other children? Does your child show interest in others, make eye contact, smile or want to play with others?
- Does your child have a family history of autism spectrum disorder, language delay, Rett syndrome, obsessive-compulsive disorder, or anxiety or other mood disorders?
- What is your child's education plan? What services does he or she receive through school?
- Autism spectrum disorder (ASD). Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/autism/facts.html. Accessed April 4, 2017.
- Uno Y, et al. Early exposure to the combined measles-mumps-rubella vaccine and thimerosal-containing vaccines and risk of autism spectrum disorder. Vaccine. 2015;33:2511.
- Taylor LE, et al. Vaccines are not associated with autism: An evidence-based meta-analysis of case-control and cohort studies. Vaccine. 2014;32:3623.
- Weissman L, et al. Autism spectrum disorder in children and adolescents: Overview of management. https://www.uptodate.com/home. Accessed April 4, 2017.
- Autism spectrum disorder. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. Arlington, Va.: American Psychiatric Association; 2013. http://dsm.psychiatryonline.org. Accessed April 4, 2017.
- Weissman L, et al. Autism spectrum disorder in children and adolescents: Complementary and alternative therapies. https://www.uptodate.com/home. Accessed April 4, 2017.
- Augustyn M. Autism spectrum disorder: Terminology, epidemiology, and pathogenesis. https://www.uptodate.com/home. Accessed April 4, 2017.
- Bridgemohan C. Autism spectrum disorder: Surveillance and screening in primary care. https://www.uptodate.com/home. Accessed April 4, 2017.
- Levy SE, et al. Complementary and alternative medicine treatments for children with autism spectrum disorder. Child and Adolescent Psychiatric Clinics of North America. 2015;24:117.
- Brondino N, et al. Complementary and alternative therapies for autism spectrum disorder. Evidence-Based Complementary and Alternative Medicine. http://dx.doi.org/10.1155/2015/258589. Accessed April 4, 2017.
- Volkmar F, et al. Practice parameter for the assessment and treatment of children and adolescents with autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2014;53:237.
- Autism spectrum disorder (ASD). Eunice Kennedy Shriver National Institute of Child Health and Human Development. https://www.nichd.nih.gov/health/topics/autism/Pages/default.aspx. Accessed April 4, 2017.
- American Academy of Pediatrics policy statement: Sensory integration therapies for children with developmental and behavioral disorders. Pediatrics. 2012;129:1186.
- James S, et al. Chelation for autism spectrum disorder (ASD). Cochrane Database of Systematic Reviews. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD010766.pub2/abstract;jsessionid=9467860F2028507DFC5B69615F622F78.f04t02. Accessed April 4, 2017.
- Van Schalkwyk GI, et al. Autism spectrum disorders: Challenges and opportunities for transition to adulthood. Child and Adolescent Psychiatric Clinics of North America. 2017;26:329.
- Autism. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed April 4, 2017.
- Autism: Beware of potentially dangerous therapies and products. U.S. Food and Drug Administration. https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm394757.htm?source=govdelivery&utm_medium=email&utm_source=govdelivery. Accessed May 19, 2017.
- Drutz JE. Autism spectrum disorder and chronic disease: No evidence for vaccines or thimerosal as a contributing factor. https://www.uptodate.com/home. Accessed May 19, 2017.
- Weissman L, et al. Autism spectrum disorder in children and adolescents: Behavioral and educational interventions. https://www.uptodate.com/home. Accessed May 19, 2017.
- Huebner AR (expert opinion). Mayo Clinic, Rochester, Minn. June 7, 2017.
- Autism spectrum disorder and digestive symptoms
Associated Procedures
News from mayo clinic.
- Understanding autism: The path to diagnosis, awareness and support April 28, 2024, 11:00 a.m. CDT
- 10 significant studies from Mayo Clinic's Center for Individualized Medicine in 2023 Dec. 30, 2023, 12:00 p.m. CDT
- Mayo Clinic 'mini-brain' study reveals possible key link to autism spectrum disorder Aug. 10, 2023, 04:00 p.m. CDT
Products & Services
- Children’s Book: My Life Beyond Autism
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be part of the cutting-edge research and care that's changing medicine.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
8 Types of Schools for Autistic Kids
- School Options
How To Choose
Frequently asked questions.
When it comes to autism and education, there is no one-size-fits-all approach. As with many things concerning autistic kids , the definition of a good educational program depends upon the individual child.
Autism spectrum disorder has two core features doctors use to make a diagnosis: social communication differences or difficulties and specific or repetitive interests and behaviors. Among autistic people, there is a wide variation of traits, strengths, and support needs.
Many autistic children need some degree of classroom support, but the needs will vary greatly from child to child. Like neurotypical children, some autistic children have more academic challenges than others.
This article discusses the different challenges autistic children may face in a school setting and the various educational options available. It will also provide tips for advocating for your child within the school system and factors to take into consideration as you enroll your autistic child in school.
Each autistic child is unique, but there are some common areas where many autistic people struggle. Sensory challenges, emotional regulation, executive functioning, and social skills are factors to consider when determining the best school setting for a child.
Sensory Processing Disorder
Schools can be a hotbed of sensory processing problems for autistic people. Loud noises like rowdy kids in the hallways, echoing gymnasiums, class bells, and fire alarms can be jarring. Various strong smells—from the classic musty, old school building smell that greets you at the door to mysterious food smells wafting from the cafeteria and odorous locker rooms—can irritate autistic children.
Add in humming fluorescent lights, uncomfortable clothing , and having to sit still when you want to run, and traditional school settings can be a real challenge for some autistic people.
Emotional Regulation
The individual burden of emotional regulation is larger for autistic people. Autistic people have more emotional triggers than neurotypical people and a decreased capacity to process them internally. Anxiety, anger, excitement, sadness, and other emotions can feel overwhelming. Some autistic people will react in ways that do not conform to expectations for traditional classroom settings.
Some examples:
- Running out of the classroom and possibly even the building, known as eloping
- Shutting down and putting their head on the desk or hiding under the desk
- Having loud, emotional outbursts, such as screaming, crying, or sobbing loudly where other students can hear
An autistic child who struggles with emotional regulation will need emotional support in the classroom. This can look like a classroom aide who your child considers a safe person. Emotional support can also look like allow stimming at the student's desk, or accommodations that allow the student to leave class for a period of time to a calming space when they are feeling a meltdown coming on.
Intellectual Capabilities
Like all students, autistic students have a wide range of intellectual capabilities. Some children qualify for gifted or advanced classes, and some children have learning disabilities; the same child might fit into both categories. A child's ability to learn can help determine the type of classroom or school that best suits them.
Some autistic students require special education classes, while others do better with advanced learning opportunities that keep them engaged in the classroom.
Social Skills
Social skills that come naturally to neurotypical people may confuse autistic people. This can affect a child's ability to participate in the classroom fully. As a result, autistic students face some social challenges.
It can also impact making friends on the playground and other social aspects of school. Research shows autistic children are at an increased risk of bullying from other students.
Educational Options for Autistic Kids
There are various educational opportunities for autistic students: a general education classroom, a resource classroom, a special education classroom, or an autistic-only setting. Some autistic students thrive in an inclusive class setting, while others are better in more tailored settings. It all depends on the child.
In the United States, the Individuals with Disabilities Education Act (IDEA) requires that school districts provide the "Least Restrictive Environment" for a child's education. That means the district must consider options such as inclusive class settings before placing the child in a more specialized setting.
If you feel a child would be better off in a specialized environment, you may need to prove that the more inclusive settings are not working before the district funds tuition for a particular school.
Autistic children often qualify for an individualized education plan (IEP) or 504 plan that allows classroom accommodations. However, just having a medical diagnosis of autism does not automatically qualify a student for accommodations. The district's child study team will determine whether the student requires additional support.
Inclusion—a newer term that replaced mainstreaming—describes a setting where a child is part of a typical classroom with minimal extra support. Some accommodations may be in place, but in general, the child is expected to be able to be able to self regulate in a large group, follow the teacher's directions, and do work at or near grade level.
Inclusive settings generally work best for children whose independence matches or exceeds their age group, and who are at least moderately social in a way that's surface-level compatible with neurotypical expectations. Inclusion settings may be especially tough for children who are non-verbal, very anxious, or likely to meltdown when under stress.
The benefit of inclusion is that the child is placed in the standard education program with their neurotypical peers. The drawback of inclusion classrooms without additional support is that an autistic child may feel the need to mask their autism, a process that can be very tiring and may not be able to be maintained. This can result in autistic burnout and depression.
Inclusion With Support
For autistic students who perform on an average level or better but struggle in an inclusion setting, the proper support can help them to be successful. Support options are spelled out in the IEP or 504 plan and may include a 1:1 aide, adapted curriculum, reduced homework, modified social groups, and more.
Many parents prefer inclusion with support as a compromise between a special education classroom and unsupported mainstreaming. Inclusion can be a terrific option for many autistic students with the proper support.
Inclusion with support does have its downsides. Autistic children in a typical classroom may be more likely to suffer from bullying and teasing. If the child has a 1:1 aide, the teacher may assume the student is taken care of and focus their attention on other students. Adapted curriculum may be taught by the aide and not the trained, credentialed teacher.
Special Education
Autistic students are sometimes placed in a special or disability education classroom in their local public school. This option may work well for students with learning disabilities if the teacher is also experienced in teaching autistic children.
The benefits of special education settings are that the classes are usually smaller, there is more opportunity to work on social skills, and students are generally included in all school activities, electives, and events.
However, special or disability education classrooms are generally intended for disabled children who have a tough time with academics. Many autistic children are comfortable with academics but struggle with social skills. For many autistic students, a special or disability education classroom may be the wrong setting.
Autistic Support Classrooms
Some larger school districts offer autistic support classrooms within their public schools. These classrooms are set up to meet the specific needs of autistic children. They are staffed by teachers and aides trained on both autism and education.
Autistic support classrooms have several advantages: They are usually very small, with a high adult-to-child ratio. They use teaching tools geared toward keeping autistic children engaged in lessons, and the curricula often weave in speech and social skills training . Students in autistic support classrooms are also included in general school activities such as assemblies, recess, and electives.
Children in these classes often spend most of the day with only other autistic children. This can be great because it means your child will not have to mask or explain their natural behavior. On the downside, autistic support classrooms tend to be quite segregated from the rest of the school. Plus, with so much attention paid to building social skills, this setting may neglect your child's academic strengths and abilities.
In addition, autistic support classrooms often use applied behavioral analysis (ABA) techniques to train autistic children to behave like neurotypical children. While ABA therapy may be effective for some autistic children, a 2018 study found that autistic people who were exposed to ABA therapy had an 86% greater likelihood of developing post-traumatic stress disorder.
Private Schools
Private schools may offer small classes, individualized attention, and terrific resources. This may be a good option for an autistic student who is independent, excels academically, and is comfortable socializing with neurotypical people with little understanding of autism. However, most private schools will not make any special accommodations for students. Few typical private schools are well prepared to handle any disability.
Of course, it is always possible that your local community has a special private offering, such as a co-op school or an alternative learning center, that may be appropriate for an autistic child. It is also possible that the student will develop the skills needed to attend a small private high school. But all of the pieces need to be in place for a typical private school to be a viable option.

Special Private Schools
Some major metropolitan areas may have private schools for children with disabilities. Many of these schools focus on children with learning disabilities or behavioral problems. But more and more schools are starting to specialize exclusively in autism . In addition to day schools, there are boarding schools across the country that cater to autistic people.
Schools for autistic children are usually a good match if the student has a difficult time matching neurotypical standards for independence or social skills—and thus unlikely to do well in a less restrictive setting—or profoundly unhappy or stressed in a neurotypical setting.
These schools have the benefit that everyone on staff knows and understands autism. They typically offer a wide range of on-site therapeutic resources, from sensory gyms and quiet zones to behavioral and occupational therapists on staff.
One thing to watch out for with a therapeutic school is ABA therapy, a controversial topic among autistic adults. ABA is a type of compliance training that helps autistic people appear neurotypical. Many autistic adults claim ABA's coerced compliance is manipulative, disingenuous, and even abusive.
One potential downside of a school that caters exclusively to autistic students is that the child may miss out on socializing with neurotypical people who make up around 80-85% of the population. However, some children with may do better in a school for autistic children since they are often extremely sensitive to the inevitable teasing in traditional school settings.
The obvious downside of a specialized private school is that tuition can be expensive. While it may be possible to convince a school district to underwrite an approved private school placement, it is usually a tough sell. You may need to hire a lawyer or special education advocate to get the district pay for specialized placement.
Homeschooling
Because the options for educating an autistic child are limited—and in many areas almost non-existent—many families are turning to homeschooling .
This can be tough for many families because it requires an adult to stay home to educate the child. For two-income families, this can be a significant financial sacrifice. This option often makes the most sense, particularly if the relationship with the local school district has become strained.
If the idea of being responsible for an autistic child's education is overwhelming, there are plenty of online homeschooling options. You can also find other local homeschooling families with autistic children to share curricula and go on field trips together.
The greatest upside to homeschooling is its absolute flexibility. If a child loves trains, for example, you can use Thomas the Tank Engine to teach reading and math skills—an approach that has a good chance of success.
Homeschooling laws vary from state to state. Some require the student to submit a portfolio of work, while other states do not provide any oversight for homeschooling. Be sure to look into your local laws before withdrawing your student from school.
Unschooling
Another option gaining traction in the autistic community is known as unschooling. Unschooling is child-led learning at home or in places other than a school. There is no traditional curriculum for unschooling. Instead, children are taught in a curious and demand-free setting based on their interests.
The philosophy of unschooling is that children are naturally curious and learn best following their interests. It is intended to be stress-free for the student and allow them to unwind, recover from school trauma, and follow their curiosity.
Unschooling is often recommended for autistic students who do not thrive in a traditional school setting or experience autistic burnout. Some families use unschooling as a temporary bridge between conventional school and homeschooling. It is commonly recommended to unschool for at least one month for every year in school before trying any formalized homeschooling.
The downsides of unschooling include fewer opportunities for socialization and the potential judgment from others. Legally, unschooling falls under the homeschool umbrella. Laws vary from state to state, and you may be required to show a portfolio of work.
Determining the proper placement for your autistic learner depends on several factors. Some points to consider as you think about the options are:
- The autistic child's communication ability and level of social engagement
- Their academic skills
- How they handle large groups
- Tolerance for sensory input
- Ability to focus on classwork
- Prior classroom experience
You will also want to look into the programs available in your local school district and any private or charter school options in your area.
Ensuring an autistic child has a positive school experience may require a little extra work on your part. You are the advocate for the child in your care, and you'll want to have a cooperative partnership with their teachers.
Creating a one-page fact sheet on your child can help ease the transition to a new school situation. In addition to listing their diagnoses (if you are comfortable sharing them), include a child's strengths, quirks, triggers, and anything that helps calm the child down. Make sure your contact and emergency contact information is visible at the top of the page.
Most autistic children will need extra support in school through a 504 plan or an IEP. This can be a long and sometimes frustrating process. Each state has its own timeline and regulations for 504 plans and IEPs. Check with your state department of education to find out the rules in your area.
A Word From Verywell
Determining the proper placement for an autistic learner can be a lengthy process. Try to work with the child's teacher and school district to get the right support.
If a child is struggling, keeping a log of the type and frequency of problems a child is having can help build a case for more support (like a 1:1 aide) or a different educational setting. Should you encounter resistance from the school district, consider consulting a special education advocate or educational lawyer. Some legal groups focused on disability may offer pro-bono or sliding scale opportunities.
Ultimately, the right school placement for an autistic child depends on their personality, strengths, struggles, and unique family situation. Some children do better in a school setting, while others do better at home. There is no right or wrong answer. What matters is that a child feels safe in their educational environment to be their personal best.
Prior to the publication of the Diagnostic and Statistical Manual of Mental Disorders, 5th edition , (DSM-5) in 2013, autism was split into five different diagnoses: autistic disorder, Asperger's syndrome, Rett syndrome, childhood disintegrative disorder, and pervasive developmental disorder not otherwise specified (PDD-NOS).
The DSM-5 combined three of those items—autistic disorder, Asperger's syndrome, and PDD-NOS—under the umbrella of autism spectrum disorder with three different levels. A Level 1 means a child will need some support, Level 2 means substantial support, and Level 3 means very substantial support.
Every autistic person is different. Some of the ways autism can affect a student include difficulty with social interactions, pragmatic language deficits, emotional regulation issues, sensory processing problems, shorter attention spans, and executive functioning challenges.
The label of high-functioning autism is a bit of a misnomer and functioning labels are discouraged in the autistic community. The term high-functioning autistic is sometimes used to dismiss the student's need for support. But, by definition, a diagnosis of autism means the person requires some level of support.
HIgh-functioning is typically used to describe people with Level 1 ASD. With the right support, people with Level 1 autism can be as successful as their neurotypical peers and possibly even more successful. However, there is no guarantee that any child will get the support they need to be their best.
A 504 plan is overseen by the Americans with Disabilities Act and spells out accommodations for students with a physical or emotional disability or impairment.
An individualized education plan (IEP) falls under the Individuals with Disabilities Act (IDEA) and provides special education services to students with a disability that negatively impacts their ability to receive academic instruction.
A 504 plan allows for special accommodations, such as extra breaks, fidgets, modified homework, and extra time for state testing.
An IEP allows for a modified curriculum, classroom accommodations, and therapy services such as speech, occupational, and physical therapy.
Zablotsky B, Bradshaw CP, Anderson CM, Law P. Risk factors for bullying among children with autism spectrum disorders . Autism . 2014;18(4):419-27. doi:10.1177/1362361313477920
Centers for Disease Control and Prevention. Early Intervention and Education for Autism Spectrum Disorder - A Closer Look .
Kupferstein H. Evidence of increased PTSD symptoms in autistics exposed to applied behavior analysis . Adv Autism . 2018;4(1):19-29. doi:10.1108/AIA-08-2017-0016
Sandoval-Norton AH, Shkedy G, Shkedy D. Long-term ABA therapy Is abusive: a response to Gorycki, Ruppel, and Zane . Adv Neurodev Disord. 2021;5: 126–34. doi:10.1007/s41252-021-00201-1
Doyle N. Neurodiversity at work: a biopsychosocial model and the impact on working adults. British Medical Bulletin . 2020;135(1):108-125.
Bottema-Beutel K, Cuda J, Kim SY, Crowley S, Scanlon D. High school experiences and support recommendations of autistic youth . J Autism Dev Disord . 2020;50(9):3397-3412. doi:10.1007/s10803-019-04261-0
Harrower JK, Dunlap G. Including children with autism in general education classrooms. A review of effective strategies . Behav Modif . 2001;25(5):762–84. doi:10.1177/0145445501255006
Mohammadzaheri F, Koegel LK, Rezaei M, Bakhshi E. A randomized clinical trial comparison between Pivotal Response Treatment (PRT) and Adult-Driven Applied Behavior Analysis (ABA) intervention on disruptive behaviors in public school children with autism. J Autism Dev Disord . 2015;45(9):2899-907. doi:10.1007/s10803-015-2451-4
Myers SM, Johnson CP; American Academy of Pediatrics Council on Children With Disabilities. Management of children with autism spectrum disorders . Pediatrics . 2007;120(5):1162–82. doi:10.1542/peds.2007-2362
Rispoli KM, Mathes NE, Malcolm AL. Characterizing the parent role in school-based interventions for autism: A systematic literature review . Sch Psychol . 2019;34(4):444-457. doi:10.1037/spq0000283
Tamm L, Duncan A, Vaughn A, et al. Academic needs in middle school: Perspectives of parents and youth with autism . J Autism Dev Disord . 2020;50(9):3126-3139. doi:10.1007/s10803-019-03995-1
Tiura M, Kim J, Detmers D, Baldi H. Predictors of longitudinal ABA treatment outcomes for children with autism: A growth curve analysis . Res Dev Disabil . 2017;70:185-197. doi:10.1016/j.ridd.2017.09.008
By Lisa Jo Rudy Rudy is a writer, consultant, author, and advocate who specializes in autism. Her work has appeared in The New York Times and Autism Parenting Magazine.
Autism at School
Reviewed by Psychology Today Staff
Children with autism can face an array of challenges at school, from keeping pace in a busy class, to forming relationships with their peers, to struggling with sensory overload in the classroom, hallway, or cafeteria.
Special education services can curb some of these problems. Covered under the Individuals with Disabilities Act, students with autism can access support and services tailored to their individual needs. Parents can play an important role in advocating for their child throughout this process.
On This Page
- How do I get services for my autistic child?
- What is an individualized education program?
- How can I prepare for my annual review meeting?
- What’s the difference between an IEP and a 504 Plan?
- How can I advocate for my autistic child at school?
- What information would help my child’s teacher?
- How can teachers help students with autism?
The first step is to reach out to your child’s school district to schedule an evaluation. This will determine if your child is eligible to receive special education and related services. To be eligible for an individualized education program (IEP), children must have a disability, such as autism, that prevents them from learning successfully in the existing classroom environment.
An IEP team can include the child’s parents, teacher, special education teacher, a representative from the school district, and a therapist to evaluate the results. The group will develop a plan with concrete goals and benchmarks to be reviewed on an annual basis.
Children with autism are guaranteed a free and fair education under the Individuals with Disabilities Education Act (IDEA) which was passed in 1975, and which incorporated autism in 1990. The law enables students to receive an individualized education program , which establishes a child’s academic goals and includes the support they need to achieve those goals.
Those services could involve additional assistance in a typical classroom, learning from a special education teacher, working with a therapist, leveraging helpful technologies, or receiving accommodations such as extra time for assignments. IEPs aim to keep kids in general education classrooms as much as possible, but some parents feel that children with autism are better served in special education classrooms .
A child’s IEP is reviewed every year, and it’s best to enter this meeting as prepared as possible. You can begin by organizing all IEP documents in a binder ahead of time. Read the IEP thoroughly and consider creating a brief summary if that would be helpful. Review the list of accommodations and reflect on which you think were effective and which were not. Ask for data on your child’s performance, and document any concerns you have for the Parental Concerns section.
An IEP and 504 Accommodation Plan both help children receive educational support, but they do so in different ways. IEPs are covered by the Individuals with Disabilities Education Act and pertain to students who qualify for special needs, while 504 Plans fall under the Americans with Disabilities Act and cover students who do not.
IEPs encompass more expansive services and therapies. They revolve around delineating specific goals and monitoring a child’s progress toward achieving those goals. They also require the parent’s participation. 504 plans do not share those traits: They focus on providing accommodations rather than fundamentally changing the educational environment and often apply to students with less severe disabilities.
Although every school is different, there are ways to advocate for your child in any environment. Let the teacher know that your child has autism by sharing a summary of their IEP and a little information about their strengths, weaknesses, and personality. Case managers coordinate the IEP, so make sure your case manager has a strong understanding of autism.
When students are separated into different levels, advocate for your child’s skill level in specific courses rather than deferring to teachers that your child should automatically be in a lower level. Consider which technologies may help your child consume material and function independently, such as note-taking devices.
If your child is bullied, work with the school to eliminate that behavior. Explore an after-school activity that the child is genuinely interested in, such as band or chess club, where he can practice his social skills and learn to function in a group setting.
Teachers may not be familiar with how autistic students experience the classroom. If your child has an IEP, email a brief summary to the teacher beforehand. If your child is higher functioning, explaining a few tips to your child’s general education teacher about autism can be helpful.
Providing a printout or website with the homework can be valuable, because multitasking is difficult for children with autism. They may not be able to write the assignment down at the same time as the teacher is explaining it or conducting the lesson.
Children with autism take things literally. Therefore, delivering specific instructions (“Turn to page 12 and begin to read the chapter” rather than “Turn to page 12”) can help the child keep up. Transitions are stressful and overwhelming for those on the spectrum due to sensory overload. Letting the child leave for their next class a few minutes early can help them to feel settled and focused for the next period. Integrating the child’s passion into the lesson, if the teacher is able, would help excite and engage the child.
Teachers can maintain predictable classroom routines. They can use concrete, specific language, since children with autism perceive language literally. They can incorporate visuals into the lessons to help kids process the material. They can also connect with a student’s parents to learn tips for working with an individual child. Implementing widespread autism competencies for teachers would ensure that every educator is equipped to serve autistic students.

Couples therapy for neurodiverse partners focuses on improving communication and using techniques like structured exercises and sensory regulation for better relationship dynamics.

With the release of "Inside Out 2," there's a fresh opportunity to explore emotions. Read how Disney's storytelling can teach well-being skills to autistic people.

Neurodiversity-specific relationship trends and strategies.

People who feel "different" from others sometimes wonder if they might be autistic. But feelings of difference can stem from many factors, only one of which is autism.

Amygdala relevance detection theory sheds light on why individuals focus their attention on aspects of their inner experience and environment in unique ways.

Neurodiversity is fundamental to humans and all of our interactions, yet until recently it's been poorly understood at work.

A Personal Perspective: Many of the tasks associated with finding and maintaining employment can be impossible for autistic people.

Personal Perspective: Parents and neurodivergent kids who need accommodations in K-12 schools carry an immense invisible burden.

Two neurodivergent clinicians speak out about how to flourish in college.

Divorcing with a special needs child? Understand the unique legal challenges and five crucial considerations to ensure your child's well-being and secure future.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that could derail our entire day. Here’s how we can face triggers with less reactivity and get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
What is Special Education?Special Education is a set of services provided to students who experience exceptional learning needs. Governed by federal law ( Individuals with Disabilities Education Act, IDEA ), special education is defined as: “Specially designed instruction, at no cost to parents, to meet the unique needs of a child with a disability.” Special education services may be provided across a variety of educational environments to students who have an individualized education program (IEP). Eligibility for special education services requires that students have an identified disability that impacts their ability to learn and requires additional services and resources to effectively participate in school. Children who typically qualify for special education services include those with the following disabilities:
Under the law, the IDEA ensures that regardless of a student’s disability or level of severity, schools must provide an appropriate education to ALL children with a disability (ages 3-21). It also requires that the following six principles be provided for students who receive special education services:
If you are ready to make a difference as an educator and learn new ways to nurture a modern classroom, earn your online Master of Science in Education in Special Education from Purdue University. Within this convenient online platform, you can reach your goals of higher education at an accelerated pace. Call 877-497-5851 to speak with an admissions advisor.
Autism and pervasive developmental disorders sourcebook : basic consumer health information about autism spectrum disorders (ASD) including autistic disorder, asperger syndrome, rett syndrome, childhood disintegrative disorder, and pervasive developmental disorder not otherwise specified (PDDNOS) : along with facts about causes, symptoms, assessment, interventions, treatments, and education, tips for family members and teachers on the transition to adulthood ... / edited by Joyce Brennfleck ShannonFull Text available online AvailabilityFinding items...
Information
InitiativesYou are accessing a machine-readable page. In order to be human-readable, please install an RSS reader. All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess . Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications. Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers. Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal. Original Submission Date Received: .
 Article Menu
Find support for a specific problem in the support section of our website. Please let us know what you think of our products and services. Visit our dedicated information section to learn more about MDPI. JSmol ViewerEvaluating the effects of self-monitoring of performance with a peer component on disruptive behavior and task completion of children with autism spectrum disorder.  1. Introduction2.1. participants and setting, 2.1.1. child participants, 2.1.2. peer mediators, 2.1.3. rbts, 2.2. materials, 2.3. dependent variables and measurement, 2.3.1. disruptive behavior, 2.3.2. task completion, 2.3.3. points earned, 2.4. interobserver agreement, 2.5. procedural fidelity, 2.6. social validity, 2.7. experimental design, 2.8. procedures, 2.8.1. pre-experimental assessments, 2.8.2. smp evaluation, 4. discussion, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
Click here to enlarge figure
Share and CiteGural, I.; Cividini-Motta, C.; Del Vecchio, M.L.; Risse, M.R. Evaluating the Effects of Self-Monitoring of Performance with a Peer Component on Disruptive Behavior and Task Completion of Children with Autism Spectrum Disorder. Behav. Sci. 2024 , 14 , 547. https://doi.org/10.3390/bs14070547 Gural I, Cividini-Motta C, Del Vecchio ML, Risse MR. Evaluating the Effects of Self-Monitoring of Performance with a Peer Component on Disruptive Behavior and Task Completion of Children with Autism Spectrum Disorder. Behavioral Sciences . 2024; 14(7):547. https://doi.org/10.3390/bs14070547 Gural, Isabella, Catia Cividini-Motta, Marissa L. Del Vecchio, and Madeline R. Risse. 2024. "Evaluating the Effects of Self-Monitoring of Performance with a Peer Component on Disruptive Behavior and Task Completion of Children with Autism Spectrum Disorder" Behavioral Sciences 14, no. 7: 547. https://doi.org/10.3390/bs14070547 Article MetricsFurther information, mdpi initiatives, follow mdpi.  Subscribe to receive issue release notifications and newsletters from MDPI journals  Transforming the understanding and treatment of mental illnesses. Información en español Celebrating 75 Years! Learn More >>
Digital Shareables on Autism Spectrum DisorderUse these resources to raise awareness about autism spectrum disorder.  Autism spectrum disorder (ASD) is a neurological and developmental disorder that affects how people interact with others, communicate, learn, and behave. For more information on signs and symptoms, causes and risk factors, diagnosis, and interventions, visit our health topic page or download our brochure . Help raise awareness by sharing information and materials based on the latest research. Share these graphics and social media messagesDownload and share these messages to help spread the word. You can copy and paste the text and graphic into a tweet, email, or post. We encourage you to use the hashtag #shareNIMH in your social media posts to connect with people and organizations with similar goals. For more ideas on how to use these resources, visit our help page .  Let's Talk About AutismHelp increase awareness and acceptance of autism spectrum disorder by sharing information and resources based on the latest research. https://go.nih.gov/nLv8oCK #shareNIMH Copy post to clipboard  Autism Awareness and AcceptanceAutism occurs in all ethnic, racial, sex and gender, and economic groups. This April, learn more about supporting people on the autism spectrum. https://go.nih.gov/nLv8oCK #shareNIMH  About Autism Spectrum DisorderDisponible en español People with autism spectrum disorder often have differences in social behavior and communication, intense interests, and repetitive behaviors. Learn more about the signs, diagnosis, interventions, and resources: https://go.nih.gov/nLv8oCK #shareNIMH  It's recommended that all children should be screened for developmental delays beginning at their 9-month well-child visit and specifically for autism at their 18- and 24-month visits. Learn more at https://go.nih.gov/nLv8oCK #shareNIMH  Autism spectrum disorder can usually be reliably diagnosed by the age of two. If you notice signs, seek an assessment to get the earliest diagnosis, interventions, and services possible. https://go.nih.gov/nLv8oCK #shareNIMH  InterventionAfter diagnosis, interventions and services should begin as soon as possible to support the needs of individuals with autism and make the most of their strengths. https://go.nih.gov/nLv8oCK #shareNIMH  Older Children and AdolescentsMany people are not diagnosed with autism until later childhood or adolescence. To read more about autism identification, visit https://go.nih.gov/nLv8oCK #shareNIMH  Services and Supports for AdultsAdults on the autism spectrum can benefit from services and supports that improve health and well-being across the lifespan. Visit https://go.nih.gov/nLv8oCK to learn more about autism. #shareNIMH Learn more about autism spectrum disorderMore information about autism spectrum disorder, brochures and fact sheets. Last Reviewed: March 2024 An official website of the United States government The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site. The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Save citation to fileEmail citation, add to collections.
Add to My BibliographyYour saved search, create a file for external citation management software, your rss feed.
[Autism spectrum disorder: the impact of an online training strategy on the knowledge of the healthcare staff of a tertiary care hospital]Affiliation.
Abstract in English, SpanishIntroduction: Autism spectrum disorder (ASD) often presents related medical disorders that require specialised healthcare. Professionals in the health sector therefore face difficulties that require specific training in the healthcare needs of this population. Aim: The aim of this study is to quantify paediatric healthcare professionals' knowledge about ASD and to assess the impact of online training. Subjects and methods: It is a quasi-experimental, longitudinal, prospective before-and-after study; study subjects: health professionals; independent variable: online training in ASD; dependent variable: knowledge about ASD. An online training course was held for paediatric professionals to address the core characteristics of diagnosis, as well as the needs they present in the hospital context and the adaptations it is recommended that should be carried out. Fifty-eight healthcare professionals took part. Results: An increase in knowledge about ASD was observed at the end of the intervention (from 73.9% to 85% according to the ASD background knowledge questionnaire), which showed that more than 90% of the participants had the highest level of knowledge about ASD. Conclusions: Online training courses are a useful and effective way to increase knowledge about ASD and the adaptations that are recommended in the hospital setting. More training in ASD should be made available in these settings. Title: Trastorno del espectro autista: impacto de una estrategia de formación en línea en los conocimientos del personal sanitario de un hospital de tercer nivel. Introducción. El trastorno del espectro autista (TEA) frecuentemente presenta trastornos médicos relacionados que requieren una atención sanitaria especializada. En este sentido, los profesionales del ámbito sanitario se enfrentan a dificultades que precisan una formación específica en las necesidades sanitarias que presenta esta población. Objetivo. Cuantificar los conocimientos sobre el TEA de los profesionales sanitarios del área pediátrica y valorar el impacto de una formación en línea. Sujetos y métodos. Estudio cuasi experimental del antes y después, longitudinal y prospectivo; sujetos a estudio: profesionales sanitarios; variable independiente: formación en línea en TEA; variable dependiente: conocimiento sobre el TEA. Se llevó a cabo una formación en línea para profesionales del área de pediatría en la que se abordaron las características nucleares del diagnóstico, así como las necesidades que presentan en el contexto hospitalario y las adaptaciones que se recomiendan llevar a cabo. Participaron 58 profesionales sanitarios. Resultados. Se observó un aumento en el conocimiento sobre el TEA al finalizar la intervención (del 73,9 al 85% según el cuestionario de conocimientos previos del TEA), que mostró que más del 90% de los participantes tenía el grado máximo de conocimiento sobre el TEA. Conclusiones. Las formaciones en línea son un método para ampliar conocimiento útil y eficaz para aumentar el conocimiento sobre el TEA y las adaptaciones que se recomiendan en el ámbito hospitalario. Se recomienda aumentar la disponibilidad de formación sobre TEA en estos entornos. PubMed Disclaimer Similar articles
Publication types
Related informationLinkout - more resources, full text sources.
NCBI Literature Resources MeSH PMC Bookshelf Disclaimer The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited. Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
Early environmental predictors for attention-deficit hyperactivity disorder (ADHD), autism spectrum disorder (ASD) and their co-occurrence: The prospective ABIS-Study
Scientific Reports volume 14 , Article number: 14759 ( 2024 ) Cite this article 45 Accesses Metrics details
ADHD and ASD are highly heritable and show a high co-occurrence and persistence into adulthood. This study aimed to identify pre and perinatal risk factors, and early psychosocial exposures related to later diagnosis of ADHD, ASD, and their co-occurrence. 16,365 children born 1997–1999 and their families, involved in the prospective population-based ABIS study (All Babies in Southeast Sweden), were included in this sub-study. Pre and perinatal factors and early environmental psychosocial exposures were collected from parental-questionnaires at birth and 1-year follow-up. Diagnoses from birth up to 23 years of age were obtained from the Swedish National Diagnosis Register in 2020. The cumulative incidence of ADHD, ASD, and their co-occurrence in the ABIS-cohort Study were 4.6%, 1.7%, and 1.1%, respectively. Being male was associated with an increased risk for ADHD, ASD, and their co-occurrence (aOR 1.30, 1.56, and 1.91, respectively), while higher household income reduced it (aOR 0.82, 0.73, and 0.64). Serious life events during pregnancy (aOR 1.40) and maternal smoking (aOR 1.51) increased the risk of ADHD, while older maternal age (aOR 0.96), higher parental education (aOR 0.72 maternal and aOR 0.74 paternal) and longer exclusive breastfeeding (aOR 0.72) reduced it. Non-Swedish paternal nationality (aOR 0.40) and higher maternal education (aOR 0.74) were associated with a lower risk of ASD, while a family history of autoimmune diseases increased the risk of the co-occurrence of both disorders (aOR 1.62). Obtained results suggest that the etiology of ADHD, ASD, and their co-occurrence is independently associated with environmental psychosocial predictors. The co-occurrence seems to overlap the etiology of ADHD, in which psychosocial determinants have a larger role, however, it is also independently influenced by a family history of autoimmune diseases. Similar content being viewed by others Quantifying the relative importance of genetics and environment on the comorbidity between mental and cardiometabolic disorders using 17 million Scandinavians Mutations in the U4 snRNA gene RNU4-2 cause one of the most prevalent monogenic neurodevelopmental disorders Autism spectrum disorderIntroduction. Attention deficit hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) are the neurodevelopmental disorders (NDDs) most commonly diagnosed, with prevalence estimates of 5–10% and 1–2%, respectively 1 , 2 . Their onset occurs in childhood and is associated with significant behavioral, academic, emotional, and adaptive problems 3 . Both disorders have been considered lifelong conditions and show a substantial degree of persistence into adulthood. Males exhibit NDDs more often than females, however, the mechanisms that lead to this sexual dimorphism are only partly understood 4 . NDDs are considered highly heritable and have multiple and complex causes, including both genetic and environmental factors 5 , 6 , 7 . The etiology of ADHD includes preterm birth, low birth weight, maternal stress, alcohol use and smoking, and severe early deprivation among others 8 , 9 . Evidence suggested that low birth weight, birth complications, advanced parental age, maternal diseases, and both bacterial and viral infections, increased the risk of ASD 10 , 11 . Toxic chemical exposure such as air pollutants, heavy metals, and pesticides, were also studied 12 . It was suggested that prenatal multivitamins supplementation decreased the risk of ASD and ADHD 13 , 14 , but also longer breastfeeding was associated with a lower risk of ASD and ADHD and better cognitive development 15 . While the most studied etiological factors were primarily biological, psychosocial exposures, also recognized as autism and ADHD determinants by The WHO’s interactive biopsychosocial model (The International Classification of Functioning—ICF), have received less attention 16 . Despite the evidence that suggests that ADHD and ASD are heterogeneous in etiology, biology, presentation, and associated functional impairment 17 , 18 , it was estimated that between 30 and 50% of individuals with ASD manifest ADHD symptoms, similarly, two-thirds of individuals with ADHD show features of ASD 19 . The high co-occurrence rates between these two disorders suggests that they might share developmental pathways and risk factors 4 , most research to date has considered separate developmental trajectories, therefore little is known regarding the etiology of their co-occurrence 20 . The prospective longitudinal design of the ABIS-Study that includes a large representative sample with more than 22 years of follow-up, together with the validated register data for ADHD and ASD diagnoses, that made the loss to follow-up minimal, offers the opportunity to determine whether the two disorders share developmental trajectories and early risk factors. The current study aimed to examine pre and perinatal risk factors and early environmental psychosocial exposures, that could increase the long-term risk of developing ADHD, ASD, and the co-occurrence of both disorders. Study populationThis prospective cohort study includes data from the ABIS-Study (All Babies in Southeast Sweden), a longitudinal, population-based cohort study based on data collected from 16,365 children born between October 1997 and October 1999 in Southeast Sweden and their respective families. ABIS-Study aims to investigate how environmental and genetic factors influence the development of immune-mediated diseases, which then includes ADHD and ASD, where immune mechanisms may play a role 10 . The children included in the ABIS-Study have been followed from birth onwards, and questionnaire data, biological samples, and register data have been collected at birth and age of 1, 3, 5, 8, 10–12, 17–19, and 23–25 years. The parents were given both oral and written information before giving informed consent to participate in the study. The ABIS-study was conducted according to the Helsinki Declaration and was approved by the Research Ethics Committees at Linköping University (Dnr: LIU 287-96, LIU 321-99, LIU 2011/53-32 and LIU 2003-092), and Lund University (LU 83-97) in Sweden. Connection of the ABIS registers to National Registers was approved by the Research Ethics Committee in Linköping (Dnr 2013/253-32). All data used in this study were also anonymized. Diagnoses of ADHD, ASD, and their co-occurrenceThe diagnoses of ADHD and ASD were obtained for the entire ABIS population (n = 16,365) from birth until 2020-12-31, by cross-linking with the Swedish National Patient Register (NPR), containing all hospital inpatients (since 1973) and outpatients (since 2001) International Classification of Diseases (ICD-8 to ICD-10) based on doctor-set diagnoses 21 . According to the ICD-10, F90 (F90.0, F90.1, F90.8, and F90.9) and F84 (F84.0, F84.1, F84.2, F84.3, F84.4, F84.5, F84.8, and F84.9) were the diagnostic codes used for ADHD and ASD, respectively. Those children that got a unique diagnosis of ADHD (n = 755), those that received a unique ASD diagnosis (n = 272), and those that got both diagnoses (ADHD and ASD co-occurrence) (n = 188), according to the NPR, were defined as the groups any outcome, the rest of the study population constituted the group without any assessed outcome (n = 15,150) (Fig. 1 ).  Study population flow-chart. Definition of groups based on the cumulative incidence rates for ADHD, ASD, and their co-occurrence from birth until the age of 23 years. ADHD attention-deficit/hyperactivity disorder, ASD autism spectrum disorder. Data was collected from the questionnaires used in the ABIS-Study at birth and 1-year follow-up. Pre and perinatalMaternal disease during pregnancy was a composite measure including hypothyroidism and hyperthyroidism, B12 deficiency, systemic lupus erythematosus, adrenal insufficiency, type 1 and type 2 diabetes, gestational diabetes, celiac disease, rheumatism, and inflammatory bowel disease. Autoimmune disease heredity was dichotomized as no autoimmune heredity or at least one first-degree relative with any of the autoimmune diseases previously mentioned 22 . Infections during pregnancy, and iron and vitamins/minerals supplements use during pregnancy, were dichotomic variables. Parity was categorized in “first parity” or “previous parity”, twins (single fetus or multiple fetuses), way of delivery (vaginal, cesarean section, or other complications), gestational age, and birth weight, were also included. PsychosocialChild’s sex, maternal and paternal age at child’s birth, maternal and paternal ethnicity (born in Sweden or abroad), civil status at child’s birth (married/living with a partner or single parent), support during pregnancy, and security for mother and child were also included. Serious life events during pregnancy and at 1 year of age 23 , maternal smoking, and tobacco exposure at 1 year of age, were also included. Exclusive breastfeeding duration was categorized as “less than 4 months”, “5–8 months”, and “9 months or more”, according to WHO recommendations 24 . Maternal and paternal education was classified according to the International Standard Classification of Education (ISCED) and graded in three levels: low = ISCED level I–II, medium = ISCED level III–IV, and high = ISCED level V–VII 25 . The disposable household income for the year 2000 was obtained from the Swedish Income and Tax register and was categorized into three levels based on percentage distribution, low income (bottom quintile), medium income (second to fourth quintile), and high income (top quintile) 26 . Statistical methodsAll statistical analyses were performed in SPSS software version 28.0 (IBM SPSS Inc., Chicago, IL, USA). Dichotomous predictors were presented as frequencies and percentages, and differences were assessed using Chi-squared test, while quantitative predictors were described using mean and standard deviation, and differences between groups were assessed using t -test. A P -value ≤ 0.05 was considered statistically significant, and multiple comparisons between the groups with any assessed outcome were adjusted using Bonferroni correction (Table 1 ). Missing values were imputed via multiple imputation in which all predictor and outcome variables were employed in the imputation process which used 5 imputation samples 27 . All reported univariate and multiple multinomial logistic regression analyses were fitted to the data after multiple imputation. Identification of statistically independent discriminators used a backward elimination algorithm in which all univariately statistically significant discriminators (unadjusted model—Table 2 ) were entered into a single full model. Individual discriminators were then removed from the model in a stepwise fashion if their individual P -value was > 0.05 until all remaining discriminators were statistically significant (Multivariable model of independent predictors—Table 2 ). Automatic model selection algorithms are known to be prone to over-optimism 28 and hence we regard the final model selected as a candidate model which is in need of independent replication. Effect sizes were reported as odds ratios (OR) or adjusted odds ratios (aOR) with 95% confidence intervals (95% CI) and 2-tailed P -values. We conducted a response-bias analysis. The cumulative incidence rates for ADHD, ASD, and their co-occurrence in ABIS Study were 4.6%, 1.7%, and 1.1%, respectively, and the prevalence was higher in boys ( P < 0.001). The median (and interquartile range) of the age at first diagnosis were 16 (6) for ADHD, 17 (6) for ASD, and 13 (6) for the co-occurrence. A total of 66 children from the initial ABIS cohort died before 23 years of age, the average age (and SD) was 14.4 (7.8). ADHD predictorsThe ADHD group was characterized by a higher prevalence of family history of autoimmune diseases ( P < 0.001), a higher proportion of preterm babies (gestational age below 37 weeks) ( P = 0.019), and lower birth weight ( P = 0.024). Concerning psychosocial factors, the ADHD group was characterized by younger parents (below 25 years of age, P < 0.001), low parental education ( P < 0.001), higher proportion of single parents ( P < 0.001), low household income ( P < 0.001), higher prevalence of maternal smoking ( P < 0.001), and tobacco exposure at 1 year of age ( P < 0.001). The ADHD group also exhibited a higher proportion of serious life events during pregnancy ( P < 0.001), and shorter breastfeeding duration (less than 4 months, P < 0.001) compared to the controls, but also to the ASD group (Table 1 ). Statistically independent predictors of ADHDBeing male, lower household income, and lower maternal education, together with younger mother, maternal smoking, serious life event during pregnancy, lower paternal education, and short breastfeeding duration, were the risk factors that remain significant in the multiple multinomial logistic regression analyses (Table 2 ). ASD predictorsMaternal diseases ( P = 0.045) and infections during pregnancy ( P = 0.019) were more frequently reported by the ASD group. Cesarean sections ( P = 0.017) were reported to a lesser extent than controls and the co-occurrence group. The ASD group was also significantly associated with older mothers (above 36 years of age) compared to controls and the ADHD group. Though the ASD group showed a higher proportion of highly educated mothers and fathers than the ADHD group, they exhibited more often low maternal education level ( P < 0.001), and low household income ( P < 0.001) than the control group (Table 1 ). Statistically independent predictors of ASDBeing male, lower household income, and lower maternal education together with paternal Swedish nationality, were the risk factors that remain significant in the multiple multinomial logistic regression analyses (Table 2 ). ADHD and ASD co-occurrence predictorsThe co-occurrence group was characterized by a higher prevalence of autoimmune diseases in the family ( P < 0.001), and a higher proportion of preterm babies ( P = 0.027). Regarding psychosocial factors, this group was predominantly associated with low parental education level ( P < 0.001), single parental status ( P < 0.001), low household income ( P < 0.001), lack of support during pregnancy ( P = 0.002), and lack of security for mother and child ( P < 0.001). This group also reported maternal smoking ( P < 0.001) and serious life events at 1 year of age ( P = 0.002) to a greater extent than the control group (Table 1 ). Statistically independent predictors of the co-occurrenceBeing male, lower household income, together with a family history of autoimmune disorders remain significant in the multiple multinomial logistic regression analyses (Table 2 ). Statistically significant predictors among the three-case groupsSerious life events during pregnancy (aOR 1.78 [95% CI 1.07–2.97]), non-Swedish father (aOR 2.39 [95% CI 1.16–4.88]), maternal age (aOR 0.95 [95% CI 0.92–0.98]), exclusive breastfeeding duration (OR 0.63 [95% CI 0.43–0.94]), and paternal education level (aOR 0.70 [95% CI 0.53–0.91]), yielded significant associations with being later diagnosed with ADHD rather than ASD. Maternal age (aOR 0.96 [95% CI 0.93–0.99]) and being male (aOR 0.67 [95% CI 0.48–0.95]), provided statistically significant discrimination between ADHD and the co-occurrence group, whereas exclusive breastfeeding duration (aOR 1.4 [95% CI 1.05–1.88]) did so between ASD and the co-occurrence group. This is the first-ever prospective study considering early environmental psychosocial exposures as potential etiological factors not only for ADHD and ASD, but also for their co-occurrence. Being male was a strong and independent predictor for later development of ADHD, ASD and their co-occurrence. Previous studies have found a male-to-female ratio of 3:1 for both ADHD 29 and ASD 30 while we found a ratio of 2:1. Genetic and endocrine causes have been proposed in previous studies, however, it is also possible that, due to cultural or social expectations, females may report their ADHD symptoms less frequently or as less disabling than males, thus not meeting the diagnostic criteria 31 . Lower household income level was also independently associated with an increased risk of ADHD, ASD and their co-occurrence. Previous studies conducted in ABIS cohort and in other high-income countries, have shown marked socioeconomic inequality associated with several child health outcomes (T1D, cardiovascular risk factor and infectious diseases) 26 , 32 , 33 . On this line, previous studies found that children in families with low SES were twice as likely to have ADHD than children in high SES families 34 . Parents with ADHD diagnosis, as a background factor, could also influence both their own SES and ADHD development in their offspring 34 . According to previous studies 35 , we found that younger mothers increased the risk for ADHD in their offspring, that together with a lower education and income level could evidence socio-economic and emotional difficulties in child-rearing 36 . SES was also related to breastfeeding, as it was shown that mothers with low education levels wean earlier 37 . In our study, longer breastfeeding was associated with lower rates of ADHD, which is in line with previous studies 15 . Breastfeeding could have a protective effect since it facilitates the intimate contact between mother and child. Furthermore, breastfeeding provides long-chain polyunsaturated fatty acids (omega 3 fatty acids, PUFA) that could affect the infant’s microbiota regulating the gut-brain-axis, important for brain development 38 . Some studies showed decreased risk for ASD also, which we could not confirm 15 . We found a positive association between smoking (at pregnancy and 1 year of age) and ADHD. Smoking per se could be a biological risk factor for ADHD, but could also indicate the exposition to a vulnerable psycho-social environment. Previous studies also reported this association 9 . Some reports have also shown that maternal stress during pregnancy is a risk factor highly associated with ASD and ADHD 8 . We found an association between serious life events during pregnancy and ADHD risk, but not ASD. Many studies have shown that prenatal exposure to maternal stress was associated with abnormalities in neurodevelopment, neurocognitive function, and cerebral processing, which lead to changes in both the hypothalamic–pituitary–adrenal axis (HPA) and the autonomic nervous system 8 , 39 . The underlying genetic and biological component of ASD seems to differ from the etiology of ADHD. The role of infections and the immune system in the etiology of ASD has been widely debated 40 . We consistently found that infections during pregnancy increased the risk of ASD. Accumulating evidence suggests that the immune system and abnormal immune function, including inflammation, cytokine dysregulation, and anti-brain autoantibodies, influence the trajectory of ASD 10 . Intriguingly, we found that the children of mothers with autoimmune diseases have a higher risk for ASD. Maternal hypertension, anemia, overweight, diabetes, and several other medical conditions have been also associated with an increased risk of ASD in offspring 41 , 42 . A meta-analysis revelated that delivery complications and cesarean section are risk factors for ASD 43 , but when differentiating between ASD and the co-occurrence group, we found that cesarean delivery seems to be a protective factor for ASD. This might be explained by avoidance of brain damage and/or hypoxia of the new-born which might otherwise have happened in a vaginal delivery. A recent systematic review, evidenced, after adjustment for familial confounding, that perinatal hypoxia and respiratory stress were consistently associated with ASD 11 . Regarding the role of genetics, a study on a large cohort of Swedish children showed that the heritability of ASD is approximately 50% and the risk of ASD increases tenfold if a sibling has the disease and twofold if a cousin is diagnosed with ASD 44 . Regarding the ADHD/ASD co-occurrence seems to overlap the etiological pattern of ADHD, while the possible biological etiology of ASD tends to be obscured. There is evidence suggesting that autistic traits are common among children with ADHD, being ADHD a better predictor of the co-occurrence, rather than ASD 45 . A family history of autoimmune diseases was found to be a strong and independent factor for the co-occurrence (not each disorder separately), which may suggest that both disorders could share similar genetic or environmental background. Common immune-mediated diseases such as asthma and eczema have repeatedly been linked to ADHD 46 , 47 , 48 , similarly, ADHD has been related to autoimmune diseases, such as celiac disease, ulcerative colitis, psoriasis, ankylosing spondylitis and T1D 47 , 49 . It was suggested that the co-occurrence is associated with greater impairment, increased severity of psychosocial problems, and may be less responsive to standard treatments for either disorder 20 . Strengths and limitationsAlthough our results are based on a large prospective birth cohort from the general population with a follow-up for more than 20 years and the strength of merging doctor-set diagnoses of ADHD and ASD via the National Diagnosis Register, our study has some limitations. The family history of ADHD and ASD diagnoses was not possible to obtain. The lack of explicit criteria for ADHD and ASD co-occurrence could lead to variability in diagnosis and may have contributed to under-recognition or misdiagnosis of this comorbidity. Most data are based on questionnaires answered by the parents, usually the mothers, therefore there is a risk of recall bias. We have validated several data against information registered in the journals of Well Baby Clinics with good agreement, and there is no reason to believe that such registers have a systematic misdistribution that would influence our results. There are dropouts from birth to one year of age, but the remaining ABIS population is still representative of the general population. Thus, in summary, we believe that our results are robust and representative of the Swedish population. Our study includes pre and perinatal, and early environmental psychosocial exposures as etiological factors of ADHD, ASD, and their co-occurrence in a long-term prospective follow-up of a general population-based birth cohort. Observed associations suggest a genetic and biological component underlying ASD, and a larger role of environmental psychosocial factors in ADHD etiology. The co-occurrence seems to overlap the etiology of ADHD but is also influenced by a family history of autoimmune diseases. This study shed light on the factors that may confer risk for the expression and/or diagnosis of ADHD, ASD and their co-occurrence and despite these factors are not necessarily causal, may constitute important incentives for preventive measures in child health. Data availabilityDeidentified participant data can be shared for a specified purpose, after approval by Johnny Ludvigsson ([email protected]) through a signed data access agreement. Polanczyk, G. V., Willcutt, E. G., Salum, G. A., Kieling, C. & Rohde, L. A. ADHD prevalence estimates across three decades: An updated systematic review and meta-regression analysis. Int. J. Epidemiol. 43 (2), 434–442. https://doi.org/10.1093/ije/dyt261 (2014). Article PubMed PubMed Central Google Scholar Baio, J. et al. Prevalence of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2014 [published correction appears in MMWR Morb Mortal Wkly Rep. 2018 May 18;67(19):564] [published correction appears in MMWR Morb Mortal Wkly Rep. 2018 Nov 16;67(45):1280]. MMWR Surveill. Summ. 67 (6), 1–23. https://doi.org/10.15585/mmwr.ss6706a1 (2018). Rao, P. A. & Landa, R. J. Association between severity of behavioral phenotype and comorbid attention deficit hyperactivity disorder symptoms in children with autism spectrum disorders. Autism 18 (3), 272–280. https://doi.org/10.1177/1362361312470494 (2014). Article PubMed Google Scholar Johnson, M. H., Gliga, T., Jones, E. & Charman, T. Annual research review: Infant development, autism, and ADHD–early pathways to emerging disorders. J. Child Psychol. Psychiatry 56 (3), 228–247. https://doi.org/10.1111/jcpp.12328 (2015). Taylor, M. J. et al. Association of genetic risk factors for psychiatric disorders and traits of these disorders in a Swedish population twin sample. JAMA Psychiatry 76 (3), 280–289. https://doi.org/10.1001/jamapsychiatry.2018.3652 (2019). Posthuma, D. & Polderman, T. J. What have we learned from recent twin studies about the etiology of neurodevelopmental disorders?. Curr. Opin. Neurol. 26 (2), 111–121. https://doi.org/10.1097/WCO.0b013e32835f19c3 (2013). Herbert, M. R. Contributions of the environment and environmentally vulnerable physiology to autism spectrum disorders. Curr. Opin. Neurol. 23 (2), 103–110. https://doi.org/10.1097/WCO.0b013e328336a01f (2010). Article MathSciNet PubMed Google Scholar Van den Bergh, B. R. H. et al. Prenatal developmental origins of behavior and mental health: The influence of maternal stress in pregnancy. Neurosci. Biobehav. Rev. 117 , 26–64. https://doi.org/10.1016/j.neubiorev.2017.07.003 (2020). Nakamura, A., François, O. & Lepeule, J. Epigenetic alterations of maternal tobacco smoking during pregnancy: A narrative review. Int. J. Environ. Res. Public Health 18 (10), 5083. https://doi.org/10.3390/ijerph18105083 (2021). Bölte, S., Girdler, S. & Marschik, P. B. The contribution of environmental exposure to the etiology of autism spectrum disorder. Cell. Mol. Life Sci. 76 (7), 1275–1297. https://doi.org/10.1007/s00018-018-2988-4 (2019). Article CAS PubMed Google Scholar Carlsson, T., Molander, F., Taylor, M. J., Jonsson, U. & Bölte, S. Early environmental risk factors for neurodevelopmental disorders—A systematic review of twin and sibling studies. Dev. Psychopathol. 33 (4), 1448–1495. https://doi.org/10.1017/S0954579420000620 (2021). Scattolin, M. A. A., Resegue, R. M. & Rosário, M. C. D. The impact of the environment on neurodevelopmental disorders in early childhood. J. Pediatr. (Rio J.) 98 (Suppl 1), S66–S72. https://doi.org/10.1016/j.jped.2021.11.002 (2022). Levine, S. Z. et al. Association of maternal use of folic acid and multivitamin supplements in the periods before and during pregnancy with the risk of autism spectrum disorder in offspring. JAMA Psychiatry 75 (2), 176–184. https://doi.org/10.1001/jamapsychiatry.2017.4050 (2018). Raghavan, R. et al. Maternal multivitamin intake, plasma folate and vitamin B 12 levels and autism spectrum disorder risk in offspring. Paediatr. Perinat. Epidemiol. 32 (1), 100–111. https://doi.org/10.1111/ppe.12414 (2018). Bar, S., Milanaik, R. & Adesman, A. Long-term neurodevelopmental benefits of breastfeeding. Curr. Opin. Pediatr. 28 (4), 559–566. https://doi.org/10.1097/MOP.0000000000000389 (2016). Bölte, S., Lawson, W. B., Marschik, P. B. & Girdler, S. Reconciling the seemingly irreconcilable: The WHO’s ICF system integrates biological and psychosocial environmental determinants of autism and ADHD: The International Classification of Functioning (ICF) allows to model opposed biomedical and neurodiverse views of autism and ADHD within one framework. Bioessays 43 (9), e2000254. https://doi.org/10.1002/bies.202000254 (2021). Thapar, A., Cooper, M. & Rutter, M. Neurodevelopmental disorders. Lancet Psychiatry 4 (4), 339–346. https://doi.org/10.1016/S2215-0366(16)30376-5 (2017). Lombardo, M. V., Lai, M. C. & Baron-Cohen, S. Big data approaches to decomposing heterogeneity across the autism spectrum. Mol. Psychiatry 24 (10), 1435–1450. https://doi.org/10.1038/s41380-018-0321-0 (2019). Russell, G., Rodgers, L. R., Ukoumunne, O. C. & Ford, T. Prevalence of parent-reported ASD and ADHD in the UK: Findings from the Millennium Cohort Study. J. Autism Dev. Disord. 44 (1), 31–40. https://doi.org/10.1007/s10803-013-1849-0 (2014). Leitner, Y. The co-occurrence of autism and attention deficit hyperactivity disorder in children—What do we know?. Front. Hum. Neurosci. 8 , 268. https://doi.org/10.3389/fnhum.2014.00268 (2014). Ludvigsson, J. F. et al. Registers of the Swedish total population and their use in medical research. Eur. J. Epidemiol. 31 (2), 125–136. https://doi.org/10.1007/s10654-016-0117-y (2016). Ji, J., Ludvigsson, J. F., Sundquist, K., Sundquist, J. & Hemminki, K. Incidence of celiac disease among second-generation immigrants and adoptees from abroad in Sweden: Evidence for ethnic differences in susceptibility. Scand. J. Gastroenterol. 46 (7–8), 844–848. https://doi.org/10.3109/00365521.2011.579999 (2011). Nygren, M., Carstensen, J., Koch, F., Ludvigsson, J. & Frostell, A. Experience of a serious life event increases the risk for childhood type 1 diabetes: The ABIS population-based prospective cohort study. Diabetologia 58 (6), 1188–1197. https://doi.org/10.1007/s00125-015-3555-2 (2015). World Health Organization. Infant and young child nutrition. 54th World Health Assembly (WHA 54.2) (WHO, 2001). Google Scholar UIS. International Standard Classification of Education ISCED 2011 (UNESCO Institute for Statistics, 2012). White, P. A., Faresjö, T., Jones, M. P. & Ludvigsson, J. Low maternal education increases the risk of Type 1 Diabetes, but not other autoimmune diseases: A mediating role of childhood BMI and exposure to serious life events. Sci. Rep. 13 (1), 6166. https://doi.org/10.1038/s41598-023-32869-x (2023). Article ADS CAS PubMed PubMed Central Google Scholar Marti, H. & Chavance, M. Multiple imputation analysis of case-cohort studies. Stat. Med. 30 (13), 1595–1607. https://doi.org/10.1002/sim.4130 (2011). Steyerberg, E. W., Bleeker, S. E., Moll, H. A., Grobbee, D. E. & Moons, K. G. Internal and external validation of predictive models: A simulation study of bias and precision in small samples. J. Clin. Epidemiol. 56 (5), 441–447. https://doi.org/10.1016/s0895-4356(03)00047-7 (2003). Bruchmüller, K., Margraf, J. & Schneider, S. Is ADHD diagnosed in accord with diagnostic criteria? Overdiagnosis and influence of client gender on diagnosis. J. Consult. Clin. Psychol. 80 (1), 128–138. https://doi.org/10.1037/a0026582 (2012). Loomes, R., Hull, L. & Mandy, W. P. L. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. J. Am. Acad. Child Adolesc. Psychiatry 56 (6), 466–474. https://doi.org/10.1016/j.jaac.2017.03.013 (2017). Davies, W. Sex differences in attention Deficit Hyperactivity Disorder: Candidate genetic and endocrine mechanisms. Front. Neuroendocrinol. 35 (3), 331–346. https://doi.org/10.1016/j.yfrne.2014.03.003 (2014). Spencer, N. J. et al. Household income and maternal education in early childhood and activity-limiting chronic health conditions in late childhood: findings from birth cohort studies from six countries [published online ahead of print, 2022 Jul 21]. J. Epidemiol. Community Health https://doi.org/10.1136/jech-2022-219228 (2022). Spencer, N. J. et al. Social gradients in ADHD by household income and maternal education exposure during early childhood: Findings from birth cohort studies across six countries. PLoS One 17 (3), e0264709. https://doi.org/10.1371/journal.pone.0264709 (2022). Article CAS PubMed PubMed Central Google Scholar Reiss, F. et al. Socioeconomic status, stressful life situations and mental health problems in children and adolescents: Results of the German BELLA cohort-study. PLoS One 14 (3), e0213700. https://doi.org/10.1371/journal.pone.0213700 (2019). Min, X., Li, C. & Yan, Y. Parental age and the risk of ADHD in offspring: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 18 (9), 4939. https://doi.org/10.3390/ijerph18094939 (2021). Hackman, D. A., Farah, M. J. & Meaney, M. J. Socioeconomic status and the brain: Mechanistic insights from human and animal research. Nat. Rev. Neurosci. 11 (9), 651–659. https://doi.org/10.1038/nrn2897 (2010). Flacking, R., Wallin, L. & Ewald, U. Perinatal and socioeconomic determinants of breastfeeding duration in very preterm infants. Acta Paediatr. 96 (8), 1126–1130. https://doi.org/10.1111/j.1651-2227.2007.00386.x (2007). Cenit, M. C., Nuevo, I. C., Codoñer-Franch, P., Dinan, T. G. & Sanz, Y. Gut microbiota and attention deficit hyperactivity disorder: New perspectives for a challenging condition. Eur. Child Adolesc. Psychiatry 26 (9), 1081–1092. https://doi.org/10.1007/s00787-017-0969-z (2017). Angelidou, A. et al. Perinatal stress, brain inflammation and risk of autism-review and proposal. BMC Pediatr. 12 , 89. https://doi.org/10.1186/1471-2431-12-89 (2012). Meltzer, A. & Van de Water, J. The role of the immune system in autism spectrum disorder. Neuropsychopharmacology 42 (1), 284–298. https://doi.org/10.1038/npp.2016.158 (2017). Rivera, H. M., Christiansen, K. J. & Sullivan, E. L. The role of maternal obesity in the risk of neuropsychiatric disorders. Front. Neurosci. 9 , 194. https://doi.org/10.3389/fnins.2015.00194 (2015). Maher, G. M. et al. Association of hypertensive disorders of pregnancy with risk of neurodevelopmental disorders in offspring: A systematic review and meta-analysis. JAMA Psychiatry 75 (8), 809–819. https://doi.org/10.1001/jamapsychiatry.2018.0854 (2018). Zhang, T. et al. Association of cesarean delivery with risk of neurodevelopmental and psychiatric disorders in the offspring: A systematic review and meta-analysis. JAMA Netw. Open 2 (8), e1910236. https://doi.org/10.1001/jamanetworkopen.2019.10236 (2019). Sandin, S. et al. The familial risk of autism. JAMA 311 (17), 1770–1777. https://doi.org/10.1001/jama.2014.4144 (2014). Tistarelli, N., Fagnani, C., Troianiello, M., Stazi, M. A. & Adriani, W. The nature and nurture of ADHD and its comorbidities: A narrative review on twin studies. Neurosci. Biobehav. Rev. 109 , 63–77. https://doi.org/10.1016/j.neubiorev.2019.12.017 (2020). Muskens, J. B., Velders, F. P. & Staal, W. G. Medical comorbidities in children and adolescents with autism spectrum disorders and attention deficit hyperactivity disorders: A systematic review. Eur. Child Adolesc. Psychiatry 26 (9), 1093–1103. https://doi.org/10.1007/s00787-017-1020-0 (2017). Chen, M. H. et al. Comorbidity of allergic and autoimmune diseases among patients with ADHD. J. Atten. Disord. 21 (3), 219–227. https://doi.org/10.1177/1087054712474686 (2017). Cortese, S. et al. Association between attention deficit hyperactivity disorder and asthma: A systematic review and meta-analysis and a Swedish population-based study. Lancet Psychiatry 5 (9), 717–726. https://doi.org/10.1016/S2215-0366(18)30224-4 (2018). Nielsen, P. R., Benros, M. E. & Dalsgaard, S. Associations between autoimmune diseases and attention-deficit/hyperactivity disorder: A nationwide study. J. Am. Acad. Child Adolesc. Psychiatry 56 (3), 234-240.e1. https://doi.org/10.1016/j.jaac.2016.12.010 (2017). Download references AcknowledgementsWe are grateful to all the participating families who take part in ABIS ongoing cohort study and all the staff at Obstetric Department and Well-Baby Clinics. Open access funding provided by Linköping University. ABIS-study has received funding from the County Council of Östergötland, Swedish Research Council (K2005-72X-11242-11A and K2008-69X-20826-01-4), Swedish Child Diabetes Foundation (Barndiabetesfonden), Juvenile Diabetes Research Foundation, Wallenberg Foundation (K 98-99D-12813-01A), Medical Research Council of Southeast Sweden (FORSS), Swedish Council for Working Life and Social Research (FAS2004–1775), Östgöta Brandstodsbolag, and Joanna Cocozza Foundation. Author informationAuthors and affiliations. Division of Pediatrics, Department of Biomedical and Clinical Sciences, Linköping University, US Campus, Building 511 (14, 09B), 581 83, Linköping, Sweden Andrea Lebeña & Johnny Ludvigsson Department of Medicine and Health, Community Medicine, Linköping University, Linköping, Sweden Åshild Faresjö, Felicia Bengtsson & Tomas Faresjö School of Psychological Sciences, Macquarie University, North Ryde, NSW, Australia Michael P. Jones Crown Princess Victoria Children’s Hospital, Region Östergötland, Linköping, Sweden Johnny Ludvigsson You can also search for this author in PubMed Google Scholar ContributionsJ.L. created and still leads the ABIS study. J.L. collected all data, supporting this study, including funding acquisition. Å.F. and T.F. led the design of the study. A.L. and J.L. wrote the initial and final drafts of the manuscript. M.P.J., A.L., and F.B. performed the statistical analyses. All authors contributed to the interpretation of findings, critical revisions, and redrafting of the manuscript. The first and last authors (the manuscript’s guarantors) affirm that the manuscript is an honest, accurate, and transparent account of the study being reported and that no important aspects of the study have been omitted. All authors have confirmed the final version of the manuscript. Corresponding authorCorrespondence to Andrea Lebeña . Ethics declarationsCompeting interests. The authors declare no competing interests. Additional informationPublisher's note. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Rights and permissionsOpen Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . Reprints and permissions About this articleCite this article. Lebeña, A., Faresjö, Å., Jones, M.P. et al. Early environmental predictors for attention-deficit hyperactivity disorder (ADHD), autism spectrum disorder (ASD) and their co-occurrence: The prospective ABIS-Study. Sci Rep 14 , 14759 (2024). https://doi.org/10.1038/s41598-024-65067-4 Download citation Received : 21 August 2023 Accepted : 17 June 2024 Published : 26 June 2024 DOI : https://doi.org/10.1038/s41598-024-65067-4 Share this articleAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate. Quick links
Sign up for the Nature Briefing: Anthropocene newsletter — what matters in anthropocene research, free to your inbox weekly.  | ||||
COMMENTS
Learn about autism spectrum disorder (ASD), a neurological and developmental disorder that affects how people interact, communicate, and behave. Find out how ASD is diagnosed, what are the signs and symptoms, and what are the causes and risk factors.
Learn about the legal rights and educational options for children with Autism under IDEA. Find out how to develop and implement an Individualized Education Program (IEP) that meets your child's needs and goals.
Autism spectrum disorder is a condition related to brain development that impacts how a person perceives and socializes with others, causing problems in social interaction and communication. The disorder also includes limited and repetitive patterns of behavior. The term "spectrum" in autism spectrum disorder refers to the wide range of ...
CDC activities help us better understand autism spectrum disorder (ASD) and help support people with. Skip directly to site content Skip directly to search. ... call your local elementary school or board of education and ask to speak with someone who can help you have your child evaluated. If you're not sure who to contact, call the ECTA at 919 ...
Autism spectrum disorder (ASD) refers to a group of complex neurodevelopment disorders caused by differences in the brain that affect communication and behavior. The term "spectrum" refers to the wide range of symptoms, skills, and levels of ability in functioning that can occur in people with ASD.
Teacher needs for educating children with autism spectrum disorders in the general education classroom. Journal of Special Education Apprenticeship, 2(2). Google Scholar *Frederickson N., Jones A. P., Lang J. (2010). Inclusive provision options for pupils on the autistic spectrum. ... Research in Autism Spectrum Disorders, 6(3), 1156-1167 ...
Children with autism are guaranteed free, appropriate public education under the federal laws of Public Law 108-177: Individuals with Disabilities Education Improvement Act (2004), sometimes called "IDEA." IDEA ensures that children diagnosed with certain disabilities or conditions, including autism spectrum disorder (ASD), get free educational services and educational devices to help them to ...
Autism - also referred to as autism spectrum disorder ̶ constitutes a diverse group of conditions related to development of the brain. About 1 in 100 children has autism. Characteristics may be detected in early childhood, but autism is often not diagnosed until much later. The abilities and needs of autistic people vary and can evolve over ...
The fourth edition of Autism Spectrum Disorders: Identification, Education, and Treatment provides current and prospective professionals and researchers with a timely update of issues relevant to the field of autism. This new edition describes up-to-date trends and issues critical for the treatment of children, adolescents, and young adults with autism spectrum disorder (ASD).
Autism spectrum disorder (ASD) is a developmental disorder that afects communication and behavior. Although autism can be diagnosed at any age, it is described as a "developmental disorder" because symptoms generally appear in the first two years of life. Autism is known as a "spectrum" disorder because there is wide variation in the ...
Current treatments for autism spectrum disorder (ASD) seek to reduce symptoms that interfere with daily functioning and quality of life. Treatments can be given in education, health, community, or home settings, or a combination of settings.
Autism is one of the most common developmental disabilities. People with autism, also called autism spectrum disorder (ASD), have differences in the way their brains develop and process information. As a result, they face significant communication, social, and behavior challenges. Symptoms can be severe and interfere with everyday tasks, or ...
What Are the Autism Spectrum Disorders? The autism spectrum disorders are more common in the pediatric population than are some better known disorders such as diabetes, spinal bifida, or Down syndrome. 2 Prevalence studies have been done in several states and also in the United Kingdom, Europe, and Asia. Prevalence estimates range from 2 to 6 per 1,000 children.
Developmental Milestones. Your child should reach milestones in how he plays, learns, speaks and acts. A delay in any of these areas could be a sign of a developmental problem, even autism. Visit our webpage to see milestones that children should reach from 2 months to 5 years of age, plus interactive tools to help keep track of the ...
Autism spectrum disorder (ASD) is a lifelong condition characterised by social communication difficulties and repetitive behaviours (American Psychiatric Association Citation 2013).The standardised prevalence is around 1.76% of children within schools in England (Roman-Urrestarazu et al. Citation 2021); and there is a high incidence of mental health difficulties (Murphy et al. Citation 2016).
In addition to autism spectrum disorder, children, teens and adults can also experience: Medical health issues. Children with autism spectrum disorder may also have medical issues, such as epilepsy, sleep disorders, limited food preferences or stomach problems. Ask your child's doctor how to best manage these conditions together.
This brochure presents information about autism spectrum disorder (ASD) including signs and symptoms, causes and risk factors, diagnosis in young children, older children, teens, and adults, and treatments. ... The school's special education team may perform an initial evaluation and then recommend that a child undergo additional evaluation ...
Autism spectrum disorder (ASD) is a developmental disability that affects how a person interacts with the world. It can cause difficulties with socializing, communicating, and behavior. The term "spectrum" refers to the wide range of symptoms and behaviors a person might have. In 2013, the criteria used to diagnose ASD and the names of some ...
Autism spectrum disorder has two core features doctors use to make a diagnosis: social communication differences or difficulties and specific or repetitive interests and behaviors. Among autistic people, there is a wide variation of traits, strengths, and support needs. ... Early Intervention and Education for Autism Spectrum Disorder - A ...
Special education services can curb some of these problems. ... 2023 in Women with Autism Spectrum Disorder. ... Positive reinforcement is an evidence-based intervention for children on the autism ...
Autism spectrum disorder (ASD) is a neurological and developmental disorder that afects how people interact with others, communicate, learn, and behave. Although autism can be diagnosed at any age, it is described as a "developmental disorder" because symptoms generally appear in the first two years of life. Autism is known as a "spectrum ...
Students with Autism Spectrum Disorders sometimes have high levels of anxiety and stress, particularly in social environments like school. If a student exhibits aggressive or explosive behavior, it is important for educational teams to recognize the impact of stress and anxiety. Preparing students for new situations, such as through writing ...
Autism spectrum disorder; Traumatic brain injury; Other health impairments; Specific learning disabilities; ... Individualized education program (IEP) — this document is the foundation of special education and specifically describes the services to be provided to the student with a disability. The IEP includes a description of a student's ...
Autism and pervasive developmental disorders sourcebook : basic consumer health information about autism spectrum disorders (ASD) including autistic disorder, asperger syndrome, rett syndrome, childhood disintegrative disorder, and pervasive developmental disorder not otherwise specified (PDDNOS) : along with facts about causes, symptoms, assessment, interventions, treatments, and education ...
Children with autism spectrum disorder (ASD) exhibit deficits in social interaction and communication, show repetitive behaviours, and have restricted interests. They are at high risk of developing challenging behaviours, which can hinder social relationships, academic achievement, language skills, overall adaptive development, and also ...
Autism Spectrum Disorder, or autism, is a disability that is often present early in life and can affect multiple aspects of a child's development. Individuals with autism do not look ... Special Education and Related Services) agreeing to Part B services The IEP team which includes the parent will develop the IEP.
Self-monitoring (SM) is a widely used intervention to address a myriad of problem behaviors exhibited by individuals with autism spectrum disorder (ASD) and other disabilities (e.g., specific learning disability). SM of performance (SMP) interventions have been effective in increasing task completion and on-task behaviors in the general education setting. However, most of the research on SM ...
Digital Shareables on Autism Spectrum Disorder. Use these resources to raise awareness about autism spectrum disorder. Autism spectrum disorder (ASD) is a neurological and developmental disorder that affects how people interact with others, communicate, learn, and behave. For more information on signs and symptoms, causes and risk factors ...
Introduction: Autism spectrum disorder (ASD) often presents related medical disorders that require specialised healthcare. Professionals in the health sector therefore face difficulties that require specific training in the healthcare needs of this population. Aim ...
Attention deficit hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) are the neurodevelopmental disorders (NDDs) most commonly diagnosed, with prevalence estimates of 5-10% and 1 ...