Account Management
Log in to manage your policy, generate a certificate of insurance (COI), make a payment, and more.
Log in to your account to update your information or manage your policy.
Download a Certificate of Insurance (COI) to provide to your employer.
Make a Payment
Make a one-time payment, set up autopay, or update your payment information.
Submit a notice of an incident or claim in just minutes.
Topics on this page:

What Is an Incident Report?
What’s the purpose of an incident report, what classifies as an ‘incident’ that would prompt a report, what information do you put in an incident report, 6 tips for writing an effective incident report, how to write a nurse incident report.
Jul 24, 2024

If you dread writing incident reports, you might take comfort in knowing that you’re not alone. Stressing over getting the report done or about what to include are common concerns for nurses — not to mention worrying about whether filing the report reflects badly on your performance. Mistakes happen all the time, and healthcare facilities are not immune. According to a 2016 study conducted by Johns Hopkins , medical errors have become the third-leading cause of death in the U.S. and threaten the safety and well-being of patients. As time-consuming as incident reports may be, their role in patient care cannot be ignored.
An incident report is an electronic or paper document that provides a detailed, written account of the chain of events leading up to and following an unforeseen circumstance in a healthcare setting. The incident doesn’t have to have caused harm to a patient, employee, or visitor, but it’s classified as an “incident” because it threatens patient safety.
To ensure the details are as accurate as possible, incident reports should be completed within 24 hours by whomever witnessed the incident. If the incident wasn’t observed (e.g., a patient slipped, fell, and got up on his own), then the first person who was notified should submit it. For the most part, these incident reports are completed by nurses or other licensed personnel and are used for risk management, quality assurance, educational, and legal purposes .

Incident reports are used to communicate important safety information to hospital administrators and keep them updated on aspects of patient care for the following purposes:
- Risk management . Incident report data is used to identify and eliminate potential risks necessary to prevent future mistakes. For example, if an incident report review finds that most medical errors occur during shift changes, risk management teams may suggest that nursing staff develop standardized turnover protocols to avoid future errors.
- Quality assurance. Quality assurance is all about patient safety, customer satisfaction, and improving healthcare quality. Quality control groups comb through incident reports to look for indicators that suggest a patient received high-quality, patient-centered care at a reasonable price.
- Educational tools. Incident reports make great training tools because everyone has an innate ability to learn from their mistakes — or the mistakes of others. Healthcare teams often use resolved incident reports as educational tools to prevent similar occurrences.
Be aware that because incident reports could potentially be used for legal purposes, providing incomplete, inaccurate, or false documentation in an incident report can harm patients and jeopardize the defense of any case — including your own.
In most circumstances, nurses are required to complete an incident report whenever they witness a reportable event or are notified that one has occurred. What constitutes a reportable event may vary by organization and practice setting, but the New York State Department of Health has identified some of the most common types:
- Examples: adverse reactions, equipment failure or misuse, medication errors
- Examples: assaults, burns, falls, needle sticks
- Examples: complaints, elopement (i.e., the patient leaves without authorization), treatment refusal
- Example: potential for an error existed but was corrected before it occurred
Consider the following examples as situations in which an incident report should be filed:
- You’re working as a nurse on an acute inpatient psych unit when one of the patients begins to act violently and attacks a staff member or another patient.
- You’re ambulating a patient in the hallway and securely holding onto their gait belt when the patient abruptly falls to their knees before you had a chance to react.
- You’re interviewing a clinic patient who passes out and falls from the examination table onto the floor without warning. Upon awakening, the patient appears to be fine but passes out again a few minutes later. Emergency medical services are called to respond.
According to RegisteredNursing.org , the information in an incident report should always include the who, what, when, where, and how, and — at the very least — the following pertinent information:
- Date, time, and facility location
- Where the incident occurred
- Incident type
- Name of the person(s) affected by the incident
- Witnesses or names and titles of other involved persons
- Detailed description of the event with events listed chronologically
- Witnesses or injured party statements
- Injuries sustained by the person(s) as a result of the incident or the outcome
- Actions taken immediately after the incident occurred
- Treatments administered
- Contributing factors
- Name(s) of who was notified (i.e., doctor, supervisor)
- Recommendations for change to prevent future incidents
Incident reports come in several formats. Typical incident report form examples include clinical events and employee – related work injuries .
Now that we know how important these incident reports are, here are six tips to consider to make sure you write a detailed and effective report, as outlined by healthcare regulation and compliance company HCPro .
Tip #1: Make sure it is clear, concise, and accurate.
Tip #2: use proper grammar, punctuation, and spelling., tip #3: state facts objectively and avoid making assumptions or casting blame..
For example:
- Write this: “The patient, who typically uses a cane, was walking down the hall when he slipped on the wet floor. The patient was not using his cane at the time of the fall.”
- Not this: “The patient was walking too fast down the hall and slipped. He should have been using his cane.”
Tip #4: Provide a chronological sequence of events.
- 12:05, Rob from Environmental Services finished mopping the floor. A “Caution: Slippery When Wet” sign was displayed.
- 12:15, Simon fell on the floor.
- 12:15, Nurses were called.
- 12:16, Charge nurse Mary arrived first and assessed the patient.
Tip #5: Include direct quotations made by witnesses or the injured party, if applicable.
Provide full names of these witnesses in case they are needed later.
Tip #6: Start the writing process early or take notes shortly after to remember key details.
Evernote is recognized as one of the best note-taking apps for healthcare providers. Microsoft One N ote , Notability , and Simplenote are good options, as well.
Organizational and practice setting requirements may vary. Regardless of your nursing background, or whether you’re working at a hospital, clinic, or other healthcare center, it’s your responsibility to follow the incident reporting guidelines established by your facility.
Image courtesy of iStock.com/ Shuttermon
Last updated on Jul 24, 2024. Originally published on Nov 30, 2018.
- Career Growth
The views expressed in this article are those of the author and do not necessarily reflect those of Berxi™ or Berkshire Hathaway Specialty Insurance Company. This article (subject to change without notice) is for informational purposes only, and does not constitute professional advice. Click here to read our full disclaimer
The product descriptions provided here are only brief summaries and may be changed without notice. The full coverage terms and details, including limitations and exclusions, are contained in the insurance policy. If you have questions about coverage available under our plans, please review the policy or contact us at 833-242-3794 or [email protected] . “20% savings” is based on industry pricing averages.
Berxi™ is a part of Berkshire Hathaway Specialty Insurance ( BHSI ). Insurance products are distributed through Berkshire Hathaway Global Insurance Services, California License # 0K09397. BHSI is part of Berkshire Hathaway’s National Indemnity group of insurance companies, consisting of National Indemnity and its affiliates, which hold financial strength ratings of A++ from AM Best and AA+ from Standard & Poor’s. The rating scales can be found at www.ambest.com and www.standardandpoors.com , respectively.
No warranty, guarantee, or representation, either expressed or implied, is made as to the correctness, accuracy, completeness, adequacy, or sufficiency of any representation or information. Any opinions expressed herein are subject to change without notice.
The information on this web site is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment, and does not purport to establish a standard of care under any circumstances. All content, including text, graphics, images and information, contained on or available through this web site is for general information purposes only based upon the information available at the time of presentation, and does not constitute medical, legal, regulatory, compliance, financial, professional, or any other advice.
BHSI makes no representation and assumes no responsibility or liability for the accuracy of information contained on or available through this web site, and such information is subject to change without notice. You are encouraged to consider and confirm any information obtained from or through this web site with other sources, and review all information regarding any medical condition or treatment with your physician or medical care provider. NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING THAT YOU HAVE READ ON OR ACCESSED THROUGH THIS WEB SITE.
BHSI is not a medical organization, and does not recommend, endorse or make any representation about the efficacy, appropriateness or suitability of any specific tests, products, procedures, treatments, services, opinions, health care providers or other information contained on or available through this web site. BHSI IS NOT RESPONSIBLE FOR, AND EXPRESSLY DISCLAIMS ALL LIABILITY FOR, ANY ADVICE, COURSE OF TREATMENT, DIAGNOSIS OR ANY OTHER SERVICES OR PRODUCTS THAT YOU OBTAIN AFTER REVIEWING THIS WEB SITE.
Want Berxi articles delivered straight to your inbox? Sign up for our monthly newsletter below!
" * " indicates required fields
How we use your email address Berxi will not sell or rent your email address to third parties unless otherwise notified. Other than where necessary to administer your insurance policy or where required by law, Berxi will not disclose your email address to third parties. Your email address is required to identify you for access to the Berxi website. You may also receive newsletters, product updates, and communications about quotes and policies.

Nichole L. Cosgrove, MSN, APRN, FNP-C is a contributing writer for Berxi. She is a family nurse practitioner currently specializing in pain management with a background in mental health nursing and a recreational medical freelance writer. Nichole lives in rural Nebraska with her husband, teenage son, and their family cat, and they have an “adopted” daughter who lives in Germany that they welcomed into their family when she was a visiting exchange student. She loves Husker football, Chicago Cubs baseball, and movies with thriller and horror genres being her favorite.
Related Articles

The 7 Most Common Nursing Mistakes (And What You Can Do If You Make One)
Paul Dughi Aug 28, 2024

Real-Life Nursing Malpractice Case: One NP Shares Her Experience of Being Sued
Robyn Correll, MPH Jul 24, 2024

What Is Supplemental Malpractice Insurance?
Berxi Editorial Team Jul 24, 2024

Nursing Incident Report
Incident report generator.
Nurses are no strangers when it comes to incidents that happen in and out of the hospital. Whether they go to work, coming from work or in the middle of work, it would seem incidents follow them. Whoever and wherever it may be, places like hospitals can be considered hotspots for incidents to happen. It goes without saying, anything and anywhere incidents or accidents can come and can happen to just about anyone. Whether these incidents are mild or severe, there is no guarantee it could get worse or it could stop altogether on its own. But rather than turning a blind eye on these kinds of problems, it is always important to file for an incident report.
Especially if you or your patients are going to be victims of the incident. To keep everyone safe from any issues or risks that go with it, incident reports should be a priority especially for those who are working in health care or medical fields. You may wonder what to expect in an incident report, and what can be filled out in it. As well as who can you give the incident report to when it is time to pass it. For answers, you should go and scroll what an incident report is and how to write them.
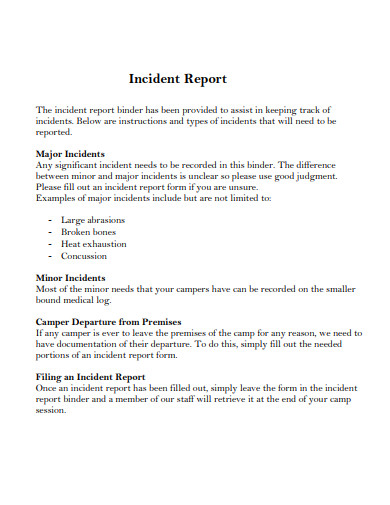
11+ Nursing Incident Report Examples
1. school nurse incident report.
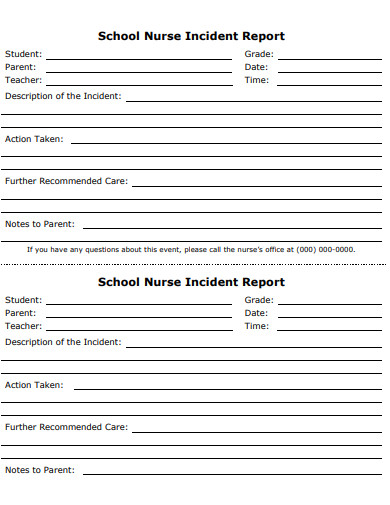
Size: 56 KB
2. Nursing Incidents of Violence Report
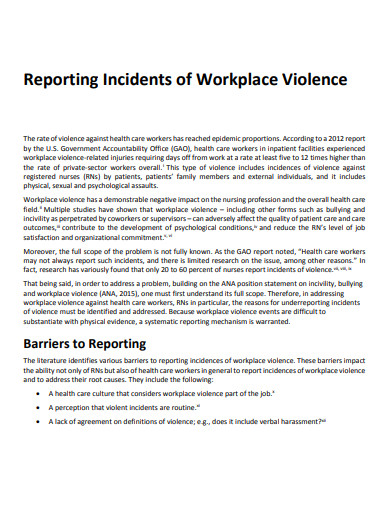
Size: 236 KB
3. Printable Nursing Incident Report
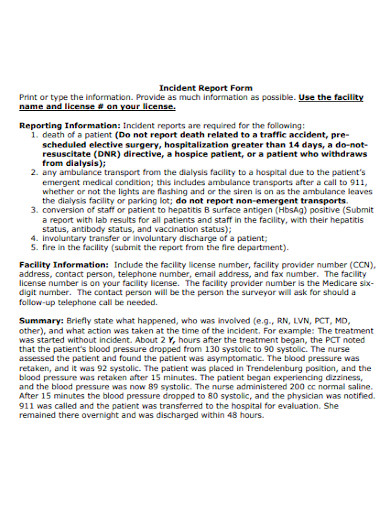
Size: 482 KB
4. Nursing Student Incident Action Report
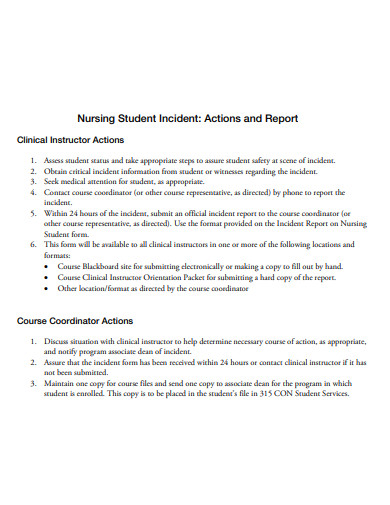
Size: 36 KB
5. Nursing Officer Incident Report
Size: 184 KB
6. Nursing Station Incident Report
Size: 244 KB
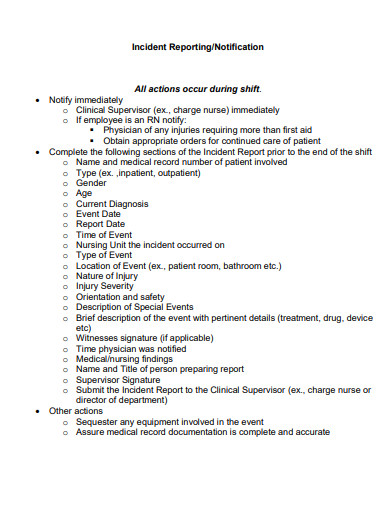
7. Staff Nurse Incident Reporting
Size: 142 KB
8. Nurse Injury Incident Report
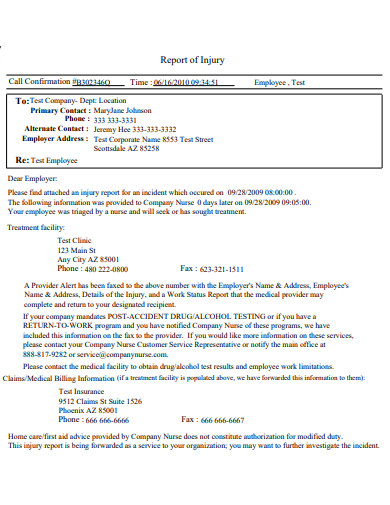
Size: 18 KB
9. Nurses and Physicians Incident Report
Size: 279 KB
10. Nurses Short Staffing Incident Report
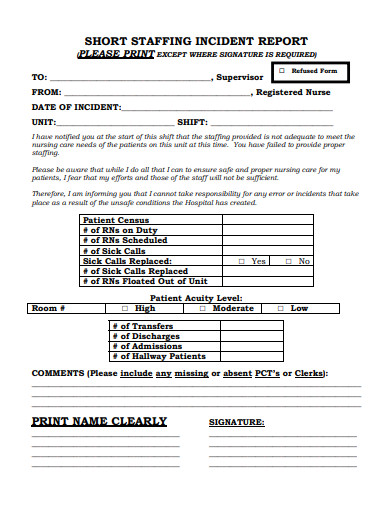
Size: 76 KB
11. Nursing Home Incident Report
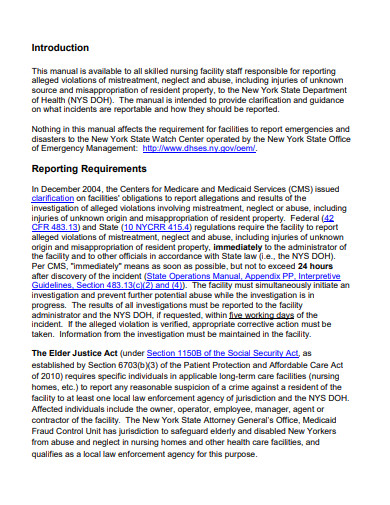
Size: 540 KB
12. Nursing Student Medication Incident Report
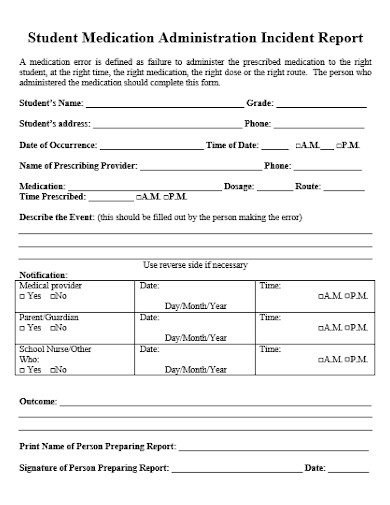
Size: 10 KB
What Is a Nursing Incident Report?
We know what an incident report is and what it looks like. But do we have any idea as to what a nursing incident report is and what it looks like? Is there even any difference between these two kinds of reports? A nursing incident report is a kind of report that is filled out by nurses or anyone in the health care or medical field. This kind of report is made solely to fill out what they believe may have caused the incident, what happened during the incident and if there are any people involved in it. Since a lot of incidents do happen with patients under health care, an incident report is then used to help figure out the problem, find a solution and be able to find a way to deal with it permanently. Reports like these are very important, apart from it being used by nurses, it is also in a way used as a document or a history report for anyone who may have encountered the same issue and to find a solution or a better solution by comparing it to previous notes.
How to Write a Nursing Incident Report?
Being able to know what can and cannot be written in a nursing incident report is important. Take note that this document is a formal written report, and must be treated as such all the time. So to not make any mistakes when writing your incident report, here are five simple tips to guide you when you are writing your nursing incident report.
1. Remembering the Details as Much as Possible
Just like any other kind of report, a nursing incident report would have the same format as that of a normal report. Remember your details as much as possible. Make sure that what happened during the incident was exactly how it happened. If you are not able to remember the exact things, make sure to give at least clues.
2. Watch Your Tone, Spelling and Grammar
It goes without saying, when you write your incident report, your tone should also be watched carefully. Make sure that when you write, you do not sound as if you are blaming the patient or the nurse, or just about anyone there. Also watch your spelling and grammar. A lot of people would be reading your report and may find it unprofessional to see a lot of spelling and grammar errors.
3. Stick To How and What Happened
Avoid fabricating your report. If it so happens that they find out you fabricated the report, chances are you will face some consequences. A report is not a story filled with nice things, it’s facts. Stick to how and what happened. All the while keeping a professional matter when writing.
4. Provide Facts on What Happened
A good way to prove that this really happened is to provide as much evidence as possible. If you are not able to get a photo to prove it, you can write what happened in chronological order. Make sure that you include the time, the person or people involved and the date. Be more specific as you can.
5. Finalize Your Report and Send It
Last but not the least, check before you finalize and send the report. Make sure when you are reading your report, it sounds professional and not accusing someone of something that happened. In addition to that, make sure that all the facts and evidence are provided in your report.
What is a nursing incident report?
A nursing incident report is a kind of report that a nurse or any health care worker writes to report an incident. This report gives a good bird’s eye view of how the incident happened and what can be done to resolve it.
Why is it so important to write about the incident in detail?
The reason it is necessary to write the incident in detail is to make sure that you have written out what really happened. Not fabricating anything in the report and to make sure that anyone who was there is also aware of what happened. That they can assure the one reading your report that it really happened.
What is something that should be avoided when writing a nursing incident report?
Forgetting to place the evidence or the proof of what happened. As well as not rearranging in chronological order as to how it happened. Details are an important part of the incident report.
The next time someone tells you to write a report, always make sure to have the necessary things for it. The evidence or the facts, the information, and most importantly the report itself. Make sure to have every single detail in check. Make sure that your story or your report does not sound like it was fragmented and of course, the tone of your writing should not make it sound like you are not taking this seriously. It is a professional report.
Text prompt
- Instructive
- Professional
Craft an incident report on a classroom equipment damage involving students during a group activity
Develop an incident report about a lost personal item of a student reported in the school library.

Nursing Incident Report | A Quick Guide

Did you know that one of the risks to patient safety is unexpected and preventable incidents? Patient safety is the number one priority of any healthcare facility. One of the ways of ensuring this is by writing a nursing incident report– a document that not only identifies issues but also provides opportunities for improvement. Incident reporting is strictly based on learning from prior experiences. For this reason, you must learn how to write a good nursing incident report. With the help of our nursing writers , creating a compelling incident report is easy. In this guide, our nursing writers will provide you with all the steps and tips needed to learn how to write an incident report.
What is the Meaning of an Incident Report?
An incident report is a type of document that systematically outlines important details about an unexpected event or accident. Nurses write an incident report to report an incident that could have or did cause harm to a patient or property damage within healthcare.
So when should an incident report be filed? An incident report is filed whenever any of the following incidents occur:
- Medication errors : Any errors that occur when prescribing or administering medication should be recorded. Medical errors could also occur because of wrong dosage, wrong medication, incorrect route of administration, and giving medication to the wrong patient.
- Malfunction of a medical device : When a medical device fails to function properly, especially when in use, it must be reported.
- Patient falls: Incidents of either patient falling either in the hospital or under the care of a nurse, at home or at a nursing home must be reported.
- Fire: If a fire occurs in the facility, then it must be reported.
- Adverse drug reactions: Unexpected reactions to a medication given to patients must be reported.
- Bedsores: Bedridden patients or those with limited mobility who develop pressure ulcers should be reported.
- When a patient leaves the hospital against medical advice: If there are instances when patients walk out of the hospital without being formally discharged or refusing to continue to receive treatment, then it should be reported.
- Near misses or close calls: In the event that an incident occurs but was prevented before affecting the safety of the patient, it should also be reported.
- Disease outbreaks: Disease outbreaks within healthcare settings should be reported.
What are the Elements of an Incident Report?
The following elements should be included in your nursing incident report:
- Date, time, and location where the incident happened. This helps establish a timeline for the events that happen.
- Name and address of the facility where the incident occurred.
- Names of the affected individuals
- Names and roles of witnesses of the incidents,
- Incident type and details, written in a chronological format
- Key details of the injury or damage.
- Total cost of the injury and damage.
- Name of physician notified.
- Suggestions for corrective action to prevent such incidents in the future.
The aim is to provide as much information as possible to ensure that readers understand exactly what happened. It will also help the management team set up appropriate measures to ensure such incidents do not occur again.
When Should an Incident Report be filed?
Incident reports are written in the hospital immediately after an incident occurs and not later than 48 hours. The rule of thumb is immediately an incident occurs. Even if it does not result in harm, the facility or organization will still have something to learn from it. If you are not sure whether to write an incident report, consult your facility's policy or, better yet, write it whenever something unusual happens.
A nurse or any other licensed professional present when the incident occurs is responsible for filing an incident report.
Importance of Incident Reporting
An incident report is an essential part of an organization's safety measures and quality improvement. As a nurse, you must write an incident report every time an abnormal incident occurs. Here are more reasons why nursing incident reporting is mainly for:
Maintain Patient Safety
The World Health Organization (WHO) defines patient safety as the absence of preventable harm to patients while receiving care at a healthcare facility. Maintaining the safety of patients is the sole responsibility of a healthcare facility, and one of the ways of ensuring this is by writing an incident report.
By documenting incidents, an organization can implement corrective measures to ensure they do not occur again in the future, thus safeguarding patient safety.
Quality Improvement
Incident reports provide valuable information that can help with quality improvement initiatives within an organization. The safety of patients can be improved when an organization engages in a cycle of quality improvement.
An analysis of the incident will reveal significant problems and areas for improvement, such as staff training, implementing evidence-based practices, increasing communication, etc. This approach ensures that an organization keeps its patients and workers safe from harm.
Track Trends
A well-written incident report helps an organization identify a pattern of problems or issues that are recurring that could jeopardize the safety of everyone within. These trends may indicate a larger problem within an organization, thus allowing the management to adopt preventive measures.
Additionally, by tracking trends, an organization can gain foresight about patient experiences and improve the quality of services.
Help with Risk Management
Incident reports are great tools in the risk management process. When an organization is able to identify problems and near misses, it can design strategies to curb liabilities and prevent serious problems.
Effective risk management strategies are based on accurate information from incident reports, thus helping minimize legal, financial, and reputation risks that could damage an organization.
Professional Accountability
Writing incident reports promotes accountability among nurses and other healthcare workers. By documenting their actions and behaviors when an incident occurs, healthcare workers can take responsibility for their actions and seek improvement.
By taking accountability, nurses and other employees can promote a culture of continuous improvement and growth.
Legal Compliance
An incident report serves as a record for liability. The report includes crucial information about an incident, how it happened, and those affected. Healthcare workers are bound by legal and regulatory requirements when writing this information to demonstrate their commitment to ensuring patient safety and accountability.
Remember that incident reports could be used by authorities and the court when investigating the cause of the incident. If it is properly written, an incident report can provide valuable evidence that will prove the nurse and the facility is not at fault for the incident.
Failure to report these incidents or misrepresent them results in serious legal issues for both the organization and its workers.
Steps for Writing a Nurse Incident Report
Follow these steps to help you write an effective nursing incident report.
Gather Information
Gather all relevant information about the incident, such as the time, date, location where the event occurred, and who was affected or witnessed the event, e.g., patients, healthcare providers, etc.
Use the following questions to help you know what information to include in your report:
- What type of injury occurred? Was it fatal or non-fatal?
- What were the employees/patients doing when the incident happened?
- Who asked the employee or the patient to do what they were doing at the time of the incident?
- Was property (s) damaged?
- Where did the incident happen?
Remember, incident reports are done as part of the process of analyzing a particular event that has led to an injury, property damage or the presence of a hazard. So, providing adequate information about an issue can help ensure that proper measures are put in place to prevent the situation from happening again in the future.
Always ensure that your incident report reflects what happened exactly. So, ensure you take time to remember everything before writing the report.
Describe What Happened
Now that you remember everything that happened, begin writing it. Provide a chronological order of the events leading up to the incident. Provide the time and date the incident occurred to establish a clear timeline of the events and uncover any trends.
Consistent and comprehensive information about the time will help investigators track, report, and analyze the events of what happened. In addition, it will help establish the duration of the incident, response time, and actions taken at the time of the incident.
If the event was a medical error, provide information on the type of medication, brand name, manufacturer, and the nature of the error that occurred.
Also, provide the location of the incident. The building, room, floor area, etc. Use visual aids, such as a picture, to ensure your information is more precise. This information is necessary to identify surrounding risks that could have caused the problem.
Use clear and objective language and ensure every piece of information is relevant to the event.
Describe the Injuries
Determine the outcome of the incident. If people were injured, write down the nature of those injuries and provide the following details:
- Type of injury
- The severity of the injury
- Injured body parts.
- Type of treatment(s) provided.
Write down Patient’s or Affected Person’s Information
Document all relevant information about the patient involved in the incident. Provide accurate information such as their names, ages, medical record number, bed number, illness, condition before and after the incident, etc.
Keep in mind that patient information must be handled with confidentiality . Follow your organization’s privacy policies and regulations when sharing such information in the incident report. Ensure that no unauthorized persons access this information.
If other people were affected, identify them with their names, job titles, shift arrangements, training, contact numbers, and any other relevant information that will help those involved make important decisions.
Related: Ethical dilemmas in nursing.
Identify the Witnesses
The people present during the incident are most helpful when providing accurate information about events. These witnesses are an important part of any incident as they help clarify what happened and provide a sequence of the events that resulted in the incident.
So, identify the wiriness in the incident by naming them, their titles and roles at the time the incident happened.
Once you identify them, record their accounts of every incident that occurred. Please note witnesses directly involved in the incident, particularly serious issues, could be experiencing emotional stress. Therefore, they could need time to calm down first before talking about what happened.
Ensure you conduct the interview as soon as it has happened. This ensures the witnesses’ recollection of the events is fresh. Having this ensures detailed and accurate information that will smoothen the investigation process.
Objectivity is key when it comes to taking witnesses into account. Ensure you record their accounts of the incident verbatim.
Write Down Contributing Factors
What contributed to the incident? Was it the weather? Equipment failure? Was it hazardous substances? Human error? Whatever it is that you think led to the incident happening, write it down clearly.
Document both immediate factors and underlying issues to ensure effective and lasting solutions to the problem. It is important to clearly state which factors happened after the incident and those that contributed to the issues. This clarity will help the management team to design effective strategies to solve the problem.
Please also note that there is never one single cause of an issue. Identify all variables that contributed to the incident, even those that you think were insignificant. Make sure to look deeply, without judgment, at everyone's actions and irresponsibility when the incident happened.
Document the Actions Taken
Were there actions taken to stop the incident from going on? Record all actions and interventions taken to help those affected by the incident in the action section. Were they given medications? Was the equipment repaired?
Provide specific tasks of everything that was done to curb the event. Write these actions in the sequence in which they were taken. As you do this, ask yourself the flowing questions:
- Why was it okay for them to make the decisions they did?
- Why did they act the way they did?
Also, mention whether the facility's management or authorities were notified. If possible, provide details of conversations, consultations, or referrals that occurred because of the incident.
Consider also including the specific actions that you can take to complete writing the incident report.
Recommendation for Future
What would you like done in the future? Document your suggestions that will help prevent similar incidents in the future based on what you have learned now. For instance, if a patient or staff fell and injures themselves because of a slippery floor, suggest covering them with mats and rugs or using scrubbers-dryers instead of wet cleaning.
Besides specific strategies, you can propose improvements in the facility's policies, procedures, and training to mitigate risks.
Review and Revise the Incident Report
Go through your incident and check whether you have included all the information. Check for accuracy, completeness, and consistency throughout the document. If possible, verify your information with your coworkers or other witnesses to ensure your document reflects the true nature of the incident.
Consider also verifying your incident report against medical records or other hospital documentation to ensure you have written it according to the facility's policy.
Do's and Don't for Writing an Incident Report in Nursing
- Write your incident report immediately after it has happened.
- Your description of what happened should be clear and concise.
- Provide a detailed timeline of the events and the actions.
- Provide the interventions that were done to help the injured person.
- If there were any witnesses present, include direct quotes of their account.
- Write with a pen, not a pencil. A pencil can be erased easily.
- Where possible, attach relevant photos of the incident, injury, etc., as they can help provide the root cause of the problem.
- Include the information about the incident report in a patient's health records.
- Procrastinate writing the report as this could lead to inaccuracy.
- Speculate or guess about what might have happened in the incident. Every information you provide should be factual.
- Use bias or judgmental language when describing the events.
- Refrain from throwing around accusations or blaming people for the actions that led to the incident. Instead, focus on identifying the main cause of the issues.
- Exaggerate or minimize the severity of the issue. Maintain honesty when reporting the facts of the incident.
- Dismiss near misses. Even when the incident did not result in loss of life or any form of harm, ensure you report it. Near misses provide valuable opportunities for people to learn and the organization to set measures to prevent future incidents.
- Forgetting to follow up. After submitting your incident report, follow up with the relevant parties to ensure appropriate actions are taken to prevent similar situations in the future. Ensure you advocate for the right changes, including policy changes.
- How to write a nursing Quality Improvement Report.
- Steps for writing a great policy analysis paper.
- How to write a nursing research paper.
- Writing a nursing interview essay.
And there you have it, a simplified guide for writing a nursing incident report the right way. Remember, when writing these types of reports, the aim is to capture every detail of the event so that someone who was not present or witnessed the events has a clear picture of what occurred.
If you are having a hard time writing an incident report, let our writers help you . Our expert writers will guide you on the dos and don’ts of writing a catchy incident report that leads to meaningful change.
Struggling with
Related Articles
Nursing Information Systems: Pros and Cons, Types, and Examples

Nursing Theorists and Theories in Nursing Practice
Best Nursing Topics and Ideas for Presentations
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.
- Journey Management
- Lone Worker Management
- Alertness and Impairment Test
- Predictive Roster Analysis
- Incident Reporting
- Hazard Identification
- Safety Observations
- Audits and Inspections
- Mining, Oil and Gas
- Manufacturing
How to Write an Incident Report - With Examples
According to research on safety management among nurses (in hospital settings), "Despite 94.8% of registered nurses being aware of incident reporting systems, only 32% reported an incident in a month, indicating a critical gap between awareness and practical reporting practices in healthcare institutions."
It can drive severe consequences for overall safety in a workspace and shows that mastering the art of incident reporting is fundamentally integral to the effectiveness of your workplace safety and risk mitigation.
In this guide, you’ll learn the keys to:
- Optimizing the incident reporting process
- Crafting a detailed incident report
- Understanding the core elements of effective reporting
- Writing a compelling and structured narrative
- Adapting examples of incident reports for clarity
- How to find incident report forms tailored to your sector
- How the newest incident reporting software can change your approach
Equip yourself with the knowledge and the tools to transform your incident reporting from tedious form completion to a smart working environment. From basic principles to safety incident management software , your incident reporting toolkit is right here.

Incident Report And Its Purpose
An incident report is a formal written document that serves as a reference when an unexpected event or accident occurs. This event could result in injury, damage to property, or work interruptions.
The main purposes of an incident report are to:
- Capture key details of what happened while events are still fresh in witnesses’ minds. It is the document of who, what, when, where, injuries/damage sustained, equipment/property affected, actions taken, and more.
- Allow a thorough investigation of the root causes and contributing factors that culminated in the incident. The more thorough your report, the more insight it provides on how and why the incident transpired.
- Identify any safety or operational policies violated that were part of the incident. It reveals if any protocols were not followed or were overlooked altogether.
- Inform subsequent action to prevent any similar incidents from occurring in the future. It will help management to see where they need to make improvements in processes, training equipment, policies, facilities, etc.
[ YOU CAN ALSO DOWNLOAD THIS FREE GUIDE TO EFFECTIVE WORKPLACE INCIDENT REPORTING ]
Core Components of an Effective Incident Report
Fundamental information.
The fundamental information outlined in an incident report includes:
- Type: Categorizing the incident provides a point of reference. Common types include injuries, property damage, security incidents, workplace violence, environmental problems, privacy breaches, and more.
- Location, date and time: The “where and when” of any incident is a must. Be as specific as you can with location, and with date and time.
- Names of individuals involved: List all people involved in the incident. Give the full name and any title or role, i.e., Robert Patterson, Security Guard. If there were injuries, list the person who was injured and list witnesses with their titles or roles, i.e. Alice Lansing, Accountant.
- Injuries sustained: Include a list of injuries, first aid that might have been administered, and any medical treatment. No injuries? State, "No injuries were sustained."
Specific Details
The specifics of an incident report provide important context:
- Equipment involved: Make a note of any tools, machinery, materials, chemicals or other equipment involved in the incident. Include the manufacturer, model number if it applies, and precise details of how the equipment was being used.
- Events leading up to the incident: The reconstruction of events can offer a number of insights into causes. Provide a concise chronological sequence of events leading up to the incident.
- Account of the incident: A detailed, chronological narrative of the incident itself will bring the incident to life. Use precise, objective language, quoting any witness statements where relevant.
- Subsequent events: Make a note of any actions that were taken after the incident, such as first aid, medical treatment, notification of the appropriate authorities, or checks for any damage or maintenance required on the equipment involved.
This leads to a basic account combined with vivid detail, making a full and useful incident report. The combination allows for the causes to be properly investigated and for the incident to be the basis for preventing similar eventualities.
Crafting an Effective Incident Report
A narrative structure is essential while writing an incident report. Organize the report into three basic sections:
Introduction
Who, what, where, and when should be answered in the introduction. As an example:
“Jane Doe, an ABC Company cashier, was involved in an incident around 10:15 am on Tuesday, March 1, 2022. The incident occurred in the company's headquarters breakroom at 123 Main St, Anytown, USA."
From here, we know that Jane Doe was involved, an event occurred, on Tuesday, March 1st, 2022, at 10:15 am, and in the breakroom at 123 Main St. It shows how this introduction sets the background for the report.
The body details the incident from beginning to end. It includes all relevant occurrences before, during, and after the incident.
As an example:
“Jane Doe walked into the breakroom and made her coffee at the coffee maker. As she reached for the coffee pot, she slipped on a puddle liquid and fell to the ground. The coffee pot struck her right calf and shattered. Jane Doe screamed out in pain with the fall.”
The body reaffirms who, what, where, and when, as well as the chronology.
The conclusion describes the resolution of the incident as well as key findings. As an example:
“Emergency services were called at 10:18 am. Jane Doe was removed by ambulance to Riverdale Hospital for a laceration of her right leg. She received 12 stitches. The broken coffee pot was cleaned and thrown away. Facilities were made aware and requested to keep a supply of Wet Floor signs positioned near breakroom spills.”
In the conclusion, the resolution and incident investigation recommendations are briefly stated to bring the matter to a close.
This introduction-body-conclusion structure makes incident reports logical and complete and makes them easy to understand. A story that winds its way to a conclusion makes a whole lot more sense.
Incident Report Example – How To Write It?
Here’s how an incident report will be written for “Main Office Security Incident - Unauthorized Entry Attempt”:
(This Incident report is vital, because it captures the security event and can be reviewed to make future security improvements.)
Other Examples Of Incident Reports [Manufacturing And Mining Industry]
Manufacturing Industry Incident Report Example:
Mining Industry Incident Report Example:
Incident Report Forms (For Different Organizations)
Reporting incident forms are the usual medium used to document incidents. They are tailored to the sector and the organization, so incident report forms differ. Here are a few examples:
General Staff Incident Report
These generic staff or personnel incident reports are employed by many businesses to log employee, customer, and visitor incidents. A general staff incident report generally includes:
- Person’s name and contact details
- Incident Time, date, and site
- Pertinent details about what happened
- Kind of injury or damage
- Name of witnesses
- Safety measures taken Suggestions for prevention
Here’s what a normal general staff incident report looks like:

Incident Report Construction Site
Construction job site safety guarantees in-depth incident reporting. Construction incident reports include particulars, for example:
- Name and role of person injured or involved
- Date, time, exact location, and description of incident
- Type of injury or illness sustained
- Equipment, materials, or chemicals involved
- Actions taken following the incident
- Suggestions to improve safety and prevent recurrences
A normally used construction site incident form looks like this:

Hospital/clinic Incident Report
Healthcare utilizes unique incident report forms to describe patient care, medical therapy, pharmaceutical errors, laboratory mishaps, confidentiality breaches, and a whole lot more. A healthcare facility or hospital might have an incident report that includes:
- Patient safety incidents, falls, infections, or privacy breaches
- Medication errors or equipment malfunctions
- Workplace injuries to staff
- Security issues, theft, property damage, or vandalism
Here’s a sample of patient incident report form usually used in clinical settings:

Incident Reporting Software For Smarter Workplace Management - SafetyIQ
SafetyIQ is an advanced incident reporting software that transforms incident reporting by providing a sleek, user-friendly platform that sets new industry standards for workplace safety.
Emerging as the leading incident reporting solution, SafetyIQ is redefining workplace safety with a variety of next-generation features and comprehensive free guides.
Take a closer look at the key features of this tool:
- Effortless Incident Reporting: The platform simplifies and centralizes the incident reporting process, allowing users to submit full-featured incident reports – complete with multimedia documentation – with minimal effort.
- Customization for Unique Needs: SafetyIQ tailors incident report forms to meet the unique requirements of each organization, expediting incident data capture and analysis in the process.
- Proactive Safety Measures: This platform is a host of specialized solutions for managing high-risk scenarios – Journey Management , Lone Worker Management , Fatigue Management , and beyond. It helps steer organizations beyond compliance and toward a proactive culture of safety.
- Real-time Insights and Analysis: Organizations enjoy a comprehensive suite of reporting dashboards that reveal the hidden safety performance insights within their data in real-time, featuring color-coded charts and infographics that allow for rapid identification of movements.
- User-Centric Design: The entire solution is designed with an emphasis on the end user, prioritizing a clean, user-friendly interface for both field workers submitting incidents and the managers analyzing the safety trends within their organization.
This software turns incident reporting into the beginning of a proactive safety culture by equipping organizations with the resources they need to put in place world-class safety practices continually. With its ability to assign corrective actions based on a data-driven approach, SafetyIQ is the best solution for workplace management and safety.
FAQs - Get More Answers Here!
Incident reporting software is a tool designed to streamline the documentation of untoward events or accidents in a business or workplace, which is crucial for reference, investigation, and informing corrective actions. It ensures a systematic approach to safety incident management.
SafetyIQ allows live incident reporting through its user-friendly platform, enabling real-time submission of multimedia-rich incident reports for immediate documentation and analysis of safety incidents.
SafetyIQ offers incident report templates that capture the critical information followed through a structured format, enabling consistency and completeness in incident documentation.
SafetyIQ has a user-centric design from the bottom up for an intuitive user experience that makes it easy for field workers to submit live incident reports and managers to analyze safety trends and overall enhance the incident reporting and management process.
Live incident reporting is simple and easy with the online platform. It enables the convenient and immediate submission of data-rich incident reports in real-time. Companies can customize the tool features to support unique requirements and enable proactive safety measures.
We cover a range of topics in our articles - view all blogs .
Get more actionable insights in your inbox!
Free guide: future proof your safety program.

Copyright © 2024 SafetyIQ Pty Ltd. All Rights Reserved.
Consent Preferences

- Incident Report in Nursing: Definition and Examples

Nursing Career Guide
Why Incident Reports Are So Important for Nurses
“To err is human, to cover up is unforgivable, and to fail to learn is inexcusable,” states Professor Liam Donaldson, World Health Organization (WHO) Envoy for Patient Safety.
Two words: Incident Reports. Ask any nurse about them and you will probably not get a happy response. Groans about the time they take, uncertainty about what to include, and worries about being punished. Maybe even a little desire to skip it.
It’s time to rethink how you feel about incident reports. Stop seeing them as a time-sucking enemy. Start seeing them as a way to a better workplace…and your protection.
What exactly are they?
The definition is simple: An incident report in nursing is a report which details an event where a person is injured, or property is damaged, threatening patient, visitor, or staff safety. Although this seems straightforward, an “event” isn’t always obvious.
There are three types to know about:
Sentinel Event: Any unanticipated event in a healthcare setting that results in death, or serious physical or psychological injury to a patient, staff member, or visitor. If the event involves a patient, it is not related to the natural course of the patient’s condition.
These are the events that are clear-cut: A fatal medication error; a nurse is attacked and beaten by a patient; an infant is abducted from the nursery.
Minor Event: An inaccurate name for this type of incident report, this is any unplanned event that results in an injury or property damage, no matter how insignificant it seems.
Examples: A patient trips on their IV pole; a nurse cuts their finger while opening a vial; a wheel on the medication cart is broken.
Near-Miss: Unplanned events where no one was injured or property was damaged, but with a different action, position, or time, they could have been.
Examples: The nurse realizes they are about administer the wrong medication; a housekeeper mops up a spill and forgets to place a caution sign; a smeared label on a specimen is difficult to read.
Why are they important?
Although incident reports can take time in your already busy shift, they serve some important purposes:
- They protect YOU. Every nurse makes mistakes . When it happens, a well-documented incident report can actually save your nursing license and career. (Read Protecting Your Nursing License: Learn Why Nurses Lose Their Licenses and What to Do About It ) If you are ever named in a lawsuit, the first question a lawyer will ask is, “Did you complete an incident report?” Keep this in mind the next time you want to complain about the hassle of filling out that form.
- They protect your organization. If a patient or their family decides to file a lawsuit against the organization (which can also include you), it will be essential for the organization to show that policies were followed, an incident report was filed, and appropriate departments or people were notified.
- They result in better patient care and an improved work environment. It might not seem like your simple incident report will have much impact, but it does. The only way changes can happen is if safety and operations managers recognize the need to make things safer for everyone.
- They create a “reporting culture” that encourages staff to participate. One of the Joint Commission’s efforts is to get accredited members to educate all employees on how to report unsafe practices and conditions. Other industries, such as aerospace, have implemented “good catch” programs to remove the fear of reprisal when reporting hazards, especially near-misses (no-harm) events.
- They make restitution easier. Suppose a visitor’s coat is stolen or someone breaks into your locker and takes your wallet. Hospitals and organizations have incidents—large and small—every day. Without an incident report, it’s impossible for administration to be fair and accurate in providing compensation for injury, loss, or damage.
What is ideally included?
Workplaces have either designated software or a specific form to complete an incident report. These make it easy to include the necessary components of the report. Your documentation will provide every detail, written in a professional and objective style.
Here is the “Baker’s Dozen” of elements in a perfect incident report:
Administrative Information
- Your name and title
- Date and time of the incident
- Exact location of the incident
Incident Information
- Details of the events leading up to the accident
- Description of the incident, in chronological order
- Description of all injuries and/or damage
Witness Information
- Current observations about the incident area
- Witness full names and contact information
- Witness statements
Actions and Recommendations
- Actions that you took to give aid
- Actions that you took to prevent further injury/damage
- Recommendations to prevent another event
Final Section
- Documentation finalization and sign-off
What else should you know?
The incident report itself is very straightforward. However, it can be challenging to provide the necessary details in an objective manner; it’s tempting to make assumptions or place blame, especially away from ourselves.
Here are some tips from legal professionals. (Read Professional Liability Insurance for Nurses: Why EVERY Nurse Must Have It )
- An incident report should be filed for ANY unexpected event. Period. Years can pass between the time of the event and when a lawsuit is filed. You will never remember all the details, so recording them in real time—and separate from the medical record—can make all the difference in the outcome.
- Remember that the patient’s medical record does NOT include mention of the incident report. The report belongs to risk management or administration. If it becomes part of the medical record, the patient’s lawyers can argue that it be turned over to them.
- Stick to the facts. Do NOT speculate about who or what might have caused the event. Simply state what happened in clear and concise terms. For example, write “Patient who usually uses a walker slipped and fell going to the bathroom. Patient was not using their walker at the time of the fall.” Do NOT write, “Patient slipped and fell going to the bathroom. They should have been using their walker.”
- Present the facts in chronological order. Make notes of exact times and what happened. Start at the time you arrive on the scene or discover the event. Example: “0920: Entered patient’s room to administer medication. 0921: Verified patient’s identity. 0922: Discovered medication was not the same dose as prescribed. Did not administer. 0924: Notified pharmacy of the discrepancy.”
- Include photos and videos. If your organization allows, taking photos, audio, and/or videos can provide valuable supplemental information. Technology makes it possible to document events in real time, with greater accuracy, allowing for proper investigation and resolution of unplanned incidents.
- Avoid judgment. Never include your opinion about how the incident occurred. Do NOT blame the physician who wrote the wrong order, the nursing assistant to didn’t raise the bedrail, or the housekeeper who left their cart in the middle of the hall. These can have serious implications for those mentioned in the document, as well as yourself.
- Use quotation marks for anything that the patient or a witness states. Quotation marks indicate details from another person’s perspective, in their exact words. Do NOT document “Patient stated they were wrong to get out of bed without help.” Instead, write, “Patient stated, ‘I was wrong to get out of bed without help.'” The difference is enormous, because it goes from subjective to objective.
- Include your own actions. Don’t forget to document the actions you took. Did you provide emergency care? Call the Rapid Response Team? Notify the family? Clean up the mess? Label defective equipment and place it out of the way? Show how you responded in a professional and thorough manner.
They are part of nursing, too
You probably didn’t learn much about incident reports in nursing school. They are a normal part of a nursing career and are not likely to go away. When filed promptly and completely, they are the best way to protect yourself from malpractice and other legal action.
When you accurately document an unplanned situation, you should have nothing to worry about. No matter how trivial the event seems, filing incident reports is part of every nurse’s job description.

About the Author
Winona Suzanne Ball
Nursing Adviser, RN | MHS, Governors State University, IL Full member of the American Nurses Association. Learn more
More help for you
How much nurses make
How to become a Registered Nurse
NCLEX terminology
NCLEX Exam Simulator
Preparing for your NCLEX RN or PN? Sure you can study the dusty textbooks, but they don’t give you a pass guarantee. We do. Pass using our fast and efficient method, or your Premium membership is free.
What’s Your Time and Sanity Worth?
Sure you can study the dusty textbooks, but they don’t give you a pass guarantee. We do. Pass your NCLEX exam using our fast and efficient method, or it’s free.

1 st Reporting
Things You Need To Know About The Incident Report In Nursing For 2024
Posted 27.01.21 by: Bond Seidel
Updated June 3, 2024.

Understanding when and why you need to approach a situation as an incident is sometimes confusing for those minor situations that may seem like they are not worth mentioning. But what exactly constitutes a situation or event where you must file an incident report in the nursing field?
A minor event may not be significant enough for you to stop what you’re doing and fill out an incident report in a busy ward. That is until it becomes a liability for you and your facility. Here’s the first thing you need to know about the incident report in nursing:
Table of Contents
1. What Is An Incident Report In Nursing?
An incident report in nursing is a report which details an event where a person is injured, or property is damaged. If these conditions occur on medical facility property, completion of an incident report is necessary.
Now that we’ve defined the first of four things you need to know about incident reports in nursing, let’s look at the others.
Some healthcare facilities have standards that are different from others, so we’ll define a baseline standard, and you can use this relative to your facility’s reporting standard. Even if the standards are different, the concept will remain the same. So, join us in examining the incident report in the nursing field and four things you need to know.
2. When To Report an Incident Report
There are going to be times when reporting an incident is a no-brainer. For example, a patient slips and fractures their arm. That’s a severe injury from a simple slip, but it happens more times than you might think. What if a patient stubs their toe on an IV cart wheel while going to the restroom?
Many situations seem trivial and not worth reporting. In some cases, nurses fear reprisals for having an incident in their ward. So, sometimes, they fear reporting any incident, albeit trivial ones, even though it is in their best interest to do so.
How do you define a severe incident worthy of reporting from a minor one? Each facility will likely have its version of these definitions. Indeed, no hospital practices medicine without a team of lawyers deciding what is or isn’t worthy of note-taking. But, in case your facility’s policies seem a little lax in the explanation department, let’s see if we can lend a hand to your dilemma.
Regarding liability, we’re not lawyers, and you should always seek legal advice. However, we know a thing or two about incident reporting. And it seems fitting that an event becomes a reportable incident when it meets one or both prerequisites:
- A person sustains an injury.
- Property sustains damage.
Want to know how your incident reporting program could send instant notifications when an injury or property damage incident report is completed? Try the 1 ST Reporting app and discover what digital reporting can do for your facility.
When A Person Is Injured – File An Incident Report
When devoid of a clear and concise plan, the simplest way is to report any injury. It could be as minor as a paper cut in this case. There is no grey area defined, so it’s simple to understand. Any injury requires a report.
With this definite ruling in practice, a medical facility has the best chance of catching and correcting potential hazards. The potential for an improved standard of care for patients becomes evident when there is no grey area in an incident reporting program.
When Property Is Damaged File An Incident Report
Similar to an incident report in nursing for injuries, you can include a polarized property damage reporting policy in your reporting practices. That is to say, incident reporting happens if damage occurs. The approach is black and white, with no grey area for misinterpretation.
With a reporting strategy of zero tolerance, nothing escapes reporting; minor damages are all reportable. It could be as simple as an IV or med cart’s wheel breaking or a broken mirror due to a patient’s outburst. No matter the cause, if the property is damaged, it should fall into the required reporting category.
3. What To Report

We’ve discussed when to report without a clear and concise reporting procedure for your medical facility. However, determining what to write is a slightly different topic. Why? We must clarify what constitutes injury or damage to a person or property. It’s this definition that may have a grey area of its own that can, in some situations, cast doubt upon whether or not to file a report.
Nurses know that sometimes you’re busy – extremely busy! There are near-miss incidents every minute in a busy ward, just stand and watch a swinging entrance door, and you’ll see multiple safety close-calls. But it doesn’t stop with doors; there are safety concerns around every corner in medical facilities.
And how should one define an injury? A minor paper cut may heal in a day or two, so does it count? If a ward is bustling and the nurses are busy, there is a likely chance that nurses may avoid an incident report for minor concerns like paper cuts or stubbed toes.
But what happens when a patient returns with a lawyer six months later and demands restitution for alleged mistreatment for some minor paper cut or toe-stubbing incident? If there is no record, you may stand little chance of defense.
The lesson to this dilemma is always to file an incident report if you are notified of an injury, no matter the severity. It’s the only way to ensure that you’ve got a record to fall back on later to protect yourself and your work facility.
Learn 12 things to include in an incident report (with five tips on writing the report better).
4. Why Nurses Need To File An Incident Report
There are five primary reasons why nurses need to complete incident reports:
Personal Liability
Facility/organization liability, enhanced patient care and facilities.
- Improved Workplace Safety Culture
Improved Restitution Process
Morally, we’re supposed to ignore personal liability and ‘just do what’s right.’ However, in a world where people throw lawsuits like we throw candy to children on Halloween, you’ve got to cover your bases.
No one wants to think they will be named in a lawsuit, but it happens daily. So, merely for personal liability, nurses should complete incident reports with every event that includes property damage (or loss) or injury to anyone.
It doesn’t look right to get fired. No one wants to lose one’s job. Worse yet is to get blackballed in your area due to a facility administration getting sued over something you neglected to report. It is not an issue of personal liability (but, in a way, it could be).
Keeping your facility out of hot water by maintaining a strict incident reporting regiment is a wise practice.
Documenting incidents of every type is the only way that safety and operations managers can implement new, evolved, or replacement procedures. From a simple material change to a procedural makeover, a facility cannot improve its functions without documentation of how an incident came to pass. And we all want a better working environment that strives to improve. In medical facilities, a minor improvement could make the difference between life and death for a patient.
Improved Workplace Safety Cultur e
In any organization, whether a medical facility like a hospital, a clinic, or another medical establishment, one thing is right. When everyone follows the rules, it’s easy to follow them yourself.
It is valid for incident reporting in the nursing community as well. No one becomes the oddball out when everyone joins the team effort to improve safety.
Hospitals are, unfortunately, places that see a lot of incidents. People from every walk of life find their way to hospitals for one reason or another. Sometimes, incidents occur, such as a person’s belongings being stolen. If someone tells a busy nurse of the infraction, but the nurse does not file a report, how will administrative staff know what restitution is deemed fitting given all the facts?
Documenting all incidents within a medical facility is critical for nurses to aid in maintaining safe and fair facilities. The goal should be for facilities where patients, visitors, and staff alike are treated with dignity and respect. That means they have the right to make claims and find reward in restitution if the situation warrants it.
The Final Thought On Incident Reporting For Nurses
The best advice is always to complete an incident report when an injury or damage occurs. A good facility management team will embrace an open reporting policy and discourage retribution to any nurse who does their duty by completing an incident report.
In any case, the only way to truly protect yourself is to complete a report and complete it factually and without judgment or bias. Completing factually and indiscriminately ensures that you genuinely cover your bases and don’t just create further headaches to deal with in the future.
Learn more about why you should complete incident reports.
Frequently Asked Questions
How do you write an incident report in nursing.

Writing an incident report in nursing is similar to writing an incident report in other industries. Following a procedure of steps when writing an incident report ensures uniformity of reporting processes and conformance with facility regulations. Learn more here about how to write a complete incident report in only 11 steps.
What are examples of an incident (in nursing)?

Incidents in nursing can range from a wide variety of events and situations. Some examples of incidents in the nursing world are: – accidental needlesticks – trips, slips, and falls – medication errors
What makes a good incident report?

A good incident report is a report that includes the vital pieces of information needed to document the incident. There are four things the writer can do to ensure the document is superior: 1. Write factually and impartially. 2. Never place judgment, blame, or make assumptions in the report. 3. Only report facts, not feelings or impressions. 4. Record data to the best of your ability quickly and efficiently while maintaining descriptive information gathering.
What is the purpose of an incident report?

The purpose of an incident report is to document any event that could affect the safety, health, or well-being of patients, staff, or visitors. These reports provide a clear and detailed account of incidents, helping healthcare facilities identify and address potential risks. Incident reports serve as valuable tools for improving patient care, enhancing safety protocols, and ensuring compliance with regulatory standards. They also protect healthcare providers by providing a factual record of events, which can be crucial in legal or administrative proceedings.
How to write an incident report for a nurse?

Writing an incident report for a nurse involves several key steps: 1. Immediate Documentation: Write the report as soon as possible after the incident to ensure accuracy. 2. Objective Description: Describe the incident objectively, including the date, time, and location. Avoid subjective language or assumptions. 3. Details of the Incident: Include a detailed account of what happened, who was involved, and any witnesses. Mention any actions taken immediately after the incident. 4. Patient Information: Provide relevant patient details, such as name and medical record number, while maintaining confidentiality. 5. Outcome and Follow-up: Document the outcome of the incident and any follow-up actions or interventions taken to address the situation. 6. Sign and Submit: Ensure the report is signed and submitted according to your facility’s protocols.
Which situations require an incident report?

In nursing, several situations necessitate an incident report, including: 1. Patient Falls: Any fall, regardless of whether it results in injury, should be reported. 2. Medication Errors: Mistakes in prescribing, dispensing, or administering medication. 3. Needlestick Injuries: Any injury involving needles or other sharp objects. 4. Patient Elopement: When a patient leaves the healthcare facility without authorization. 5. Equipment Failures: Malfunctions or failures of medical equipment that could impact patient care. 6. Violence or Abuse: Incidents involving physical or verbal abuse towards patients or staff. 7. Infections: Any incident involving the spread or potential spread of infection within the facility. These reports are crucial for maintaining a safe and effective healthcare environment, ensuring that all incidents are properly addressed and mitigated.
Now, get out there and keep making a difference in improving your safety and those around you. Good reporting and safety come to those who make it happen.
Sources and Resources
- Wikipedia Contributors. 2023. “Incident Report.” Wikipedia. Wikimedia Foundation. May 17, 2023. https://en.wikipedia.org/wiki/Incident_report .
- Besmer, Michelle, Toby Bressler, and Catherine Barrell. 2010. “Using Incident Reports as a Teaching Tool.” Nursing Management 41 (7): 16–18. https://doi.org/10.1097/01.numa.0000384141.97069.1c .
- Iedema, Rick, Arthas Flabouris, Susan Grant, and Christine Jorm. 2006. “Narrativizing Errors of Care: Critical Incident Reporting in Clinical Practice.” Social Science & Medicine 62 (1): 134–44. https://doi.org/10.1016/j.socscimed.2005.05.013 .
- P. Kantelhardt, M. Müller, A Giese, V Rohde, and S R Kantelhardt. 2009. “Implementation of a Critical Incident Reporting System in a Neurosurgical Department.” Central European Neurosurgery 72 (01): 15–21. https://doi.org/10.1055/s-0029-1243199 .
- Okuyama, Ayako, Minako Sasaki, and Katsuya Kanda. 2010. “The Relationship between Incident Reporting by Nurses and Safety Management in Hospitals.” Quality Management in Health Care 19 (2): 164–72. https://doi.org/10.1097/qmh.0b013e3181dafe88 .

Start reporting today
Join the globally-recognized brands that trust 1st Reporting to safeguard their organizations.
Join the globally-recognized brands that trust 1st Reporting to safeguard their organizations!
Privacy Overview
Customize your template.
Work with our team of experts to customize our templates to your exact business needs.
- First Name *
- Last Name *
- Phone Number *
- Changes Requested
- By submitting your information you agree to receive email marketing and promotional communications from 1st Incident Reporting
- Email This field is for validation purposes and should be left unchanged.
Free Template Download
- I would like to learn more about a digital solution to manage my reports
- Phone This field is for validation purposes and should be left unchanged.
- Incident Management How does your organization deal with registering, analyzing and managing incidents and other safety risks?
- Quality Management How do you manage improvement actions in your organization and ensure that they contribute to higher quality.
- Risk Management How dies risk management help in the identification of risks and the mitigation of incidents?
- Data Analysis How do you gain insight into the risks and improvement actions in your organization. And how do you inform your organization about the status.
- Continuous improvement culture In order to be successful in improving quality, support is very important. How do you ensure the right culture?
- Patient Safety A great deal of attention is paid to patient safety within the care sector. How do you achieve this safety.
- Collecting data
- Automate processes
- Analyze & Report
- Learn & Improve
- Software overview
- Customized solutions
- Consultancy
- Incident Management
- Complaints Manager
- OHS Incidents
- Risk Checklist
- Improve Light
- Improve 2.0
- Incident Analyses
- Satisfaction survey
- Culture survey
- Peer Support
- Aggression Report
- COVID-19 emergency response
- Blogs Many different blog posts, for every situation, for every job role.
- eBooks Are you looking for more in-depth information? View our eBooks
- Case Studies Read & learn from the experiences of other organizations.
- Product sheets View the product sheets for more information about our applications.
- Our approach
- Contact details
- Performance Health Partners US
- Cgov Australia
- Other partners
- Want to become a partner?
- Free online demo
How to write an incident report

Table of contents
The healthcare professional who witnessed an incident, or the first staff member who was notified about it, should file an incident report. But when should the report be completed and how should an incident report be written? In this article we’ll show you best practices.
When should an incident report be completed?
File an incident report whenever an unexpected event occurs. The incident report is required any time:
- A patient makes a complaint;
- A medication error occurs;
- A medical device malfunctions;
- Anyone—patient, staff member, or visitor—is injured or involved in a situation with the potential for injury
Complete the incident report as soon as possible, while the details are still fresh, but no more than 24-48 hours after the incident occurred.
What information should be included in an incident report?
Who, what, where, when, and how: Incident reports should describe factual information about what happened, answering key questions. Incident reporting needs may vary by organization, but this basic information is generally required :
- Patient name, date of birth, and hospital ID number
- Names of any other affected individuals (e.g., staff or visitors)
- Date, time, and location of the incident
- Name and address of the facility where the event occurred
- Type of incident (e.g., medication error, fall, equipment failure)
- Brief, factual description of the incident, written in chronological order
- Witness name(s) and contact information
- Details and total cost of the injury and/or damage, if any
- Action taken at the time
- Name of the physician who was notified
- Name and contact information of the person reporting the incident (if appropriate)
Best practices on how to complete an incident report
Incident reports should focus on the facts, detailing direct observations, actions taken, the assistance provided, and communications initiated:
- Describe exactly what you saw when you arrived on the scene or what you heard that led you to believe an incident had taken place. When possible, include direct quotes from the patient and/or other involved parties (e.g., a colleague or visitor) and clearly identify the source.
- Add other relevant details, such as your immediate response (e.g., calling for help and notifying the patient’s physician). Include any statement(s) a patient makes that may help to clarify his state of mind.
- Avoid making assumptions. Do not draw conclusions about how the event unfolded or speculate about who or what may have caused the incident.
- Do not assign blame. Do not point a finger at a colleague. The incident report should be a detailed description of what happened, not whom you think is responsible.
Using incident management software to simplify incident reporting
Despite the availability of incident reporting systems, many healthcare organizations still rely on manual, paper-based incident reporting, often using hand-written reports. Manual incident reporting is a time-consuming, costly, error-prone process that has many limitations, including low-quality data and limited flexibility.
Collecting incident data is just the first step in the incident management process. To identify and correct safety problems, the right people have to be able to access, sort, organize and analyze that incident data, something that is very challenging—if not impossible—when using paper reports.
To take full advantage of incident reporting, use incident management software that collects incident data electronically, stores that data in a central database, and analyzes it using proven methods.
Find out more about incident reporting and solutions
- Download our eBook " Blueprints for reporting forms " if you want to know more about developing your own reporting forms.
Our special topic page
SaaS software solutions for incident reporting:
- Incident Manager solution page
- Incident Manager product sheet
- Application overview for 5 different types of healthcare incidents
Or learn more in one of our blogs:
- Why is incident reporting important for healthcare organizations?
- The pitfalls of quality registrations on paper or spreadsheets
- The financial impact of patient safety errors
- Make healthcare safer with system-wide incident reporting

Related articles

The importance of incident reporting in nursing
Work accidents and incidents happen in every industry, including nursing. This article shows how reporting can help increase patient safety.

Bytes Without Borders: Audits, but different
Make healthcare audits easier with our application, like GGZ Drenthe did! Want to know more? Find out about it in our blog!

The SIRE Method: A Specialized Version of Root Cause Analysis
Want to know more about the SIRE (Systematic Incident Reconstruction and Evaluation) method? Read all about this analysis method in this TPSC blog.
- The Patient Safety Company
- Subscription Conditions
- Privacy Statement
Incident Report
Despite the most careful precaution of medical personnel, medico-legal accidents still occur. In all cases of accidents nurses caring for the client during the time of incident and those who saw or heard the unusual event should write an incident report. The nurse in charge of the department should also write an incident report in cases of accident. Sometimes, elderly patients in the care home sometimes show signs of neglect or abuse, which is when getting in touch with qualified nursing home abuse lawyers at places like the cain law office would be a step worth taking, especially if you care for the welfare of these patients.
An incident report is a form that filled up in order to record the details of accidents, patient injury and other unusual events that occur in a health care facility such as a hospital or nursing home. It is also called an accident report which documents the exact details of the accident or unusual event while the information is still fresh in the minds of those who witness the event. A remedy for your injuries is essential in order to get justice for the accident. An incident report will be essential to support your legal injury case.
Purpose of an Incident Report
People often regard an incident report as a black mark against the nursing staff who wrote it. This should not be the case because an informed consent is a legal document of an incident that took place. The purposes of an incident report are the following:
- To document the exact detail of an accident or unusual incident that occurred in a health-care institution.
- To be used in the future when dealing with liability issues stemming from the incident.
- To protect the nursing staff against unjust accusation.
- To protect and safeguard the client in case of negligence on the part of the nurse.
- Helps in the evaluation of nursing care to ensure safe care to all patients.
- Written at the first opportunity after the incident so that the details are not blurry or forgotten.
- Written with a pen (ink) not pencil. Information written using a pencil can be erased.
- Details should be complete and accurate. The patient should be identified with the following details:
- Hospital bed number
- Hospital ID
- Patients diagnosis
- Patient’s condition before and after the incident
Other details included are:
- Details of ward or clinical area
- Date, time and place of incident
- Details of equipments used including the serial number or asset tag identification (if appropriate)
- Written as statement of facts without interpretation or opinion. Descriptive adjectives should not be used.
For example instead of writing:
“Mr. Dimaano would not listen when I told him to stay in bed. He is very difficult to care for. It is his fault why he fell on the floor.”
You should write:
“I heard a loud crash, and immediately went to the ward. I found Mr. Dimaano on the floor.”
- Events should be written in sequence that they occurred.
- Proper technical terms should be used. For example instead of using the word bottle specify that it is a urinal.
- Identifies the witnesses.
- Identifies the medications given before the incident (if applicable)
- Identifies the equipment that is involved or used.
- Signed legibly with the correct designation.
Related Posts
Breast Biopsy
Respiratory System
Blood Chemistry

COMMENTS
According to RegisteredNursing.org, the information in an incident report should always include the who, what, when, where, and how, and — at the very least — the following pertinent information: Date, time, and facility location. Where the incident occurred. Incident type. Name of the person (s) affected by the incident.
So to not make any mistakes when writing your incident report, here are five simple tips to guide you when you are writing your nursing incident report. 1. Remembering the Details as Much as Possible. Just like any other kind of report, a nursing incident report would have the same format as that of a normal report.
Steps for Writing a Nurse Incident Report. Follow these steps to help you write an effective nursing incident report. Gather Information. Gather all relevant information about the incident, such as the time, date, location where the event occurred, and who was affected or witnessed the event, e.g., patients, healthcare providers, etc.
Location, date and time: The "where and when" of any incident is a must. Be as specific as you can with location, and with date and time. Names of individuals involved: List all people involved in the incident. Give the full name and any title or role, i.e., Robert Patterson, Security Guard.
Example of a nursing incident report. Incident Report. Date: March 12, 2024 Time: 10:30 AM Location: Willow Grove Nursing Home, Room 214 Reporter: Jane Doe, RN. Incident Details: At approximately 10:15 AM, while conducting morning rounds, I entered Room 214 to check on Mr. John Smith, a 78-year-old resident. Upon entering the room, I noticed ...
(e.g. hospital, nursing home, adult home) involved. o You will be routed to the Administrator on Duty for that program in the region where the facility is located. o The Administrator on Duty will assist with facility response to the situation. You must also file an incident report through HCS when the immediate
Present the facts in chronological order. Make notes of exact times and what happened. Start at the time you arrive on the scene or discover the event. Example: "0920: Entered patient's room to administer medication. 0921: Verified patient's identity. 0922: Discovered medication was not the same dose as prescribed.
Writing an incident report in nursing is similar to writing an incident report in other industries. Following a procedure of steps when writing an incident report ensures uniformity of reporting processes and conformance with facility regulations. Learn more here about how to write a complete incident report in only 11 steps.
Date, time, and location of the incident. Name and address of the facility where the event occurred. Type of incident (e.g., medication error, fall, equipment failure) Brief, factual description of the incident, written in chronological order. Witness name (s) and contact information. Details and total cost of the injury and/or damage, if any.
An incident report is a form that filled up in order to record the details of accidents, patient injury and other unusual events that occur in a health care facility such as a hospital or nursing home. It is also called an accident report which documents the exact details of the accident or unusual event while the information is still fresh in ...