
The Ultimate Guide to Nursing Diagnosis in 2025
What is a nursing diagnosis.
- NANDA Nursing Diagnosis
- Classification
NANDA Nursing Diagnosis List
Writing a nursing diagnosis.
- Nursing Diagnosis vs Medical Diagnosis
- American vs International

A nursing diagnosis is a part of the nursing process and is a clinical judgment that helps nurses determine the plan of care for their patients. These diagnoses drive possible interventions for the patient, family, and community. They are developed with thoughtful consideration of a patient’s physical assessment and can help measure outcomes for the nursing care plan .
In this article, we'll explore the NANDA nursing diagnosis list, examples of nursing diagnoses, and the 4 types.
Some nurses may see nursing diagnoses as outdated and arduous. However, it is an essential tool that promotes patient safety by utilizing evidence-based nursing research.
According to NANDA-I, the official definition of the nursing diagnosis is:
“Nursing diagnosis is a clinical judgment about individual, family, or community responses to actual or potential health problems/life processes. A nursing diagnosis provides the basis for selection of nursing interventions to achieve outcomes for which the nurse is accountable.”
Popular Online Master of Science in Nursing (MSN) Programs

GCU's College of Nursing and Health Care Professions has a nearly 35-year tradition of preparing students to fill evolving healthcare roles as highly qualified professionals.
Enrollment: Nationwide
- MSN - Family NP
- MSN - Adult-Gerontology Acute Care NP
- MSN - Health Informatics
- MSN - Nursing Education
- MSN - Public Health Nursing
- MSN - Health Care Quality & Patient Safety
- MSN - Nursing Leadership in Health Care Systems
- MBA & MSN - Nursing Leadership in Health Care Systems

Earn a valuable nursing credential at Purdue Global’s School of Nursing. Expand your expertise and prepare to take on leadership and independent practice opportunities. Complete your courses online, on your schedule.
Enrollment: Nationwide, but certain programs have state restrictions. Check with Purdue for details.
- Accelerated BSN-to-MSN
- MSN - Psychiatric Mental Health NP
- MSN - Nurse Educator
- MSN - Executive Leader

WGU's award-winning online programs are created to help you succeed while graduating faster and with less debt. WGU is a CCNE accredited, nonprofit university offering nursing bachelor's and master's degrees.
- BSN-to-MSN - Family NP
- BSN-to-MSN - Psychiatric Mental Health NP
- BSN-to-MSN - Nursing Education
- RN-to-MSN - Nursing Education
- RN-to-MSN - Nursing Leadership & Management
Earn your nursing degree from one of the largest nursing education providers in the U.S. Walden University’s BSN, MSN, post-master’s APRN certificate, and DNP programs are accredited by the Commission on Collegiate Nursing Education (CCNE). Get enhanced practicum support with our Practicum Pledge.
Enrollment: Nationwide, excluding CT, ND, NY and RI. Certain programs have additional state restrictions. Check with Walden for details.
- MSN - Psychiatric-Mental Health NP
- MSN - Adult-Gerontology Primary Care NP
- MSN - Pediatric NP - Primary Care
- MSN - Nursing Informatics
- MSN - Nurse Executive
- MSN & MBA - Dual Degree
Nurses Helping Nurses: Why You Can Trust Nurse.org
As the leading educational website for nurses by nurses, Nurse.org is committed to editorial integrity and data-driven analysis.
✔ Content written by 80+ licensed, practicing nurses who are experts in their respective specialties. Learn more about our nurse contributors .
✔ Transparent, trusted data sources from the U.S. Bureau of Labor and Statistics (BLS), Payscale, ZipRecruiter and Glassdoor. Learn more about our data resources .
✔ Consistent article updates to ensure they are as relevant and accurate as possible, utilizing the latest data and information when it becomes available.
What is The Purpose of a Nursing Diagnosis?
According to NANDA International , a nursing diagnosis is “a judgment based on a comprehensive nursing assessment.” The nursing diagnosis is based on the patient’s current situation and health assessment, allowing nurses and other healthcare providers to see a patient's care from a holistic perspective.
Proper nursing diagnoses can lead to greater patient safety, quality care, and increased reimbursement from private health insurance, Medicare, and Medicaid.
They are just as beneficial to nurses as they are to patients.
NANDA Nursing Diagnosis
NANDA diagnoses help strengthen a nurse’s awareness, professional role, and professional abilities.
Formed in 1982, NANDA is a professional organization that develops, researches, disseminates, and refines the nursing terminology of nursing diagnosis. Originally an acronym for the North American Nursing Diagnosis Association, NANDA was renamed to NANDA International in 2002 as a response to its broadening worldwide membership.
According to its website, NANDA International’s mission is to:
- Provide the world’s leading evidence-based nursing diagnoses for use in practice and to determine interventions and outcomes
- Contribute to patient safety through the integration of evidence-based terminology into clinical practice and clinical decision-making
- Fund research through the NANDA-I Foundation
- Be a supportive and energetic global network of nurses, who are committed to improving the quality of nursing care and improvement of patient safety through evidence-based practice
NANDA members can be found worldwide, specifically in Brazil, Colombia, Ecuador, Mexico, Peru, Portugal, Germany, Austria, Switzerland, Netherlands, Belgium, and Nigeria-Ghana.
NANDA Classification of Nursing Diagnoses
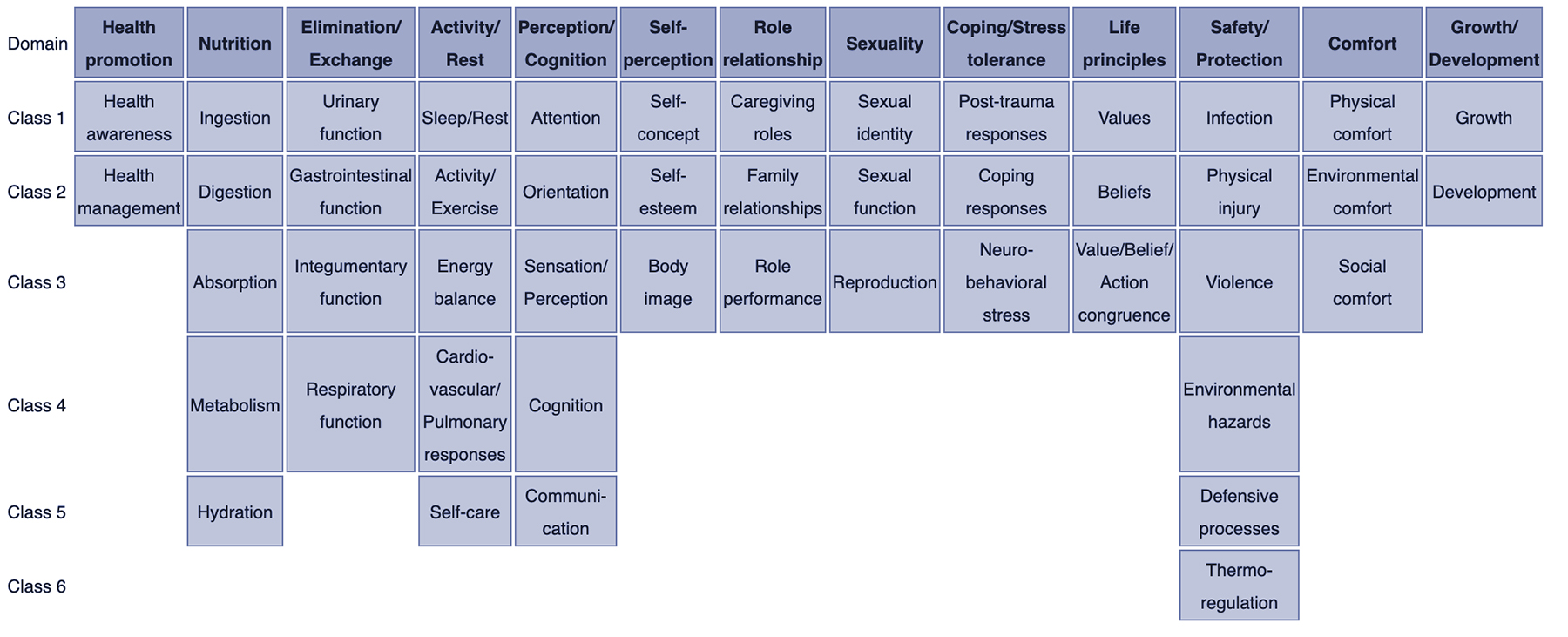
NANDA-I adopted the Taxonomy II after consideration and collaboration with the National Library of Medicine (NLM) in regards to healthcare terminology codes. Taxonomy II has three levels: domains, classes, and nursing diagnoses.
There are currently 13 domains and 47 classes:
- Health Awareness
- Health Management
- Urinary Function
- Gastrointestinal Function
- Integumentary Function
- Respiratory Function
- Activity/Exercise
- Energy Balance
- Cardiovascular-Pulmonary Responses
- Orientation
- Sensation/Perception
- Communication
- Self-concept
- Self-esteem
- Caregiving Roles
- Family Relationships
- Role Performance
- Sexual Identity
- Sexual Function
- Reproduction
- Post-trauma Responses
- Coping Response
- Neuro-Behavioral Stress
- Value/Belief Action Congruence
- Physical Injury
- Environmental Hazards
- Defensive Processes
- Thermoregulation
- Physical Comfort
- Environmental Comfort
- Social Comfort
- Development
This refined Taxonomy is based on the Functional Health Patterns assessment framework of Dr. Mary Joy Gordon. Furthermore, the NLM suggested changes because the Taxonomy I code structure included information about the location and the level of the diagnosis.
NANDA-I nursing diagnoses and Taxonomy II comply with the International Standards Organization (ISO) terminology model for a nursing diagnosis.
The terminology is also registered with Health Level Seven International (HL7), an international healthcare informatics standard that allows for nursing diagnoses to be identified in specific electronic messages among different clinical information systems.
A full list of NANDA-I-approved nursing diagnoses can be found here . Additional examples include:
- Dysfunctional ventilatory weaning response
- Impaired transferability
- Activity intolerance
- Situational low self-esteem
- Risk for disturbed maternal-fetal dyad
- Impaired emancipated decision-making
- Risk for impaired skin integrity
- Risk for metabolic imbalance syndrome
- Urge urinary incontinence
- Risk for unstable blood pressure
- Impaired verbal communication
- Acute confusion
- Disturbed body image
- Relocation stress syndrome
- Ineffective role performance
- Readiness for enhanced sleep
Examples of Nursing Diagnoses
The three main components of a nursing diagnosis are as follows.
- Problem and its definition
- Defining characteristics or risk factors
Examples of proper nursing diagnoses may include:
>> Related: What is the Nursing Process?
NANDA Nursing Diagnosis Types
There are 4 types of nursing diagnoses according to NANDA-I. They are:
- Problem-focused
- Health promotion
Popular Online RN-to-BSN Programs
Gain the skills and credentials to advance into nurse management and leadership roles, while laying the groundwork to pursue future nurse practitioner or advanced practice roles. Complete your courses online, on your schedule, at Purdue Global’s School of Nursing.
- RN-to-BSN - ExcelTrack
GCU’s RN-BSN program is tailored to meet the needs of the RN adult learner and to maximize the strengths that the working RN already possesses. Transfer up to 90 credits and earn a BSN in as little as 12 months. GCU’s online classes allow you to study at the times that work for your schedule while still enjoying a close connection with your classmates and instructor via online discussions.
The University of Texas at Arlington’s online programs are designed to help you achieve more in your nursing practice with a Bachelor of Science in Nursing. They offer convenient, flexible options for completing your RN to BSN online, designed to fit into your busy schedule.

As a pioneer in distance learning since 1985, Liberty University’s online nursing programs are designed to prepare practicing nurses to serve with integrity by teaching advanced skills from an ethical perspective. Liberty's programs are based on industry best practices and up-to-date research – so you can get the tools you need to stay on the cutting edge of nursing care and innovation.
- RN-to-BSN - Global Studies
1. Problem-focused diagnosis
A patient problem present during a nursing assessment is known as a problem-focused diagnosis. Generally, the problem is seen throughout several shifts or a patient’s entire hospitalization. However, depending on the nursing and medical care, it may be resolved during a shift.
Problem-focused diagnoses have three components.
- Nursing diagnosis
- Related factors
- Defining characteristics
Examples of this type of nursing diagnosis include:
- Decreased cardiac output
- Chronic functional constipation
- Impaired gas exchange
Problem-focused nursing diagnoses are typically based on signs and symptoms present in the patient. They are the most common nursing diagnoses and the easiest to identify.
2. Risk nursing diagnosis
A risk nursing diagnosis applies when risk factors require intervention from the nurse and healthcare team prior to a real problem developing.
- Risk for imbalanced fluid volume
- Risk for ineffective childbearing process
- Risk for impaired oral mucous membrane integrity
This type of diagnosis often requires clinical reasoning and nursing judgment.
3. Health promotion diagnosis
The goal of a health promotion nursing diagnosis is to improve the overall well-being of an individual, family, or community.
- Readiness for enhanced family processes
- Readiness for enhanced hope
- Sedentary lifestyle
4. Syndrome diagnosis
A syndrome diagnosis refers to a cluster of nursing diagnoses that occur in a pattern or can all be addressed through the same or similar nursing interventions.
Examples of this diagnosis include:
- Decreased cardiac output
- Decreased cardiac tissue perfusion
- Ineffective cerebral tissue perfusion
- Ineffective peripheral tissue perfusion
Possible nursing diagnosis
While not an official type of nursing diagnosis, possible nursing diagnosis applies to problems suspected to arise. This occurs when risk factors are present and require additional information to diagnose a potential problem.
Nursing Diagnosis Components
The three main components of a nursing diagnosis are:
- Etiology or risk factors
1. The problem statement explains the patient’s current health problem and the nursing interventions needed to care for the patient.
2. Etiology, or related factors , describes the possible reasons for the problem or the conditions in which it developed. These related factors guide the appropriate nursing interventions.
3. Finally, defining characteristics are signs and symptoms that allow for applying a specific diagnostic label. Risk factors are used in place of defining characteristics for risk nursing diagnosis. They refer to factors that increase the patient’s vulnerability to health problems.
>> Show Me Online Nursing Programs
Problem-focused and risk diagnoses are the most difficult nursing diagnoses to write because they have multiple parts. According to NANDA-I , the simplest ways to write these nursing diagnoses are as follows:
PROBLEM-FOCUSED DIAGNOSIS
Problem-Focused Diagnosis related to ______________________ (Related Factors) as evidenced by _________________________ (Defining Characteristics).
RISK DIAGNOSIS
The correct statement for a NANDA-I nursing diagnosis would be: Risk for _____________ as evidenced by __________________________ (Risk Factors).
Nursing Diagnosis vs Medical Diagnosis
While all important, nursing diagnoses are primarily handled through specific nursing interventions, while medical diagnoses are made by a physician or advanced healthcare practitioner.
The nursing diagnosis can be mental, spiritual, psychosocial, and/or physical. It focuses on the overall care of the patient while the medical diagnosis involves the medical aspect of the patient’s condition.
A medical diagnosis does not change if the condition is resolved, and it remains part of the patient’s health history forever. A nursing diagnosis, however, generally refers to a specific period of time.
Examples of medical diagnosis include:
- Congestive Heart Failure
- Diabetes Insipidus
Collaborative problems are ones that can be resolved or worked on through both nursing and medical interventions. Oftentimes, nurses will monitor the problems while the medical providers prescribe medications or obtain diagnostic tests.
History of Nursing Diagnoses
- 1973: The first conference to identify nursing knowledge and a classification system; NANDA was founded
- 1977: First Canadian Conference takes place in Toronto
- 1982: NANDA formed with members from the United States and Canada
- 1984: NANDA established a Diagnosis Review Committee
- 1987: American Nurses Association (ANA) officially recognizes NANDA to govern the development of a classification system for nursing diagnosis
- 1987: International Nursing Conference held in Alberta, Canada
- 1990: 9th NANDA conference and the official definition of the nursing diagnosis established
- 1997: Official journal renamed from “Nursing Diagnosis” to “Nursing Diagnosis: The International Journal of Nursing Terminologies and Classifications”
- 2002: NANDA changes to NANDA International (NANDA-I) and Taxonomy II released
- 2020: 244 NANDA-I approved diagnosis
American vs. International Nursing Diagnosis
There is currently no difference between American nursing diagnoses and international nursing diagnoses. Because NANDA-I is an international organization, the approved nursing diagnoses are the same.
Discrepancies may occur when the translation of a nursing diagnosis into another language alters the syntax and structure. However, since there are NANDA-I offices around the world, the non-English nursing diagnoses are essentially the same.
What is an example of a nursing diagnosis?
- A nursing diagnosis is something a nurse can make that does not require an advanced provider’s input. It is not a medical diagnosis. An example of a nursing diagnosis is: Excessive fluid volume related to congestive heart failure as evidenced by symptoms of edema.
What is the most common nursing diagnosis?
- According to NANDA, some of the most common nursing diagnoses include pain, risk of infection, constipation, and body temperature imbalance.
What is a potential nursing diagnosis?
- A potential problem is an issue that could occur with the patient’s medical diagnosis, but there are no current signs and symptoms of it. For instance, skin integrity breakdown could occur in a patient with limited mobility.
How is a nursing diagnosis written?
- Nursing diagnoses are written with a problem or potential problem related to a medical condition, as evidenced by any presenting symptoms. There are 4 types of nursing diagnoses: risk-focused, problem-focused, health promotion-focused, or syndrome-focused.
What is the clinical diagnosis?
- A clinical diagnosis is the official medical diagnosis issued by a physician or other advanced care professional.
Find Nursing Programs

Kathleen Gaines (nee Colduvell) is a nationally published writer turned Pediatric ICU nurse from Philadelphia with over 13 years of ICU experience. She has an extensive ICU background having formerly worked in the CICU and NICU at several major hospitals in the Philadelphia region. After earning her MSN in Education from Loyola University of New Orleans, she currently also teaches for several prominent Universities making sure the next generation is ready for the bedside. As a certified breastfeeding counselor and trauma certified nurse, she is always ready for the next nursing challenge.
Education: MSN Nursing Education - Loyola University New Orleans BSN - Villanova University BA- University of Mary Washington
Expertise: Pediatric Nursing, Neonatal Nursing, Nursing Education, Women’s Health, Intensive Care, Nurse Journalism, Cardiac Nursing
Nursing Diagnosis Guide: All You Need to Know to Master Diagnosing
In this ultimate tutorial and nursing diagnosis list, we’ll walk you through the concepts behind writing nursing diagnosis. Learn what a nursing diagnosis is, its history and evolution, the nursing process , the different types and classifications, and how to write nursing diagnoses correctly. Included also in this guide are tips on how you can formulate better nursing diagnoses, plus guides on how you can use them in creating your nursing care plans .
Table of Contents
- What is a Nursing Diagnosis?
Purposes of Nursing Diagnosis
Differentiating nursing diagnoses, medical diagnoses, and collaborative problems, classification of nursing diagnoses (taxonomy ii), nursing process, problem-focused nursing diagnosis, risk nursing diagnosis, health promotion diagnosis, syndrome diagnosis, possible nursing diagnosis, problem and definition.
- Etiology
Risk Factors
Defining characteristics, analyzing data, identifying health problems, risks, and strengths, formulating diagnostic statements, one-part nursing diagnosis statement, two-part nursing diagnosis statement, three-part nursing diagnosis statement, nursing diagnosis for care plans, recommended resources, references and sources, what is a nursing diagnosis.
A nursing diagnosis is a clinical judgment concerning a human response to health conditions/life processes, or a vulnerability to that response, by an individual, family, group, or community. A nursing diagnosis provides the basis for selecting nursing interventions to achieve outcomes for which the nurse has accountability. Nursing diagnoses are developed based on data obtained during the nursing assessment and enable the nurse to develop the care plan.
The purpose of the nursing diagnosis is as follows:
- For nursing students, nursing diagnoses are an effective teaching tool to help sharpen their problem-solving and critical thinking skills.
- Helps identify nursing priorities and helps direct nursing interventions based on identified priorities.
- Helps the formulation of expected outcomes for quality assurance requirements of third-party payers.
- Nursing diagnoses help identify how a client or group responds to actual or potential health and life processes and knowing their available resources of strengths that can be drawn upon to prevent or resolve problems.
- Provides a common language and forms a basis for communication and understanding between nursing professionals and the healthcare team.
- Provides a basis of evaluation to determine if nursing care was beneficial to the client and cost-effective.
The term nursing diagnosis is associated with different concepts. It may refer to the distinct second step in the nursing process , diagnosis (“D” in “ ADPIE “). Also, nursing diagnosis applies to the label when nurses assign meaning to collected data appropriately labeled a nursing diagnosis. For example, during the assessment , the nurse may recognize that the client feels anxious , fearful, and finds it difficult to sleep . Those problems are labeled with nursing diagnoses: respectively, Anxiety , Fear , and Disturbed Sleep Pattern. In this context, a nursing diagnosis is based upon the patient’s response to the medical condition. It is called a ‘nursing diagnosis’ because these are matters that hold a distinct and precise action associated with what nurses have the autonomy to take action about with a specific disease or condition. This includes anything that is a physical, mental, and spiritual type of response. Hence, a nursing diagnosis is focused on care.
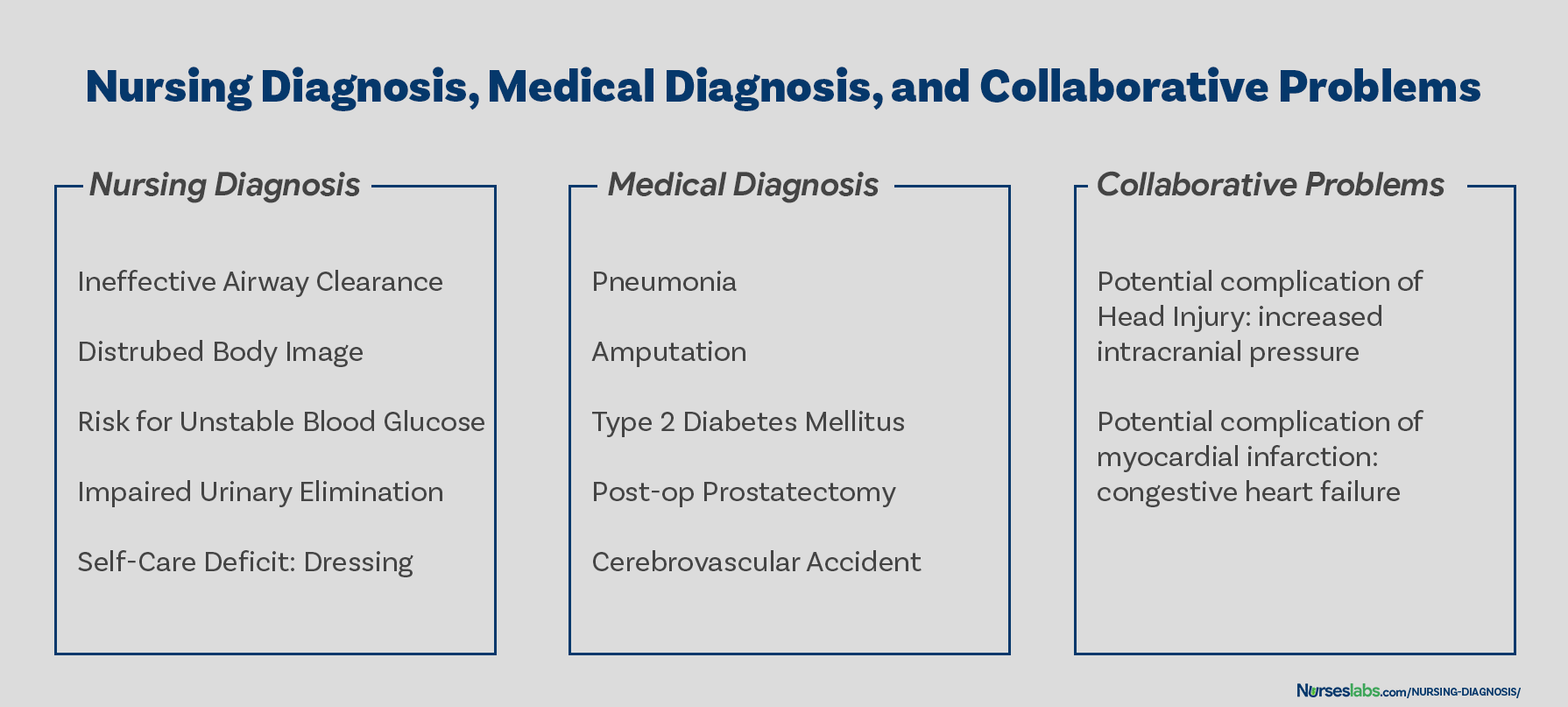
On the other hand, a medical diagnosis is made by the physician or advanced health care practitioner that deals more with the disease, medical condition, or pathological state only a practitioner can treat. Moreover, through experience and know-how, the specific and precise clinical entity that might be the possible cause of the illness will then be undertaken by the doctor, therefore, providing the proper medication that would cure the illness. Examples of medical diagnoses are Diabetes Mellitus , Tuberculosis , Amputation, Hepatitis , and Chronic Kidney Disease. The medical diagnosis normally does not change. Nurses must follow the physician’s orders and carry out prescribed treatments and therapies.
Collaborative problems are potential problems that nurses manage using both independent and physician-prescribed interventions. These are problems or conditions that require both medical and nursing interventions , with the nursing aspect focused on monitoring the client’s condition and preventing the development of the potential complication.
As explained above, now it is easier to distinguish a nursing diagnosis from a medical diagnosis. Nursing diagnosis is directed towards the patient and their physiological and psychological response. On the other hand, a medical diagnosis is particular to the disease or medical condition. Its center is on the illness.
How are nursing diagnoses listed, arranged, or classified? In 2002, Taxonomy II was adopted, which was based on the Functional Health Patterns assessment framework of Dr. Mary Joy Gordon. Taxonomy II has three levels: Domains (13), Classes (47), and nursing diagnoses. Nursing diagnoses are no longer grouped by Gordon’s patterns but coded according to seven axes: diagnostic concept, time, unit of care, age, health status, descriptor, and topology. In addition, diagnoses are now listed alphabetically by their concept, not by the first word.
- Class 1. Health Awareness
- Class 2. Health Management
- Class 1. Ingestion
- Class 2. Digestion
- Class 3. Absorption
- Class 4. Metabolism
- Class 5. Hydration
- Class 1. Urinary function
- Class 2. Gastrointestinal function
- Class 3. Integumentary function
- Class 4. Respiratory function
- Class 1. Sleep/Rest
- Class 2. Activity/Exercise
- Class 3. Energy balance
- Class 4. Cardiovascular/Pulmonary responses
- Class 5. Self-care
- Class 1. Attention
- Class 2. Orientation
- Class 3. Sensation/Perception
- Class 4. Cognition
- Class 5. Communication
- Class 1. Self-concept
- Class 2. Self-esteem
- Class 3. Body image
- Class 1. Caregiving roles
- Class 2. Family relationships
- Class 3. Role performance
- Class 1. Sexual identity
- Class 2. Sexual function
- Class 3. Reproduction
- Class 1. Post-trauma responses
- Class 2. Coping responses
- Class 3. Neurobehavioral stress
- Class 1. Values
- Class 2. Beliefs
- Class 3. Value/Belief/Action congruence
- Class 1. Infection
- Class 2. Physical injury
- Class 3. Violence
- Class 4. Environmental hazards
- Class 5. Defensive processes
- Class 6. Thermoregulation
- Class 1. Physical comfort
- Class 2. Environmental comfort
- Class 3. Social comfort
- Class 1. Growth
- Class 2. Development
The five stages of the nursing process are assessment, diagnosing, planning , implementation , and evaluation . All steps in the nursing process require critical thinking by the nurse. Apart from understanding nursing diagnoses and their definitions, the nurse promotes awareness of defining characteristics and behaviors of the diagnoses, related factors to the selected nursing diagnoses, and the interventions suited for treating the diagnoses.
The steps, importance, purposes, and characteristics of the nursing process are discussed more in detail here: “ The Nursing Process: A Comprehensive Guide “
Types of Nursing Diagnoses
The four types of nursing diagnosis are Actual (Problem-Focused), Risk, Health Promotion , and Syndrome. Here are the four categories of nursing diagnoses:
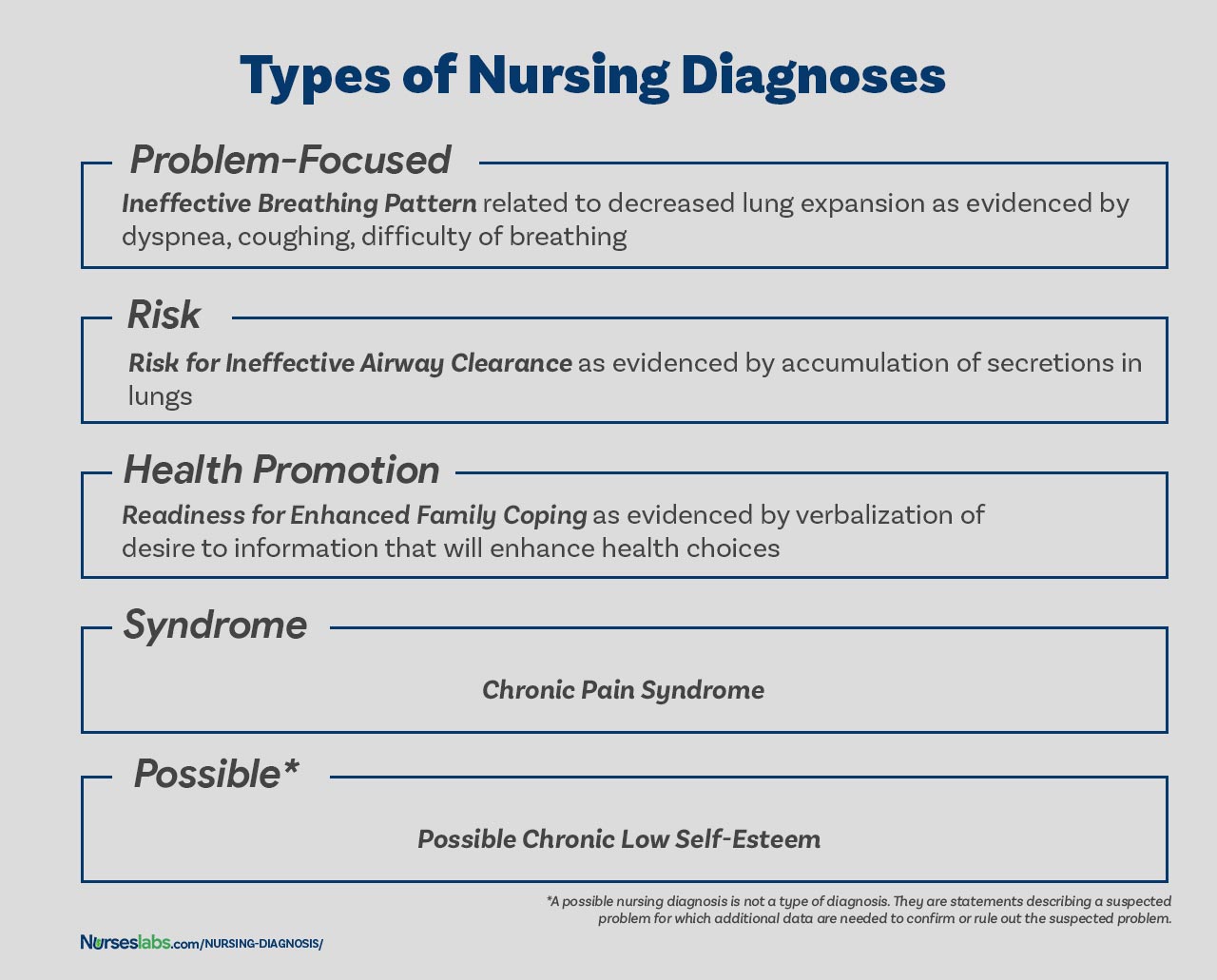
A problem-focused diagnosis (also known as actual diagnosis ) is a client problem present at the time of the nursing assessment . These diagnoses are based on the presence of associated signs and symptoms. Actual nursing diagnosis should not be viewed as more important than risk diagnoses. There are many instances where a risk diagnosis can be the diagnosis with the highest priority for a patient.
Problem-focused nursing diagnoses have three components: (1) nursing diagnosis, (2) related factors, and (3) defining characteristics. Examples of actual nursing diagnoses are:
- Anxiety related to stress as evidenced by increased tension, apprehension, and expression of concern regarding upcoming surgery
- Acute pain related to decreased myocardial flow as evidenced by grimacing, expression of pain , guarding behavior.
The second type of nursing diagnosis is called risk nursing diagnosis. These are clinical judgment for a problem does not exist, but the presence of risk factors indicates that a problem is likely to develop unless nurses intervene. A risk diagnosis is based on the patient’s current health status, past health history , and other risk factors that may increase the patient’s likelihood of experiencing a health problem. These are integral part of nursing care because they help to identify potential problems early on and allows the nurse to take steps to prevent or mitigate the risk.
There are no etiological factors (related factors) for risk diagnoses. The individual (or group) is more susceptible to developing the problem than others in the same or a similar situation because of risk factors. For example, an elderly client with diabetes and vertigo who has difficulty walking refuses to ask for assistance during ambulation may be appropriately diagnosed with risk for injury or risk for falls.
IMPORTANT: For risk nursing diagnosis, “ as evidenced by ” is used to connect the risk diagnosis label with the risk factors, rather than with the defining characteristics. The components of a risk nursing diagnosis therefore include:
- Risk diagnostic label, joined by “as evidenced by”
- Risk factors
Examples of risk nursing diagnosis are:
- Risk for Injury as evidenced by reduced cognitive awareness and use of sedative medications.
- Risk for Infection as evidenced by surgical wound, compromised immune system, and prolonged hospitalization.
- Risk for Falls as evidenced by muscle weakness , history of previous falls, impaired mobility , and use of assistive devices.
Health promotion diagnosis (also known as wellness diagnosis ) is a clinical judgment about motivation and desire to increase well-being. It is a statement that identifies the patient’s readiness for engaging in activities that promote health and well-being. For example, if a first-time mother shows interest on how to properly breastfeed her baby, a nurse make make a health promotion diagnosis of “Readiness for Enhanced Breastfeeding .” This nursing diagnosis will be then used to guide nursing interventions aimed at supporting the patient in learning about proper breastfeeding.
Additionally, health promotion diagnosis is concerned with the individual, family, or community transition from a specific level of wellness to a higher level of wellness. Components of a health promotion diagnosis generally include only the diagnostic label or a one-part statement but can be enhanced for clarity by adding related factors. Examples of health promotion diagnosis:
- Readiness for Enhanced Knowledge as evidenced by expressed desire to learn about a specific topic, openness to education, and motivation to understand complex concepts.
- Readiness for Enhanced Breastfeeding as evidenced by desire to increase breastfeeding frequency, expressed interest in learning proper latching techniques, and verbalized commitment to breastfeeding.
- Readiness for Enhanced Comfort as evidenced by expressed desire to explore comfort measures, willingness to engage in relaxation practices, and interest in improving pain management strategies.
A syndrome diagnosis is a clinical judgment concerning a cluster of problem or risk nursing diagnoses that are predicted to present because of a certain situation or event. They, too, are written as a one-part statement requiring only the diagnostic label. Examples of a syndrome nursing diagnosis are:
- Chronic Pain Syndrome
- Frail Elderly Syndrome
A possible nursing diagnosis is not a type of diagnosis as are actual, risk, health promotion , and syndrome. Possible nursing diagnoses are statements describing a suspected problem for which additional data are needed to confirm or rule out the suspected problem. It provides the nurse with the ability to communicate with other nurses that a diagnosis may be present but additional data collection is indicated to rule out or confirm the diagnosis. Examples include:
- Possible chronic low self-esteem
- Possible social isolation
Components of a Nursing Diagnosis
A nursing diagnosis has typically three components: (1) the problem and its definition, (2) the etiology, and (3) the defining characteristics or risk factors (for risk diagnosis).
The problem statement , or the diagnostic label , describes the client’s health problem or response to which nursing therapy is given concisely. A diagnostic label usually has two parts: qualifier and focus of the diagnosis. Qualifiers (also called modifiers ) are words that have been added to some diagnostic labels to give additional meaning, limit, or specify the diagnostic statement. Exempted in this rule are one-word nursing diagnoses (e.g., Anxiety, Constipation , Diarrhea , Nausea , etc.) where their qualifier and focus are inherent in the one term.
The etiology , or related factors , component of a nursing diagnosis label identifies one or more probable causes of the health problem, are the conditions involved in the development of the problem, gives direction to the required nursing therapy, and enables the nurse to individualize the client’s care. Nursing interventions should be aimed at etiological factors in order to remove the underlying cause of the nursing diagnosis. Etiology is linked with the problem statement with the phrase “ related to ” for example:
- Activity intolerance related to generalized weakness .
- Decreased cardiac output related to abnormality in blood profile
Risk factors are used instead of etiological factors for risk nursing diagnosis. Risk factors are forces that put an individual (or group) at an increased vulnerability to an unhealthy condition. Risk factors are written following the phrase “as evidenced by” in the diagnostic statement.
- Risk for falls as evidenced by old age and use of walker.
- Risk for infection as evidenced by break in skin integrity .
Defining characteristics are the clusters of signs and symptoms that indicate the presence of a particular diagnostic label. In actual nursing diagnosis, the defining characteristics are the identified signs and symptoms of the client. For risk nursing diagnosis, no signs and symptoms are present therefore the factors that cause the client to be more susceptible to the problem form the etiology of a risk nursing diagnosis. Defining characteristics are written following the phrase “as evidenced by” or “as manifested by” in the diagnostic statement.
Diagnostic Process: How to Diagnose
There are three phases during the diagnostic process: (1) data analysis, (2) identification of the client’s health problems, health risks, and strengths, and (3) formulation of diagnostic statements.
Analysis of data involves comparing patient data against standards, clustering the cues, and identifying gaps and inconsistencies.
In this decision-making step, after data analysis, the nurse and the client identify problems that support tentative actual, risk, and possible diagnoses. It involves determining whether a problem is a nursing diagnosis, medical diagnosis, or a collaborative problem. Also, at this stage, the nurse and the client identify the client’s strengths, resources, and abilities to cope.
Formulation of diagnostic statements is the last step of the diagnostic process wherein the nurse creates diagnostic statements. The process is detailed below.
How to Write a Nursing Diagnosis?
In writing nursing diagnostic statements, describe an individual’s health status and the factors that have contributed to the status. You do not need to include all types of diagnostic indicators. Writing diagnostic statements vary per type of nursing diagnosis (see below).
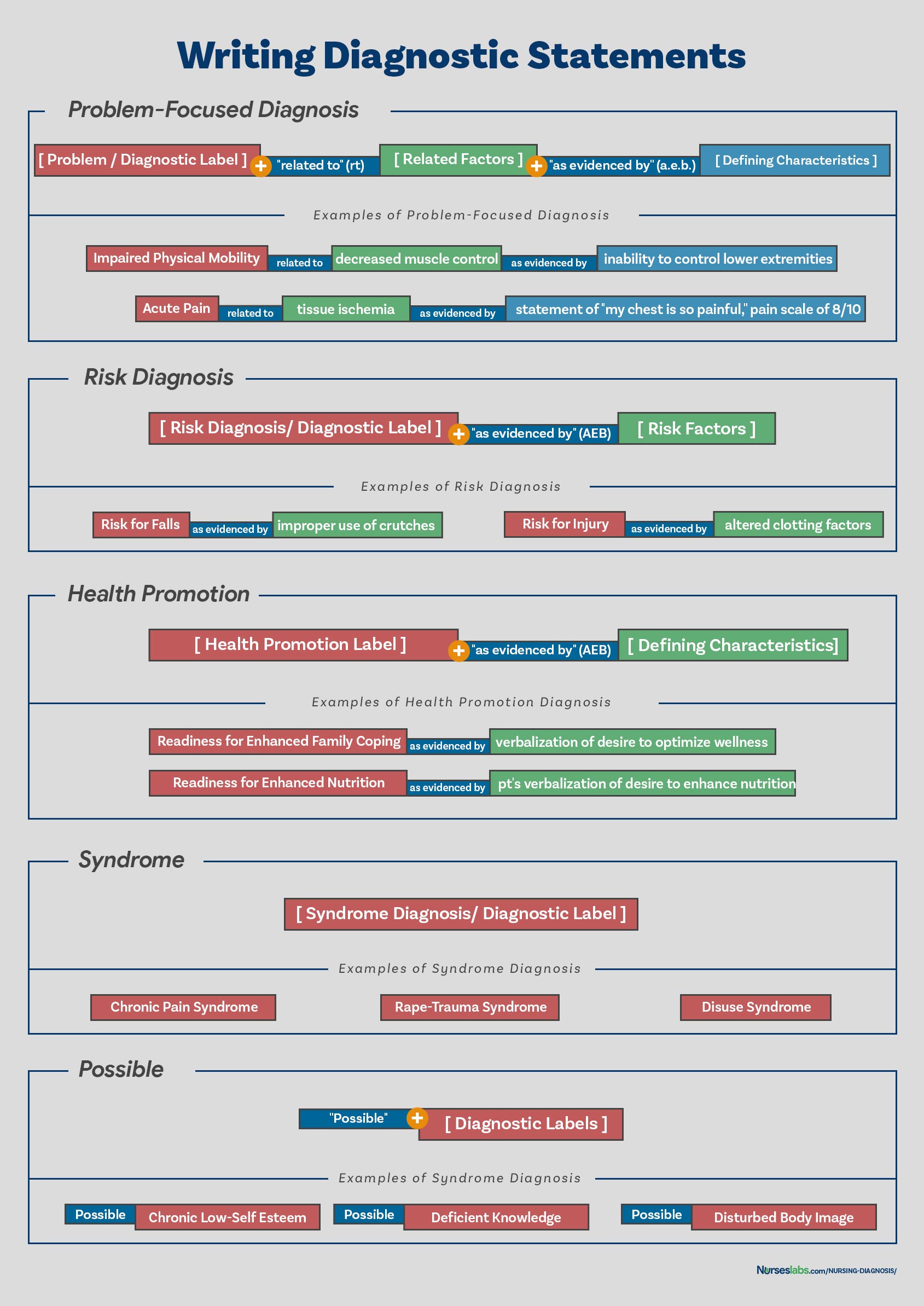
Another way of writing nursing diagnostic statements is by using the PES format, which stands for Problem (diagnostic label), Etiology (related factors), and Signs/Symptoms (defining characteristics). Diagnostic statements can be one-part, two-part, or three-part using the PES format.
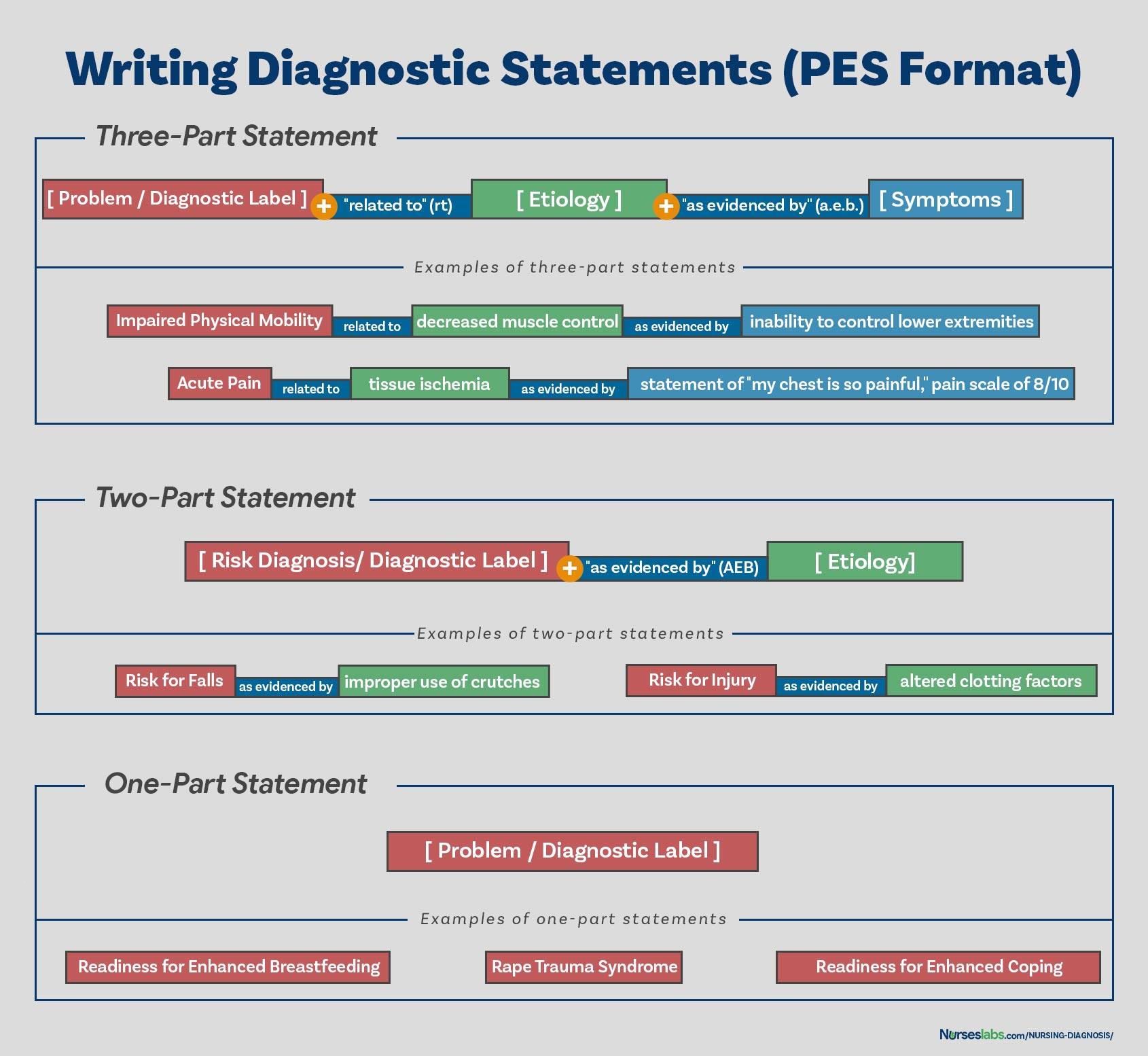
Health promotion nursing diagnoses are usually written as one-part statements because related factors are always the same: motivated to achieve a higher level of wellness through related factors may be used to improve the chosen diagnosis. Syndrome diagnoses also have no related factors. Examples of one-part nursing diagnosis statements include:
- Readiness for enhanced coping
- Rape Trauma Syndrome
Risk and possible nursing diagnoses have two-part statements: the first part is the diagnostic label and the second is the validation for a risk nursing diagnosis or the presence of risk factors. It’s not possible to have a third part for risk or possible diagnoses because signs and symptoms do not exist. Examples of two-part nursing diagnosis statements include:
- Risk for Infection as evidenced by weakened immune system response
- Risk for Injury as evidenced by unstable hemodynamic profile
An actual or problem-focus nursing diagnosis has three-part statements: diagnostic label, contributing factor (“related to”), and signs and symptoms (“as evidenced by” or “as manifested by”). The three-part nursing diagnosis statement is also called the PES format which includes the Problem, Etiology, and Signs and Symptoms. Example of three-part nursing diagnosis statements include:
- Acute Pain related to tissue ischemia as evidenced by statement of “I’m experiencing intense, sharp pain in my chest!”
- Impaired Physical Mobility related to muscle weakness as evidenced by difficulty in moving independently, and client stating “I feel too weak to move on my own.”
- Activity Intolerance related to decreased cardiac output as evidenced by shortness of breath and patient stating, “I feel exhausted after just a few steps,” secondary to pneumonia .
Variations on Basic Statement Formats
Variations in writing nursing diagnosis statement formats include the following:
- Using “ secondary to ” to divide the etiology into two parts to make the diagnostic statement more descriptive and useful. Following the “secondary to” is often a pathophysiologic or disease process or a medical diagnosis. For example, Risk for Decreased Cardiac Output as evidenced by reduced preload secondary to myocardial infarction .
- Using “ complex factors ” when there are too many etiologic factors or when they are too complex to state in a brief phrase. For example, Chronic Low Self-Esteem related to complex factors.
- Using “ unknown etiology ” when the defining characteristics are present but the nurse does not know the cause or contributing factors. For example, Ineffective Coping related to unknown etiology.
- Specifying a second part of the general response or diagnostic label to make it more precise. For example, Impaired Skin Integrity (Right Anterior Chest) related to disruption of skin surface secondary to burn injury .
This section is the list or database of the common nursing diagnosis examples that you can use to develop your nursing care plans .
See also: Nursing Care Plans (NCP): Ultimate Guide and List
- Activity Intolerance and Generalized Weakness
- Acute Confusion (Delirium) and Altered Mental Status
- Anxiety & Fear
- Bowel Incontinence (Fecal Incontinence)
- Caregiver Role Strain & Family Caregiver Support Systems
- Chronic Confusion (Dementia)
- Chronic Pain (Pain Management)
- Constipation
- Decreased Cardiac Output & Cardiac Support
- Disturbed Body Image & Self-Esteem
- Fatigue & Lethargy
- Fever (Pyrexia)
- Fluid Volume Deficit (Dehydration & Hypovolemia)
- Fluid Volume Excess (Hypervolemia)
- Grieving & Loss
- Hyperthermia & Heat-Related Illnesses
- Hypothermia & Cold Injuries
- Imbalanced Nutrition
- Impaired Gas Exchange
- Impaired Swallowing (Dysphagia)
- Impaired Thought Processes & Cognitive Impairment
- Impaired Tissue Perfusion & Ischemia
- Impaired Tissue/Skin Integrity (Wound Care)
- Ineffective Airway Clearance & Coughing
- Ineffective Breathing Pattern (Dyspnea)
- Insomnia & Sleep Deprivation
- Knowledge Deficit & Patient Education
- Nausea & Vomiting
- Physical Mobility & Immobility
- Risk for Aspiration (Aspiration Pneumonia)
- Risk for Bleeding (Hemophilia)
- Risk for Falls (Fall Risk & Prevention)
- Risk for Infection and Infection Control
- Risk for Injury & Patient Safety
- Self-Care Deficit & Activities of Daily Living (ADLs)
- Unstable Blood Glucose Levels (Hyperglycemia & Hypoglycemia)
- Urinary Elimination (Urinary Incontinence & Urinary Retention)
- For the full list, please visit: Nursing Care Plans (NCP): Ultimate Guide and List
Recommended nursing diagnosis and nursing care plan books and resources.
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy .
Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care We love this book because of its evidence-based approach to nursing interventions. This care plan handbook uses an easy, three-step system to guide you through client assessment, nursing diagnosis, and care planning. Includes step-by-step instructions showing how to implement care and evaluate outcomes, and help you build skills in diagnostic reasoning and critical thinking.

Nursing Care Plans – Nursing Diagnosis & Intervention (10th Edition) Includes over two hundred care plans that reflect the most recent evidence-based guidelines. New to this edition are ICNP diagnoses, care plans on LGBTQ health issues, and on electrolytes and acid-base balance.

Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales Quick-reference tool includes all you need to identify the correct diagnoses for efficient patient care planning. The sixteenth edition includes the most recent nursing diagnoses and interventions and an alphabetized listing of nursing diagnoses covering more than 400 disorders.

Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care Identify interventions to plan, individualize, and document care for more than 800 diseases and disorders. Only in the Nursing Diagnosis Manual will you find for each diagnosis subjectively and objectively – sample clinical applications, prioritized action/interventions with rationales – a documentation section, and much more!

All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health Includes over 100 care plans for medical-surgical, maternity/OB, pediatrics, and psychiatric and mental health. Interprofessional “patient problems” focus familiarizes you with how to speak to patients.

Other recommended site resources for this nursing care plan:
- Nursing Care Plans (NCP): Ultimate Guide and Database MUST READ! Over 150+ nursing care plans for different diseases and conditions. Includes our easy-to-follow guide on how to create nursing care plans from scratch.
- Nursing Diagnosis Guide and List: All You Need to Know to Master Diagnosing Our comprehensive guide on how to create and write diagnostic labels. Includes detailed nursing care plan guides for common nursing diagnostic labels.
References for this Nursing Diagnosis guide and recommended resources to further your reading.
- Berman, A., Snyder, S., & Frandsen, G. (2016). Kozier & Erb’s Fundamentals of Nursing: Concepts, process and practice . Boston, MA: Pearson.
- Edel, M. (1982). The nature of nursing diagnosis. In J. Carlson, C. Craft, & A. McGuire (Eds.), Nursing diagnosis (pp. 3-17). Philadelphia: Saunders.
- Fry, V. (1953). The Creative approach to nursing. AJN, 53(3), 301-302.
- Gordon, M. (1982). Nursing diagnosis: Process and application. New York: McGraw-Hill.
- Gordon, M. (2014). Manual of nursing diagnosis . Jones & Bartlett Publishers.
- Gebbie, K., & Lavin, M. (1975.) Classification of nursing diagnoses: Proceedings of the First National Conference. St. Louis, MO: Mosby.
- McManus, R. L. (1951). Assumption of functions in nursing. In Teachers College, Columbia University, Regional planning for nurses and nursing education . New York: Columbia University Press.
- Powers, P. (2002). A discourse analysis of nursing diagnosis . Qualitative health research , 12 (7), 945-965.
91 thoughts on “Nursing Diagnosis Guide: All You Need to Know to Master Diagnosing”
Very useful document indeed.
Thank you Sima! Hope it helps come up with great nursing care plans!
Thank you for this resource material. This is very simple, concise and easy to understand. This would be of great help both for the students and the teacher.
Please make proper table for nursing diagnosis it’ll be easy to read and understand .
This is simple and easy to understand.
Happy to know! Hope you visit our guide on nursing care plans too! Thanks for dropping by Modupe!
I need a complete pdf file
Hi! If you want to save it as a PDF file, simply “Print” this page and “Save as PDF”.
So very happy to stumble upon nurseslabs. Thanks so much
Happy to have helped you. Please do check out our nursing care plans list too! Thanks for visiting, Hussaina!
I want to acknowledge the writer of Understand, Matt Vera for using the initiative in simplifying the nursing notes into simple English that we as upcoming nursing students can understand nursing notes in order to practice them in our clinical. I’ve learned so much from this website and I want to be part of the nurses website so I can gather some more informations. Get me on my email. Thanks so much..
Thank you Lawrencia. Glad to be of help!
VERY NICE EXPLANATION .THANK YOU . DEAR MADAM /SIR PLEASE CAN YOU PROVIDE ME LIST OF NURSING DIAGNOSIS ALONG WITH REVISED ONE TILL DATE . I am Lecturer in college of nursing ,India Thank You
this is so educative thank you
Thank you! Glad you liked it.
really simple and effective, thank you so much.
This is great! Simple and easy to understand for the nursing students.
Comment:nice work, great nurses.
I am a nurse more than 30 yeras and try to teach my team how to used nursing process but it not success. You make me feel it simple and easy to understand . I will use your concept for my team. Thank you somuch
THANK, THANK YOU, THANK YOU FOR THE RESOURCEFUL INFORMATION.
please i want care plan on risk for unstable blood pressure i am a nursing student
@joseph auarshie jnr, can you please send me your care plan if you made it already ? I am a nursing student too. Thank you appreciated
Thanks, I look forward to learning more from you and maybe joining you in writing once am done with school. It’s awesome.
You’re very much welcome! Please feel free to ask further questions. Thank you and goodluck!
I what to check out nursing care plan
Comment: good explanation of health issue pattern
This is great. Thanks for given your time to this. Is so educative. Up thumb
Thanks alot am so interested on this
Great Work!
Thank you for the resourceful information which I was thought in school but almost forgotten until now, brain refresh, thanks
Excellent job done congratulations to all the team worker .
Please is the component of nursing diagnosis the same as type of nursing diagnosis
Each time I research about nursing diagnoses, there is something new to learn. This is a very well written piece giving great insights about nursing. More than ever, I have a better understanding of the unique body of nursing knowledge. Bravo to the Matt and entire Nurseslabs team
Thank you! Be sure to visit also our nursing care plans here .
Sorry madam the risk factors thus the potential problem has the related factors not the sign and symptom because that something has not happed yet so there is no sign and symptoms. Thank you
Excellent work and expertise team work
Usefull information
Nice work Sir/Madam thank you for giving us more hints on Nursing Diagnoses. Excellent team work.
Thank you so much for this nursing diagnosis.
Formulations of the DX has been hectic but thanks to matt vera has been of great help especally answering medsurge quizes just try to expand more on the second part (related to)of actual diagnosis
Hi Mary, Thanks you so much for your comment and endorsement. We welcome your students, thanks again!
Very useful indeed. thank you
I’m practicing nursing diagnosis by using the practice case studies my professor provided but I’m not sure if I’m doing it correctly. Here’s what I’m thinking: Problem:Anxiety Etiology: morning bouts of fear Signs and symptoms: patient stated waking nervous, light headed, agitated, and having a pounding heart Anxiety related to morning bouts of fear as evidenced by patient’s reports of waking light headed, agitated, and having a pounding heart.
In this case study we know to patient has been experiencing anxiety since childhood and was verbally abused by his father. His anxiety is causing difficulties for him to make decisions and he fears he’ll experience misfortunes whenever going to school. We also know about these bouts he has ever morning, which I thought would be a good primary diagnosis because they almost seem like a panic attack which would be extreme anxiety which is a big deal right? Am I thinking about this the right way or not and if not, what should I be concerned about as most important and how should my diagnosis be worded?
The nursing diagnostic statement you made sounds right. For the “as evidenced by” part, I would add the statement of the patient in verbatim since this is a subjective data (place it also under quotation marks) and if possible, do your own assessment and objectively obtain the data.
I would write it this way:
Anxiety related to morning bouts of fear as evidenced by increased in heart rate, apprehensiveness, and patient stating “waking lightheaded, agitated, and having a pounding heart”
well precised and nice to read.
Thanks so much for this readings, am so interested with this website I hope i could use this for my whole time
Hello Professor Matt Vera
I am Mai Ba Hai, from Hue University of Medicine and Pharmacy,faculty of nursing.I found that this content is very useful and helpful to me. I think that this content is really fit to my teaching, so I would like to ask your permission that I can translate this content into my languages (Vietnamese) to teach for my nursing students in Vietnam. I will cite you as author of this document. If you are willing to help in this point I really appreciate about it. I am looking forward to receiving your agreement. Yours sincerely.
This is so fantastic!! Thank you for taking out time to create this wonderful piece
You guys are wonderful. Thanks so much.
Very nice and very interested More ink to your pen I pray
Very useful, thank you so much
Thanks so much for the good job. Nurse Timothy Idachaba (RN, RNE, .MSC in view) from Nigeria
Matt Vera, BSN, R.N, First, I want to thank you for your amazing, short and precise note you provided for us. But I think I’ve got some trouble understanding about 3 components of Nursing diagnosis. This is because there is some variation between defining characteristics among your examples of actual and potential nursing diagnosis. Actual nursing diagnosis -Ineffective breathing pattern related to decreased lung expansion AS EVIDENCED BY dyspnoea, coughing, and difficulty of breathing. Risk diagnosis -Risk for ineffective airway clearance AS EVIDENCED BY accumulation_of_secreations_in_the_Lung. -Risk for fall AS EVIDENCED BY Muscle_weakness ……………………………………………………. As I know before, risk Nursing diagnosis misses Defining characteristics. because, the problem is not happened. but it is to happen.
So, when I compare defining characteristics among actual and risk diagnosis, there is disagreement. Accumulation of secretion in the lung is aetiology for ineffective airway clearance. But you provided it as defining characteristics. So, please make it clear.
The phrase “as evidenced by” is just used to connect the risk diagnosis label with the risk factors, rather than with the defining characteristics (as with problem-focused diagnoses).
Well elaborated, i like using nurseslabs, i always understand easily
Educative I appreciate
Such a beautiful explanation. Thank you
Very comprehensive and understandable. A job Well done by the group
Nice piece, thanks for painstakingly organizing this concise notes, God bless you
Very educative and simple to understand. Thank you for the effort
This is very handy. Your work is appreciated
This is an excellent work . I was having lectures just now on nursing diagnosis and care plan and this note helps me a lot
Its so helpful. Thank you!
Very good content. Happy to learn the Nursing diagnosis. Thanks Nurseslabs
This is a great educative article, kind of review of the nursing diagnosis. Thanks a lot for refreshing my memory.
Sorry, it’s not.
This was so simple and very helpful
So simple, concise and very helpful.
I APPRECIATE THIS WORK, USEFUL AND EASY TO UNDERSTAND.
Beautiful. I love the nursing care plan links. it is just what I have been searching for to assist my students. Thank you
I’ve been a nurse (currently working PRN) since 2015 and not having used nursing diagnosis in my day to day, this source was super helpful and a great refresher! Much thanks to the author!
Thanks for this it was very good and easy to comprehend
Thank you for your opinion; however, I agree with Mebratu. The description shown in your article for statement of “risk for” problem is confusing to me.
My view is as follows: “Actual problem” has 3 parts: nursing diagnosis (client’s problem) related to etiology (pathophysiology of what is causing the problem) as evidenced by defining characteristics (signs and symptoms of the problem)
“Risk for problem” has 2 parts: nursing diagnosis (client’s potential problem) related to etiology (client condition that may cause the problem) There is no “as evidenced by” because there IS no evidence of the problem since the problem does not yet exist.
Very nice and easy explanation, thanku
Please I need the actual manual that’s currently being used or at least a link to it -the NANDA-I document.
For the most current NANDA-I Nursing Diagnosis manual, you might want to check out the latest edition of the “Nursing Diagnosis Handbook” by NANDA International. This handbook is frequently updated with new diagnoses and guidelines.
congratulations MATT VERA, for the very nice and usefully presentation in nursing diagnosis. it has been very usefully for patient care and teaching activities. simple and very nice understandable.
Thanks a lot Matt Vera for the simplicity of the nursing diagnoses. Continue with other pieces of work
You’re welcome! I’m thrilled to hear you found the simplicity of the nursing diagnoses helpful. Your encouragement means a lot, and I’m definitely motivated to keep creating and simplifying more content for you and others in the nursing community.
If there are any specific topics or areas you’d like to see covered next, please let me know. Your feedback is invaluable in guiding the work I do.
Really interesting I thank you
Very impressive step by step explanations
Its good explanation. how to download
Really helpful Thank you
Hi Aneena, You’re welcome! I’m glad to hear you found the nursing diagnosis guide helpful. Is there a particular area or diagnosis you’d like to explore more deeply, or do you have any other questions about nursing diagnoses? Always here to help!
what a wonderful text,i really love it…….
Thank you for this material. It is much easier to understand and will be useful to both teachers and students.
Leave a Comment Cancel reply
NANDA: How to Write a Nursing Diagnosis

What is a nursing diagnosis?
A nursing diagnosis is a clinical judgment concerning human response to health conditions/life processes, or vulnerability for that response, by an individual, family, group, or community. A nursing diagnosis provides the basis for the selection of nursing interventions to achieve outcomes for which the nurse has accountability. Nursing diagnoses are developed based on data obtained during the nursing assessment and enable the nurse to develop the care plan. Medical and nursing diagnoses have different goals: a medical diagnosis identifies a variation from a norm, while a nursing diagnosis should judge the existence of a potential for enhancing self-care.
Purposes of Nursing Diagnosis
The purpose of the nursing diagnosis is as follows:
- Helps identify nursing priorities and help direct nursing interventions based on identified priorities.
- Helps the formulation of expected outcomes for quality assurance requirements of third-party payers.
- Nursing diagnoses help identify how a client or group responds to actual or potential health and life processes and knowing their available resources of strengths that can be drawn upon to prevent or resolve problems.
- Provides a common language and forms a basis for communication and understanding between nursing professionals and the healthcare team.
- Provides a basis of evaluation to determine if nursing care was beneficial to the client and cost-effective.
- For nursing students, nursing diagnoses are an effective teaching tool to help sharpen their problem-solving and critical thinking skills.
Difference between Medical and Nursing Diagnoses
The term nursing diagnosis is associated with three different concepts. It may refer to the distinct second step in the nursing process, diagnosis. Also, nursing diagnosis applies to the label when nurses assign meaning to collected data appropriately labeled with NANDA -I-approved nursing diagnosis. For example, during the assessment, the nurse may recognize that the client is feeling anxious, fearful, and finds it difficult to sleep. It is those problems which are labeled with nursing diagnoses: respectively, Anxiety, Fear, and Disturbed Sleep Pattern. Lastly, a nursing diagnosis refers to one of many diagnoses in the classification system established and approved by NANDA. In this context, a nursing diagnosis is based upon the response of the patient to the medical condition. It is called a ‘nursing diagnosis’ because these are matters that hold a distinct and precise action that is associated with what nurses have autonomy to take action about with a specific disease or condition. This includes anything that is a physical, mental, and spiritual type of response. Hence, a nursing diagnosis is focused on care.
Comparison of Nursing and Medical Diagnoses
Nursing diagnoses vs medical diagnoses
A medical diagnosis, on the other hand, is made by the physician or advance health care practitioner that deals more with the disease, medical condition, or pathological state only a practitioner can treat. Moreover, through experience and know-how, the specific and precise clinical entity that might be the possible cause of the illness will then be undertaken by the doctor, therefore, providing the proper medication that would cure the illness. Examples of medical diagnoses are Diabetes Mellitus, Tuberculosis, Amputation, Hepatitis, and Chronic Kidney Disease. The medical diagnosis normally does not change. Nurses are required to follow the physician’s orders and carry out prescribed treatments and therapies.
As explained above, now it is easier to distinguish nursing diagnosis from that of a medical diagnosis. Nursing diagnosis is directed towards the patient and his physiological and psychological response. A medical diagnosis, on the other hand, is particular with the disease or medical condition. Its center is on the illness.
NANDA International (NANDA-I)
NANDA–International earlier known as the North American Nursing Diagnosis Association (NANDA) is the principal organization for defining, distribution and integration of standardized nursing diagnoses worldwide.
The term nursing diagnosis was first mentioned in the nursing literature in the 1950s. Two faculty members of Saint Louis University, Kristine Gebbie and Mary Ann Lavin, recognized the need to identify nurses’ role in an ambulatory care setting. In 1973, NANDA’s first national conference was held to formally identify, develop, and classify nursing diagnoses. Subsequent national conferences occurred in 1975, in 1980, and every two years thereafter. In recognition of the participation of nurses in the United States and Canada, in 1982 the group accepted the name North American Nursing Diagnosis Association (NANDA).
In 2002, NANDA became NANDA International (NANDA-I) in response to its significant growth in membership outside of North America. The acronym NANDA was retained in the name because of its recognition.
Review, refinement, and research of diagnostic labels continue as new and modified labels are discussed at each biennial conference. Nurses can submit diagnoses to the Diagnostic Review Committee for review. The NANDA-I board of directors give the final approval for incorporation of the diagnosis into the official list of labels. As of 2020, NANDA-I has approved 244 diagnoses for clinical use, testing, and refinement. READ: How To Become An Auxiliary Nurse In Nigeria
History and Evolution of Nursing Diagnosis
In this section, we’ll look at the events that led to the evolution of nursing diagnosis today:
The need for nursing to earn its professional status, the increasing use of computers in hospitals for accreditation documentation, and the demand for a standardized language from nurses lead to the development of nursing diagnosis.
Post-World War II America saw an increase in the number of nurses returning from military service. These nurses were highly skilled in treating medical diagnoses with physicians. Returning to peacetime practice, nurses were faced with renewed domination by physicians and social pressures to return to traditionally defined female roles with reduced status to make room in the workforce for returning male soldiers. With that, nurses felt increased pressure to redefine their unique status and value.
Nursing diagnosis was seen as the approach that could provide the “frame of reference from which nurses could determine what to do and what to expect” in a clinical practice situation.
Nursing diagnoses were also intended to define nursing’s unique boundaries with respect to medical diagnoses. For NANDA, the standardization of nursing language through nursing diagnosis was the first step towards having insurance companies pay nurses directly for their care.
In 1953, Virginia Fry and R. Louise McManus introduced the discipline-specific term “nursing diagnosis” to describe a step necessary in developing a nursing care plan.
In 1972, the New York State Nurse Practice Act identified diagnosing as part of the legal domain of professional nursing. The Act was the first legislative recognition of nursing’s independent role and diagnostic function.
In 1973, the development of nursing diagnosis formally began when two faculty members of the Saint Louis University, Kristine Gebbie and Mary Ann Lavin, perceived a need to identify nurses’ roles in ambulatory care settings. In the same year, the first national conference to identify nursing diagnoses was sponsored by the Saint Louis University School of Nursing and Allied Health Profession in 1973.
Also in 1973, the American Nurses Association’s Standards of Practice included diagnosing as a function of professional nursing. Diagnosing was subsequently incorporated into the component of the nursing process. The nursing process was used to standardize and define the concept of nursing care, hoping that it would help to earn professional status.
In 1980, the American Nurses Association (ANA) Social Policy Statement defined nursing as: “the diagnosis and treatment of human response to actual or potential health problems.”
International recognition of the conferences and the development of nursing diagnosis came with the First Canadian Conference in Toronto (1977) and the International Nursing Conference (1987) in Alberta, Canada.
In 1982, the conference group accepted the name “North American Nursing Diagnosis Association (NANDA)” to recognize the participation and contribution of nurses in the United States and Canada. In the same year, the newly formed NANDA used Sr. Callista Roy’s “nine patterns of unitary man” as an organizing principle since the first taxonomy listed nursing diagnosis alphabetically – which was deemed unscientific.
In 1984, NANDA renamed “patterns of unitary man” as “human response patterns” based on the work of Marjorie Gordon. Currently, the taxonomy is now called Taxonomy II.
In 1990 during the 9th conference of NANDA, the group approved an official definition of nursing diagnosis:
“Nursing diagnosis is a clinical judgment about individual, family, or community responses to actual or potential health problems/life processes. Nursing diagnosis provides the basis for selection of nursing interventions to achieve outcomes for which the nurse is accountable.”
In 1997, NANDA changed the name of its official journal from “Nursing Diagnosis” to “Nursing Diagnosis: The International Journal of Nursing Terminologies and Classifications.”
In 2002, NANDA changed its name to NANDA International (NANDA-I) to further reflect the worldwide interest in nursing diagnosis. In the same year, Taxonomy II was released based on the revised version of Gordon’s Functional health patterns. As of 2018, NANDA-I has approved 244 diagnoses for clinical use, testing, and refinement.
Classification of Nursing Diagnoses (Taxonomy II)
How are nursing diagnoses listed , arranged or classified? In 2002, Taxonomy II was adopted, which was based from the Functional Health Patterns assessment framework of Dr. Mary Joy Gordon. Taxonomy II has three levels: Domains (13), Classes (47), and nursing diagnoses. Nursing diagnoses are no longer grouped by Gordon’s patterns but coded according to seven axes: diagnostic concept, time, unit of care, age, health status, descriptor, and topology. In addition, diagnoses are now listed alphabetically by its concept, not by the first word.
Nursing Diagnosis Taxonomy II
Taxonomy II for nursing diagnosis contains 13 domains and 47 classes. Image via: Wikipedia.com
Domain 1. Health Promotion
Class 1. Health Awareness
Class 2. Health Management
Domain 2. Nutrition
Class 1. Ingestion
Class 2. Digestion
Class 3. Absorption
Class 4. Metabolism
Class 5. Hydration
Domain 3. Elimination and Exchange
Class 1. Urinary function
Class 2. Gastrointestinal function
Class 3. Integumentary function
Class 4. Respiratory function
Domain 4. Activity/Rest
Class 1. Sleep/Rest
Class 2. Activity/Exercise
Class 3. Energy balance
Class 4. Cardiovascular/Pulmonary responses
Class 5. Self-care
Domain 5. Perception/Cognition
Class 1. Attention
Class 2. Orientation
Class 3. Sensation/Perception
Class 4. Cognition
Class 5. Communication
Domain 6. Self-Perception
Class 1. Self-concept
Class 2. Self-esteem
Class 3. Body image
Domain 7. Role relationship
Class 1. Caregiving roles
Class 2. Family relationships
Class 3. Role performance
Domain 8. Sexuality
Class 1. Sexual identity
Class 2. Sexual function
Class 3. Reproduction
Domain 9. Coping/stress tolerance
Class 1. Post-trauma responses
Class 2. Coping responses
Class 3. Neurobehavioral stress
Domain 10. Life principles
Class 1. Values
Class 2. Beliefs
Class 3. Value/Belief/Action congruence
Domain 11. Safety/Protection
Class 1. Infection
Class 2. Physical injury
Class 3. Violence
Class 4. Environmental hazards
Class 5. Defensive processes
Class 6. Thermoregulation
Domain 12. Comfort
Class 1. Physical comfort
Class 2. Environmental comfort
Class 3. Social comfort
Domain 13. Growth/Development
Class 1. Growth
Class 2. Development
Nursing Process
The five stages of the nursing process are assessment, diagnosing, planning, implementation, and evaluation. In the diagnostic process, the nurse is required to have critical thinking. Apart from the understanding of nursing diagnoses and their definitions, the nurse promotes awareness of defining characteristics and behaviors of the diagnoses, related factors to the selected nursing diagnoses, and the interventions suited for treating the diagnoses.
The Nursing Process, also known as the “ADPIE”
What data is collected? The first step of the nursing process is called assessment. When the nurse first encounters a patient, the former is expected to perform an assessment to identify the patient’s health problems as well as the physiological, psychological, and emotional state. The most common approach to gathering important information is through an interview. Physical examinations, referencing a patient’s health history, obtaining a patient’s family history, and general observation can also be used to collect assessment data.
What is the problem? Once the assessment is completed, the second step of the nursing process is where the nurse will take all the gathered information into consideration and diagnose the patient’s condition and medical needs. Diagnosing involves a nurse making an educated judgment about a potential or actual health problem with a patient. More than one diagnoses are sometimes made for a single patient.
How to manage the problem? When the nurse, any supervising medical staff, and the patient agree on the diagnosis, the nurse will plan a course of treatment that takes into account short- and long-term goals. Each problem is committed to a clear, measurable goal for the expected beneficial outcome. The planning step of the nursing process is discussed in detail in Nursing Care Plans (NCP): Ultimate Guide and Database.
Implementation
Putting the plan into action. The implementation phase of the nursing process is when the nurse put the treatment plan into effect. This typically begins with the medical staff conducting any needed medical interventions. Interventions should be specific to each patient and focus on achievable outcomes. Actions associated in a nursing care plan include monitoring the patient for signs of change or improvement, directly caring for the patient or conducting important medical tasks, educating and guiding the patient about further health management, and referring or contacting the patient for a follow-up.
Did the plan work? Once all nursing intervention actions have taken place, the team now learns what works and what doesn’t by evaluating what was done beforehand. The possible patient outcomes are generally explained under three terms: the patient’s condition improved, the patient’s condition stabilized, and the patient’s condition worsened. Accordingly, evaluation is the last, but if goals were not sufficed, the nursing process begins again from the first step.
Types of Nursing Diagnoses
The four types of NANDA nursing diagnosis are Actual (Problem-Focused), Risk, Health promotion, and Syndrome. Here are the four categories of nursing diagnosis provided by the NANDA-I system.
Four Types of Nursing Diagnoses
The four types of nursing diagnosis are Actual (Problem-Focused), Risk, Health promotion, and Syndrome.
Problem-Focused Nursing Diagnosis
A problem-focused diagnosis (also known as actual diagnosis) is a client problem that is present at the time of the nursing assessment. These diagnoses are based on the presence of associated signs and symptoms. Actual nursing diagnoses should not be viewed as more important than risk diagnoses. There are many instances where a risk diagnosis can be the diagnosis with the highest priority for a patient.
Problem-focused nursing diagnoses have three components: (1) nursing diagnosis, (2) related factors, and (3) defining characteristics. Examples of actual nursing diagnosis are:
- Ineffective Breathing Pattern
- Impaired Skin Integrity.
Risk Nursing Diagnosis
The second type of nursing diagnosis is called risk nursing diagnosis. These are clinical judgment that a problem does not exist, but the presence of risk factors indicates that a problem is likely to develop unless nurses intervene. The individual (or group) is more susceptible to develop the problem than others in the same or a similar situation because of risk factors. For example, an elderly client with diabetes and vertigo has difficulty walking refuses to ask for assistance during ambulation may be appropriately diagnosed with Risk for Injury.
Components of a risk nursing diagnosis include: (1) risk diagnostic label, and (2) risk factors. Examples of risk nursing diagnosis are:
- Risk for Falls
- Risk for Injury
Health Promotion Diagnosis
Health promotion diagnosis (also known as wellness diagnosis) is a clinical judgment about motivation and desire to increase well-being. Health promotion diagnosis is concerned in the individual, family, or community transition from a specific level of wellness to a higher level of wellness.
Components of a health promotion diagnosis generally include only the diagnostic label or a one-part-statement. Examples of health promotion diagnosis:
- Readiness for Enhanced Spiritual Well Being
- Readiness for Enhanced Family Coping
- Readiness for Enhanced Parenting
Syndrome Diagnosis
A syndrome diagnosis is a clinical judgment concerning with a cluster of problem or risk nursing diagnoses that are predicted to present because of a certain situation or event.
They, too, are written as a one-part statement requiring only the diagnostic label. Examples of a syndrome nursing diagnosis are:
- Chronic Pain Syndrome
- Post-trauma Syndrome
- Frail Elderly Syndrome
Possible Nursing Diagnosis
A possible nursing diagnosis is not a type of diagnosis as are actual, risk, health promotion, and syndrome. Possible nursing diagnoses are statements describing a suspected problem for which additional data are needed to confirm or rule out the suspected problem. It provides the nurse with the ability to communicate with other nurses that a diagnosis may be present but additional data collection is indicated to rule out or confirm the diagnosis. Examples include
- Possible Chronic Low Self-Esteem
- Possible Social Isolation.
Components of a Nursing Diagnosis
A nursing diagnosis has typically three components: (1) the problem and its definition, (2) the etiology, and (3) the defining characteristics.
Components of a Nursing Diagnosis Statement
A common format used when writing or formulating nursing diagnosis is the PES format.
Problem and Definition
The problem statement, or the diagnostic label, describes the client’s health problem or response for which nursing therapy is given as concisely as possible. A diagnostic label usually has two parts: qualifier and focus of the diagnosis. Qualifiers (also called modifiers) are words that have been added to some diagnostic labels to give additional meaning, limit or specify the diagnostic statement. Exempted in this rule are one-word nursing diagnoses (e.g., Anxiety, Fatigue, Nausea) where their qualifier and focus are inherent in the one term.
The etiology, or related factors and risk factors, component of a nursing diagnosis label identifies one or more probable causes of the health problem, are the conditions involved in the development of the problem, gives direction to the required nursing therapy, and enables the nurse to individualize the client’s care. Nursing interventions should be aimed at etiological factors in order to remove the underlying cause of the nursing diagnosis. Etiology is linked with the problem statement with the phrase “as related to”.
Defining Characteristics
Defining characteristics are the clusters of signs and symptoms that indicate the presence of a particular diagnostic label. In actual nursing diagnoses, the defining characteristics are the identified signs and symptoms of the client. For risk nursing diagnosis, no signs and symptoms are present therefore the factors that cause the client to be more susceptible to the problem form the etiology of a risk nursing diagnosis. Defining characteristics are written “as evidenced by” or “as manifested by” in the diagnostic statement.
How to Write a Nursing Diagnosis?
In writing nursing diagnostic statements, describe the health status of an individual and the factors that have contributed to the status. You do not need to include all types of diagnostic indicators. Diagnostic statements can be one-part, two-part, or three-part statements. A common format used when writing or formulating nursing diagnosis is the PES format.
Writing Diagnostic Statements
Nursing diagnostic statements can be one-part, two-part, or three-part statements
One-Part Nursing Diagnosis Statement
Health promotion nursing diagnoses are usually written as one-part statements because related factors are always the same: motivated to achieve a higher level of wellness though related factors may be used to improve the of the chosen diagnosis. Syndrome diagnoses also have no related factors. Examples of one-part nursing diagnosis statement include:
- Readiness for Enhance Breastfeeding
- Readiness for Enhanced Coping
- Rape Trauma Syndrome
Two-Part Nursing Diagnosis Statement
Risk and possible nursing diagnoses have two-part statements: the first part is the diagnostic label and the second is the validation for a risk nursing diagnosis or the presence of risk factors. It’s not possible to have a third part for risk or possible diagnoses because signs and symptoms do not exist. Examples of two-part nursing diagnosis statement include:
- Risk for Infection related to compromised host defenses
- Risk for Injury related to abnormal blood profile
- Possible Social Isolation related to unknown etiology
- Three-part Nursing Diagnosis Statement
An actual or problem nursing diagnosis have three-part statements: diagnostic label, contributing factor (“related to”), and signs and symptoms (“as evidenced by”). Three-part nursing diagnosis statement is also called the PES format which includes the Problem, Etiology, and Signs and Symptoms. Examples of three-part nursing diagnosis statement include:
Impaired Physical Mobility related to decreased muscle control as evidenced by inability to control lower extremities.
Acute Pain related to tissue ischemia as evidenced by statement of “I feel severe pain on my chest!”
References and Sources
References for this Nursing Diagnosis guide and recommended resources to further your reading.
Ackley, B. J., & Ladwig, G. B. (2010). Nursing Diagnosis Handbook-E-Book: An Evidence-Based Guide to Planning Care. Elsevier Health Sciences. [Link]
Berman, A., Snyder, S., & Frandsen, G. (2016). Kozier & Erb’s Fundamentals of Nursing: Concepts, process and practice. Boston, MA: Pearson. [Link]
Edel, M. (1982). The nature of nursing diagnosis. In J. Carlson, C. Craft, & A. McGuire (Eds.), Nursing diagnosis (pp. 3-17). Philadelphia: Saunders.
Fry, V. (1953). The Creative approach to nursing. AJN, 53(3), 301-302.
Gordon, M. (1982). Nursing diagnosis: Process and application. New York: McGraw-Hill.
Gebbie, K., & Lavin, M. (1975.) Classification of nursing diagnoses: Proceedings of the First National Conference. St. Louis, MO: Mosby.
McManus, R. L. (1951). Assumption of functions in nursing. In Teachers College, Columbia University, Regional planning for nurses and nursing education. New York: Columbia University Press.
For the Complete List of NANDA-I Nursing Diagnosis: Herdman, H. T., & Kamitsuru, S. (Eds.). (2017). NANDA International Nursing Diagnoses: Definitions & Classification 2018-2020. Thieme. [Link]
NANDA. International. (2014). Nursing Diagnoses 2012-14: Definitions and Classification. Wiley.
Powers, P. (2002). A discourse analysis of nursing diagnosis. Qualitative health research, 12(7), 945-965. [Scribd]
Related posts:

Leave a Reply (Cancel reply)
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Please enable JavaScript! Bitte aktiviere JavaScript! S'il vous plaît activer JavaScript! Por favor,activa el JavaScript! antiblock.org

Nursing Diagnosis: A Comprehensive Guide and List
Nursing diagnosis is an essential component of nursing practice that helps nurses identify actual or potential health problems and formulate individualized care plans for their patients.
Definition of Nursing Diagnosis
Nursing diagnosis is a clinical judgment made by nurses based on data collected during a patient assessment. It identifies actual or potential health problems and their related factors, including physical, psychological, social, and environmental factors. Nursing diagnosis is used to guide nursing interventions and evaluate patient outcomes.
List of Nursing Diagnosis
Imbalanced nutrition: less than body requirements
Risk for infection
Hypothermia
Hyperthermia
Ineffective thermoregulation
Autonomic dysreflexia
Risk for autonomic dysreflexia
Constipation
Perceived constipation
Risk for constipation
Impaired urinary elimination
Stress urinary incontinence
Urge urinary incontinence
Risk for urge urinary incontinence
Urinary retention
Risk for imbalanced fluid volume
Excess fluid volume
Deficient fluid volume
Risk for deficient fluid volume
Decreased cardiac output
Impaired gas exchange
Ineffective airway clearance
Ineffective breathing pattern
Impaired spontaneous ventilation
Dysfunctional ventilatory weaning response
Risk for injury
Risk for suffocation
Risk for poisoning
Risk for physical trauma
Risk for aspiration
Risk for disuse syndrome
Risk for latex allergy reaction
Ineffective protection
Impaired tissue integrity
Impaired oral mucous membrane integrity
Impaired skin integrity
Risk for impaired skin integrity
Impaired dentition
Impaired verbal communication
Impaired social interaction
Social isolation
Risk for loneliness
Ineffective role performance
Impaired parenting
Risk for impaired parenting
Risk for impaired attachment
Sexual dysfunction
Interrupted family processes
Caregiver role strain
Risk for caregiver role strain
Dysfunctional family processes
Parental role conflict
Ineffective sexuality pattern
Spiritual distress
Risk for spiritual distress
Readiness for enhanced spiritual wellbeing
Ineffective coping
Defensive coping
Ineffective denial
Disabled family coping
Compromised family coping
Readiness for enhanced family coping
Readiness for enhanced community coping
Ineffective community coping
Decisional conflict
Impaired physical mobility
Risk for peripheral neurovascular dysfunction
Risk for perioperative positioning injuryc
Impaired walking
Impaired wheelchair mobility
Impaired transfer ability
Impaired bed mobility
Sleep deprivation
Decreased diversional activity engagement
Delayed surgical recovery
Feeding self-care deficit
Impaired swallowing
Ineffective breastfeeding
Interrupted breastfeeding
Readiness for enhanced breastfeeding
Bathing self-care deficit
Dressing self-care deficit
Toileting self-care deficit
Relocation stress syndrome
Risk for disorganized infant behavior
Disorganized infant behavior
Readiness for enhanced organized infant behavior
Disturbed body image
Chronic low self-esteem
Situational low self-esteem
Disturbed personal identity
Unilateral neglect
Hopelessness
Powerlessness
Deficient knowledge
Acute confusion
Chronic confusion
📖 Impaired memory ✍
📖 Nursing diagnosis Acute pain ✍
📖 Nursing diagnosis Chronic pain ✍
📖 Nursing diagnosis Nausea ✍
Chronic sorrow
Risk for other-directed violence
Risk for self-mutilation
Risk for self-directed violence
Post-trauma syndrome
Rape-trauma syndrome
Risk for post-trauma syndrome
Death anxiety
Risk for relocation stress syndrome
Self-mutilation
Risk for powerlessness
Risk for situational low self-esteem
Risk for sudden infant death
Readiness for enhanced communication
Readiness for enhanced coping
Readiness for enhanced family processes
Readiness for enhanced knowledge
Readiness for enhanced nutritiona
Readiness for enhanced parenting
Readiness for enhanced sleep
Readiness for enhanced self-concept
Sedentary lifestyle
Impaired religiosity
Risk for impaired religiosity
Readiness for enhanced religiosity
Risk for acute confusion
Risk for compromised human dignity
Moral distress
Stress overload
Risk for impaired liver function
Risk for unstable blood glucose level
Risk for contamination
Contamination
Readiness for enhanced self-care
Readiness for enhanced comfort
Readiness for enhanced decision-making
Readiness for enhanced hope
Readiness for enhanced power
Risk-prone health behavior
Self-neglect
Neonatal hyperbilirubinemia
Risk for electrolyte imbalance
Dysfunctional gastrointestinal motility
Risk for dysfunctional gastrointestinal motility
Disturbed sleep pattern
Ineffective activity planning
Risk for decreased cardiac tissue perfusion
Risk for ineffective cerebral tissue perfusion
Ineffective peripheral tissue perfusion
Risk for shock
Risk for bleeding
Readiness for enhanced relationship
Readiness for enhanced childbearing process
Risk for disturbed maternal-fetal dyad
Impaired resilience
Risk for impaired resilience
Readiness for enhanced resilience
Risk for vascular trauma
Impaired comfort
Deficient community health
Insufficient breast milk production
Risk for allergy reaction
Risk for adverse reaction to iodinated contrast media
Risk for dry eye
Risk for thermal injuryc
Ineffective childbearing process
Ineffective impulse control
Ineffective relationship
Risk for chronic low self-esteem
Risk for disturbed personal identity
Risk for ineffective activity planning
Risk for ineffective childbearing process
Risk for ineffective peripheral tissue perfusion
Risk for ineffective relationship
Risk for neonatal hyperbilirubinemia
Risk for frail elderly syndrome
Risk for overweight
Chronic functional constipation
Risk for chronic functional constipation
Impaired sitting
Impaired standing
Risk for decreased cardiac output
Impaired mood regulation
Impaired emancipated decision-making
Readiness for enhanced emancipated decision-making
Risk for impaired emancipated decisionmaking
Risk for corneal injury
Risk for delayed surgical recovery
Risk for impaired oral mucous membrane integrity
Risk for impaired tissue integrity
Risk for urinary tract injury
Labile emotional control
Risk for hypothermia
Risk for perioperative hypothermia
Chronic pain syndromed
Labor paind
Frail elderly syndrome
Acute substance withdrawal syndrome
Risk for acute substance withdrawal syndrome
Risk for complicated immigration transition
Risk for dry mouth
Readiness for enhanced health literacy
Neonatal abstinence syndrome
Risk for occupational injury
Risk for surgical site infection
Risk for unstable blood pressure
Ineffective adolescent eating dynamics
Ineffective child eating dynamics
Ineffective infant feeding dynamics
Risk for female genital mutilation
Imbalanced energy field
Risk for ineffective thermoregulation
Ineffective health self-management
Ineffective dry eye self-management
Ineffective lymphedema self-management
Disturbed thought process
Neonatal hypothermia
Risk for ineffective lymphedema selfmanagement
Risk for neonatal hypothermia
Disturbed family identity syndrome
Risk for disturbed family identity syndrome
Readiness for enhanced grieving
Risk for child pressure injury
Neonatal pressure injury
Risk for neonatal pressure injury
Risk for suicidal behavior
Risk for elopement attempt
Risk for thrombosis
Ineffective health maintenance behaviors
Readiness for enhanced health selfmanagement
Ineffective family health self-management
Ineffective infant suck-swallow response
Risk for metabolic syndrome
Disability-associated urinary incontinence
Decreased activity tolerance
Risk for decreased activity tolerance
Ineffective home maintenance behaviors
Maladaptive grieving
Risk for maladaptive grieving
Risk for adult falls
Risk for adult pressure injury
Risk for delayed child development
Risk for child falls
Readiness for enhanced exercise engagement
Risk for ineffective home maintenance behaviors
Readiness for enhanced home maintenance behaviors
Mixed urinary incontinence
Risk for impaired cardiovascular function
Adult pressure injury
Child pressure injury
Delayed child development
Delayed infant motor development
Risk for delayed infant motor development
Dysfunctional adult ventilatory weaning response
Impaired bowel continence
Nipple-areolar complex injury
Risk for nipple-areolar complex injury
Risk for urinary retention
Types of Nursing Diagnosis
There are three types of nursing diagnosis:
Actual Nursing Diagnosis
An actual nursing diagnosis describes a current problem that is present in the patient. This type of nursing diagnosis is based on clinical signs and symptoms, laboratory results, and other objective data. An example of an actual nursing diagnosis is "Impaired Gas Exchange related to pneumonia as evidenced by shortness of breath and decreased oxygen saturation."
Risk Nursing Diagnosis
A risk nursing diagnosis describes a potential problem that the patient is at risk for developing. This type of nursing diagnosis is based on risk factors identified during the patient assessment. An example of a risk nursing diagnosis is "Risk for Falls related to unsteady gait and history of falls."
Health Promotion Nursing Diagnosis
A health promotion nursing diagnosis describes a patient's motivation and desire to improve their health and wellbeing. This type of nursing diagnosis is based on patient strengths and resources. An example of a health promotion nursing diagnosis is "Readiness for Enhanced Nutrition related to increased knowledge and motivation to improve dietary habits."
Process of Nursing Diagnosis
The nursing diagnosis process involves several steps:
The first step in the nursing diagnosis process is to collect data about the patient's physical, psychological, social, and environmental status. This information can be gathered through observation, physical examination, interviews, and medical records review.
Data Analysis
After collecting data, nurses analyze it to identify patterns, problems, and potential health risks. They use critical thinking and clinical judgment to interpret the data and make informed decisions about nursing diagnoses.
The nursing diagnosis is formulated based on the data analysis. Nurses use standardized nursing language, such as NANDA-I (North American Nursing Diagnosis Association International), to identify the problem and related factors.
After formulating the nursing diagnosis, nurses develop a comprehensive care plan that addresses the patient's specific needs, goals, and interventions. The plan should be individualized and based on the patient's preferences and values.
Implementation
The care plan is implemented through nursing interventions that aim to achieve the goals and improve the patient's health status. Nurses monitor the patient's response to interventions and modify the plan as needed.
The final step in the nursing diagnosis process is to evaluate the effectiveness of the care plan and interventions. Nurses assess the patient's progress towards achieving goals and modify the plan if necessary.
Importance of Nursing Diagnosis
Nursing diagnosis is essential for several reasons:
Individualized Care
Nursing diagnosis helps nurses identify individual patient needs and develop care plans that are tailored to their specific problems, strengths, and preferences.
Efficient Resource Allocation
Nursing diagnosis helps nurses prioritize care interventions and allocate resources effectively. It ensures that resources are used efficiently and effectively to achieve the best patient outcomes.
Improved Patient Outcomes
Nursing diagnosis improves patient outcomes by providing targeted and individualized care that addresses their specific health problems and needs. It helps prevent complications and promotes faster recovery.
Professional Development
Nursing diagnosis is a critical thinking process that requires nurses to analyze data, interpret findings, and make informed decisions. It enhances their clinical judgment skills and promotes their professional development as competent and skilled healthcare providers.
Collaboration with Interdisciplinary Team
Nursing diagnosis facilitates collaboration with the interdisciplinary healthcare team. It enables nurses to communicate effectively with physicians, pharmacists, and other healthcare providers to ensure that the patient receives comprehensive and coordinated care.
Challenges in Nursing Diagnosis
Despite the benefits of nursing diagnosis, several challenges can hinder its effective implementation. These challenges include:
Lack of Knowledge and Skills
Some nurses may lack the knowledge and skills required to perform an accurate and comprehensive patient assessment, analyze data, and formulate a nursing diagnosis. This can compromise the quality of care and patient outcomes.
Time Constraints
Nurses may face time constraints that limit their ability to collect and analyze data thoroughly, formulate a nursing diagnosis, and develop a comprehensive care plan. This can result in incomplete or inadequate care.
Communication Barriers
Effective nursing diagnosis requires communication and collaboration with the patient and the interdisciplinary healthcare team. Communication barriers, such as language differences, cultural differences, and communication disorders, can hinder effective nursing diagnosis.
In conclusion, nursing diagnosis is an essential component of nursing practice that helps nurses identify actual or potential health problems, develop individualized care plans, and promote better patient outcomes. The nursing diagnosis process involves several steps, including assessment, data analysis, diagnosis, planning, implementation, and evaluation. Although nursing diagnosis has many benefits, several challenges, such as lack of knowledge and skills, time constraints, and communication barriers, can hinder its effective implementation.
Who can perform a nursing diagnosis?
- Nurses who have completed a nursing program and obtained a license to practice can perform a nursing diagnosis.
What is the difference between a medical diagnosis and a nursing diagnosis?
- A medical diagnosis identifies a disease or condition, while a nursing diagnosis identifies a patient's response to a disease or condition.
Can a nursing diagnosis change over time?
- Yes, a nursing diagnosis can change over time as the patient's health status and needs change.
How can nurses overcome time constraints when performing a nursing diagnosis?
- Nurses can prioritize data collection and analysis, delegate non-nursing tasks to other healthcare providers, and use technology to streamline the nursing diagnosis process.
Can patients be involved in the nursing diagnosis process?
- Yes, patients can be involved in the nursing diagnosis process by providing information about their health status, preferences, and goals.

NurseStudy.Net
Nursing Education Site
Nursing Diagnosis Guide and Nursing Care Plan
Nursing diagnosis guide.
Nursing diagnosis is a clinical judgment about a person’s, families, groups, or community response to health conditions/life processes or vulnerability to that response.
A nursing diagnosis serves as the foundation for deciding which nursing actions to use in order to accomplish outcomes for which the nurse is responsible.
Nursing diagnoses are made based on the information gathered during the nursing assessment and allow the nurse to create a care plan. The development and implementation of a nursing diagnosis help nurses determine the best course of treatment for their patients.
Nursing diagnoses are created after thoughtful consideration of a patient’s physical assessment. They can be used to track the patient’s care plan’s progress and influence the possible intervention for the patient, family, and community. Some nurses may regard nursing diagnoses as archaic and time-consuming. It is, nevertheless, an essential tool for promoting patient safety through the use of evidence-based nursing research.
Purpose of Nursing Diagnosis
According to NANDA International, a nursing diagnosis is “a judgment based on a comprehensive nursing evaluation.” It is based on the patient’s current status and health assessment, allowing nurses and other healthcare providers to see a patient holistically.
The following are the purposes of nursing diagnosis:
- It helps identify nursing priorities and the direction of nursing interventions based on identified priorities.
- It assists in formulating expected outcomes for third-party payer quality assurance requirements.
- It helps determine how a client or group reacts to current or projected health and life processes and identifies the strengths that may be used to prevent or resolve problems.
- It provides a common language and forms a basis for communication between the nursing professionals and the healthcare team to communicate and comprehend one another.
- It provides a foundation for determining whether nursing treatment was beneficial and cost-effective for the patient.
- It is an effective teaching tool for nursing students who want to improve their problem-solving and critical thinking skills.
- An accurate nursing diagnosis provides patient safety, excellent care, and enhanced reimbursement from commercial health insurance, Medicare, and Medicaid.
History of Nursing Diagnosis
NANDA–International, formerly known as the North American Nursing Diagnosis Association (NANDA), is the leading organization for defining, disseminating, and integrating standardized nursing diagnoses worldwide.
In the 1950s, the term “nursing diagnosis” was first used in nursing literature. Kristine Gebbie and Mary Ann Lavin, both of Saint Louis University, saw the need to define the role of nurses in ambulatory care settings. The first national meeting of the NANDA was convened in 1973 to identify, create, and classify nursing diagnoses formally.
National conferences were held in 1975, 1980, and every two years after that. In 1982, the association adopted the name North American Nursing Diagnosis Association (NANDA) to acknowledge the involvement of nurses from the United States and Canada. NANDA was renamed NANDA International (NANDA-I) in 2002 due to its significant membership growth outside of North America.
Because of its prominence, the acronym NANDA was retained in the name. Each biennial conference continues to review, develop, and investigate diagnostic labels, with new and updated labels being considered. Nurses can submit diagnoses to the Diagnostic Review Committee for review.
The NANDA-I board of directors gives final approval for the diagnosis to be added to the official label list. NANDA-I approved 267 diagnoses for clinical use, testing, and refining as of 2021
According to its website, NANDA international’s mission is as follows:
- To determine interventions and outcomes, provide the world’s leading evidence-based nursing diagnoses for use in practice.
- Integrate evidence-based terminology into clinical practice and clinical decision-making to improve patient safety.
- Helps to fund research through the NANDA-I Foundation
- Be a vibrant and supportive global network of nurses dedicated to enhancing the quality of nursing care and patient safety via evidence-based practice.
The Evolution of Nursing Diagnosis
- Nursing diagnosis emerged from the need for nurses to gain professional status, the increasing use of computers in hospitals for accrediting documentation, and the demand for a standardized language from nurses.
- Following WWII, the number of nurses returning from military service increased in the United States. These nurses were experts in working with doctors to treat medical diagnoses. When nurses returned to peacetime work, they were confronted with renewed physician dominance and social pressures to return to historically defined female positions with lower status in order to create a way in the workforce for returning male troops. Nurses felt more pressure to redefine their distinct status and value as a result.
- In a clinical practice situation, the nursing diagnosis was considered as the strategy that could provide the “frame of reference from which nurses might choose what to do and what to expect.”
- Nursing diagnoses were also created to establish nursing’s distinct boundaries in relation to medical diagnoses. The first step toward letting insurance companies pay nurses directly for their care, according to NANDA, was to standardize nursing language through nursing diagnosis.
- In 1953, the term “nursing diagnosis” was introduced by Virginia Fry and R. Louise McManus to define a step in the development of a nursing care plan.
- Diagnoses were recognized as part of the legal domain of professional nursing by the New York State Nurse Practice Act in 1972. The Act was the first legislative honor of nursing’s independent role and diagnostic function.
- The development of nursing diagnosis formally began in 1973, when two Saint Louis University faculty members, Kristine Gebbie and Mary Ann Lavin, saw a need to identify nurses’ roles in ambulatory care settings. In the same year, the Saint Louis University School of Nursing and Allied Health Professions hosted the first national conference to identify nursing diagnoses.
- Diagnosing as a function of professional nursing was included in the American Nurses Association’s Standards of Practice in 1973. Diagnosing became a part of the nursing process. The nursing process was developed to standardize and define the concepts of nursing care in the hopes of achieving professional status.
- Nursing was described as “the diagnosis and treatment of human response to real or potential health problems” by the American Nurses Association (ANA) in its Social Policy Statement in 1980.
- The First Canadian Conference in Toronto (1977) and the International Nursing Conference (1987) in Alberta, Canada, brought international credibility to the conferences and the development of nursing diagnosis.
- To recognize the participation and contribution of nurses in the United States and Canada, the conference group accepted the name “North American Nursing Diagnosis Association (NANDA)” in 1982. The newly created NANDA utilized Sr. Callista Roy’s “nine patterns of unitary man” as an organizing principle since the first taxonomy listed nursing diagnosis alphabetically – which was deemed unscientific.
- Based on the work of Marjorie Gordon, NANDA renamed “patterns of unitary man” as “human response patterns” in 1984. Taxonomy II is the current name of the taxonomy.
- During NANDA’s 9th conference in 1990, the organization accepted an official definition of nursing diagnosis.
- NANDA’s official journal, “Nursing Diagnosis” was changed to “Nursing Diagnosis: The International Journal of Nursing Terminologies and Classifications” in 1997.
- NANDA was renamed NANDA International (NANDA-I) in 2002 to better reflect the worldwide interest in nursing diagnosis. Taxonomy II, based on a revised version of Gordon’s Functional health patterns, was released the same year.
- NANDA-I approved 244 diagnoses for clinical use, testing, and refining as of 2018.
- There are 267 approved diagnoses for clinical use, testing, and refining by the year 2021.
Classification of Nursing Diagnoses or Taxonomy II
How are nursing diagnoses organized, categorized, and listed? Taxonomy II, based on Dr. Mary Joy Gordon’s Functional Health Patterns assessment framework, was accepted in 2002.
Domains, Classes, and nursing diagnoses are the three levels of Taxonomy II. Nursing diagnoses are now coded according to seven axes: diagnostic concept, time, unit of care, age, health status, descriptor, and topology, rather than Gordon’s patterns.
Furthermore, diagnoses are now listed alphabetically by concept rather than by the first word.
Types of Nursing Diagnosis
There are four categories of Nursing diagnoses provided by NANDA-I system:
1. Problem-Focused Nursing Diagnosis
A client problem that exists at the time of the nursing assessment is referred to as a problem-focused diagnosis (also known as actual diagnosis).
The presence of associated signs and symptoms is used to make these diagnoses. Actual nursing diagnoses should not be viewed as more important than risk diagnoses. A risk diagnosis can be the highest priority for a patient in many situations.
There are three parts to problem-focused nursing diagnoses: (1) nursing diagnosis, (2) related factors, and (3) defining characteristics. Examples of actual nursing diagnoses are the following:
- Ineffective Breathing Pattern related to pain as evidenced by the use of accessory muscles to breathe, pursed-lip breathing, reports of pain during inhalation, and dyspnea.
- Anxiety related to stress as evidenced by increased tension, nervousness, and verbalization of concern regarding the upcoming surgery.
- Acute Pain related to decreased myocardial flow as evidenced by irritability, verbalization of pain, and guarding behavior.
- Impaired Skin Integrity related to pressure over bony prominence as evidenced by acute pain, breaks on the skin, redness, and wound drainage.
2. Risk Nursing Diagnosis
A risk nursing diagnosis is the second category of nursing diagnosis. Although these are clinical judgments that a problem does not exist, the presence of risk indicators implies that unless nurses intervene, a problem will arise.
Risk diagnoses have no etiological variables or related factors. Because of risk factors, the individual or group is more likely to acquire the condition than others in the same or comparable situation. For example, if an older patient with diabetes and vertigo has difficulties walking and refuses to ask for help, the patient may be classified with Risk for Injury.
A risk nursing diagnosis consists of two parts: (1) a risk diagnostic label and (2) risk factors. The following are some examples of risk nursing diagnoses:
- Risk for Falls as evidenced by body malaise
- Risk for Injury as evidenced by problems in gait and balance
- Risk for Infection as evidenced by immunosuppression
- Risk for Ineffective Childbearing Process
- Risk for Impaired Oral Mucous Membrane Integrity
3. Health Promotion Diagnosis
A clinical judgment concerning motivation and desire to improve well-being is known as a health promotion diagnosis, also known as wellness diagnosis.
The transition of an individual, family, or community from a certain level of wellness to a higher level of wellness is the focus of health promotion diagnosis. The diagnostic label or a one-part statement is usually the only component of a health promotion diagnosis. The following are some examples of health promotion diagnoses:
- Readiness for Enhanced Spiritual Well-being
- Readiness for Enhanced Self-care
- Readiness for Enhanced Parenting
- Readiness for Enhanced Participation in Daily Activities
- Readiness for Enhanced Sleeping Pattern

4. Syndrome Diagnosis
A syndrome diagnosis is a clinical decision made in response to a cluster of problems or risk nursing diagnoses that are expected to manifest due to a certain condition or incident.
Syndrome diagnoses are also written as a one-part statement requiring only the diagnostic label. The following are some examples of syndrome nursing diagnoses:
- Chronic Pain Syndrome
- Post-trauma Syndrome
- Frail Elderly Syndrome
- Decreased Cardiac output
- Ineffective cerebral tissue perfusion
Possible Nursing Diagnosis
Actual, danger, health promotion, and syndrome are all types of nursing diagnoses, but a possible nursing diagnosis is not one of them.
Possible nursing diagnoses are statements that describe a suspected condition that requires additional information to confirm or rule out.
It allows the nurse to inform other nurses that a condition may be present, but that additional data collection is needed to rule out or confirm the diagnosis. Here are several examples:
- Possible Chronic Low Self-Esteem
- Possible Social Isolation
- Possible Nutritional Imbalance
Components of Nursing Diagnosis
A nursing diagnosis usually consists of three parts: (1) the problem and its definition, (2) the etiology, and (3) the defining characteristics or risk factors (for risk diagnosis).
- Problem and Definition
The problem statement, also known as the diagnostic label, is a brief description of the client’s health problem or response for which nursing care is provided. A diagnostic label normally consists of two parts: a qualifier and the focus of the diagnosis. Qualifiers (also known as modifiers) are words added to some diagnostic labels to give additional meaning, limit, or specify the diagnostic statement. One-word nursing diagnoses (e.g., Anxiety, Constipation, Diarrhea, Nausea, etc.) are exempt from this rule because their qualifier and focus are inherent in the one term.
The etiology, or related factors, component of a nursing diagnosis label identifies one or more probable causes of the health problem, the conditions involved in the problem’s development directs the required nursing therapy, and allows the nurse to personalize the patient’s care. In order to eliminate the underlying cause of the nursing diagnosis, nursing interventions should be directed at etiological factors. With the term “related to,” etiology is linked to the problem statement, such as
- Decreased activity tolerance related to generalized weakness.
- Decreased physical mobility related to imposed bed rest.
- Impaired urinary elimination related to acute pain.
- Altered mentation related to delirium .
- Risk Factors
For risk nursing diagnosis, risk factors are used instead of etiological factors. Risk factors are forces that put an individual (or group) at an increased vulnerability to an unhealthy condition. Risk factors are normally written before the phrase “as evidenced by” in the diagnostic statement.
- Risk for Falls as evidenced by problems in gait and balance.
- Risk for Infection as evidenced by a break in skin integrity .
- Risk for dehydration as evidenced by poor skin turgor.
- Risk for Injury related to altered mobility.
- Risk for aspiration related to increased mucus production.
- Defining Characteristics
The clusters of signs and symptoms that indicate the presence of a specific diagnostic label are known as defining characteristics. The identified signs and symptoms of the patient are the defining characteristics in actual nursing diagnoses. Because no signs or symptoms are apparent in a risk nursing diagnosis, the factors that make the client more susceptible to the problem create the etiology of the problem. Defining characteristics are written following the phrase “as evidenced by” or “as manifested by” in the diagnostic statement.
Diagnostic Process: How to Diagnose
The diagnostic process is divided into three phases: (1) data analysis, (2) identification of the client’s health problems, risks, and strengths, and (3) formulation of diagnostic statements.
- Analyzing Data
Comparing patient data to standards, clustering cues, and identifying gaps and inconsistencies are all part of analyzing data.
- Identifying Health Problems, Risks, and Strengths
Following data analysis, the nurse and the client identify problems that support tentative actual, risk, and possible diagnoses in this decision-making process. It entails identifying whether a problem is a nursing diagnosis, a medical diagnostic, or a collaborative problem. This is also the stage in which the nurse and the client determine the client’s strengths, resources, and coping abilities.
- Formulating Diagnostic Statements
The last part of the diagnostic process is the formulation of diagnostic statements, in which the nurse develops a diagnostic statement through a process. The process is listed below,
How to Write a Nursing Diagnosis
When writing nursing diagnostic statements , describe an individual’s health status and the factors that have contributed to that status. It is not necessary to provide all diagnostic indicators. The format of diagnostic statements varies depending on the type of nursing diagnosis.
The PES format, which stands for Problem (diagnostic label), Etiology (related factors), and Signs/Symptoms (defining characteristics), is another approach to writing nursing diagnostic statements . Diagnostic statements in the PES format might be one-part, two-part, or three-part statements.
- One-Part Nursing Diagnosis Statement . Health promotion nursing diagnoses are frequently written as one-part statements since related factors are always the same: inspired to reach a greater level of wellness through related factors may be used to enhance the chosen diagnosis. There are no related factors on syndrome diagnoses. The following are some examples of one-part nursing diagnosis statements:
- Readiness for enhanced parenting
- Readiness for enhanced coping
- Two-Part Nursing Diagnosis Statement . The first component of risk or possible nursing diagnosis is the diagnostic label, and the second part is the validation for a risk nursing diagnosis or the presence of risk factors. Because signs and symptoms do not present, a third part for risk or possible diagnoses is not possible. The following are some examples of two-part nursing diagnosis statements:
- Risk for Infection as evidenced by compromised host defenses
- Risk for Ineffective tissue perfusion as evidenced by abnormal blood profile
- Possible Self Isolation related to unknown etiology
- Three-Part Nursing Diagnosis Statement. A three-part statement makes up an actual or problem-focused nursing diagnosis: diagnostic label, contributing factor (“related to”), and signs and symptoms (“as evidenced by” or “as manifested by”). The three-part nursing diagnosis statement is also known as the PES format that contains the Problem, Etiology, and Signs and Symptoms. The following are some examples of three-part nursing diagnosis statements:
- Impaired Physical Mobility related to decreased muscle control as evidenced by difficulty to move lower extremities.
- Acute Pain related to tissue ischemia as evidenced by statement of “I feel severe pain on my head!”
Variations on Basic Statement Formats
Variations in writing basic nursing diagnosis statement formats include the following:
- To make the diagnostic statement more descriptive and informative, use “secondary to” to break the etiology into two parts. A pathophysiologic or disease process, or a medical diagnosis, commonly follows the “secondary to.”
Example: Risk for Decreased Cardiac Output related to reduced preload secondary to myocardial infarction
- When there are too many etiologic factors or when they are too complex to explain in a single statement, the phrase “complex factors” is used.
Example: Chronic Imbalanced Nutrition: Less than body requirements related to complex factors.
- When the defining characteristics are present but the nurse is unsure of the cause or contributing factors, “unknown etiology” is used.
Examples: Ineffective Coping related to unknown etiology
Situational Low Self Esteem related to unknown etiology
- Specify a second part of the general response or NANDA label to make it more particular. Example: Impaired Skin Integrity (right side of the chest) related to damage of skin surface secondary to burn injury.
List of Nursing Diagnosis Examples
- Activity Intolerance Nursing Diagnosis
- Acute Pain Nursing Diagnosis
- Altered Mental Status Nursing Diagnosis
- Anemia Nursing Diagnosis
- Ankylosing Spondylitis Nursing Diagnosis
- Antisocial Nursing Diagnosis
- Anxiety Nursing Diagnosis
- Asthma Nursing Diagnosis
- Bell’s Palsy Nursing Diagnosis
- CHF Nursing Diagnosis
- Chronic Pain Nursing Diagnosis
- Constipation Nursing Diagnosis
- COPD Nursing Diagnosis
- Cytomegalovirus CMV Nursing Diagnosis
- Deficient Knowledge
- Dehydration Nursing Diagnosis
- Dentition Impaired Nursing Diagnosis
- Depression Nursing Diagnosis
- Diabetes Nursing Diagnosis
- E. Coli Nursing Diagnosis
- Electrolyte Imbalance Nursing Diagnosis
- Excess Fluid Volume Nursing Diagnosis
- Fluid Volume Excess Nursing Diagnosis
- GI Bleed Nursing Diagnosis
- HF Nursing Diagnosis
- Hodgkin’s Lymphoma Nursing Diagnosis
- Hypertension Nursing Diagnosis
- Imbalanced Nutrition Less than Body Requirements
- Imbalanced Nutrition More than Body Requirements
- Impaired Dentition
- Impaired Gas Exchange
- Impaired Physical Mobility
- Impaired Skin Integrity
- ineffective breathing pattern nursing diagnosis
- Ineffective Coping
Access all of our Nursing Diagnosis here or just type what you are looking for in the search bar.
Nursing references.
Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnoses handbook: An evidence-based guide to planning care . St. Louis, MO: Elsevier. Buy on Amazon
Gulanick, M., & Myers, J. L. (2022). Nursing care plans: Diagnoses, interventions, & outcomes . St. Louis, MO: Elsevier. Buy on Amazon
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2018). Medical-surgical nursing: Concepts for interprofessional collaborative care . St. Louis, MO: Elsevier. Buy on Amazon
Silvestri, L. A. (2020). Saunders comprehensive review for the NCLEX-RN examination . St. Louis, MO: Elsevier. Buy on Amazon
Anna Curran. RN, BSN, PHN
Leave a Comment Cancel reply
Lecturio Nursing
Cheat Sheets
Nursing Knowledge
Nursing Diagnosis: Examples & How To
RELATED STUDY SHEET
How to develop a nursing diagnosis using the nursing process
Table of contents, what is a nursing diagnosis .
A nursing diagnosis is a clinical judgment and a statement about a patient’s response to actual or potential health conditions or needs. It serves as the basis for selecting nursing interventions and making appropriate clinical decisions.
Making nursing diagnoses is the second step of the 5-step nursing process (ADPIE):
- Assessment
- Implementation
- Evaluation
In this step, the nurse actually identifies their client’s problems and names them according to nursing diagnoses.
Nursing diagnosis vs medical diagnosis
Medical diagnoses are made by physicians and identify a specific disease that a patient has.
Nursing diagnoses, on the other hand, focus on the patient’s response to that disease or condition , guiding individualized care plans. Nursing diagnoses are standardized and often use frameworks like NANDA-I (North American Nursing Diagnosis Association International) for consistent terminology and categorization.
How to write a nursing diagnosis
The goals of making nursing diagnoses are:
- Provide a concise definition of the patient’s response to a health condition
- Allows nurses to communicate in a common language
- Enables nurses to analyze assessment data
How to make nursing diagnoses:
- Activate critical reasoning skills.
- Observe for bodily changes.
- Determine strengths and unmet needs.
- Identify health risks.
- Cluster assessment data and match them with the NANDA nursing diagnoses.
What is the NANDA?
The NANDA-I (North American Nursing Diagnosis Association International) diagnostic manual is a compilation/list of nursing diagnoses originally recognized in 1973, with continued growth through nursing research.
Nursing diagnosis examples
Assessment data: Client has difficulty breathing when walking short distances and is wringing their hands during interaction.
Nursing diagnosis:
- Activity intolerance
Assessment data: Client has alteration in fluid volume due to dehydration, anemia, neurological impairment, and impaired memory related to dehydration.
Fitting official NANDA nursing diagnoses for this assessment include Fluid volume deficit and impaired memory.
Nursing diagnosis practice questions
Which nursing diagnosis would best apply to a child with allergic rhinitis .
A child with allergic rhinitis will experience increased mucus production, nasal congestion, and postnasal drip. These symptoms can lead to the child having difficulty maintaining a clear airway, which is correctly diagnosed with the nursing diagnosis of ineffective airway clearance.
Which nursing diagnosis would best apply to a child with rheumatic fever?
A child with rheumatic fever likely will experience joint pain and inflammation. Relevant nursing diagnoses would include acute pain related to inflammation and swelling , plus potentially impaired mobility and others.
Which condition is most likely to have a nursing diagnosis of fluid volume deficit?
The condition most likely to have a nursing diagnosis of fluid volume deficit is dehydration . Other conditions that may warrant this diagnosis include severe burns, hemorrhage, or conditions that cause polyuria like uncontrolled diabetes.
Why would a nursing diagnosis of a cough be incorrect?
A nursing diagnosis of “a cough” would be incorrect because a cough is a symptom, not a nursing diagnosis. Potential correct nursing diagnoses in a client suffering from a cough could be ineffective airway clearance, impaired gas exchange , or others depending on the assessment.
RELATED TOPIC:
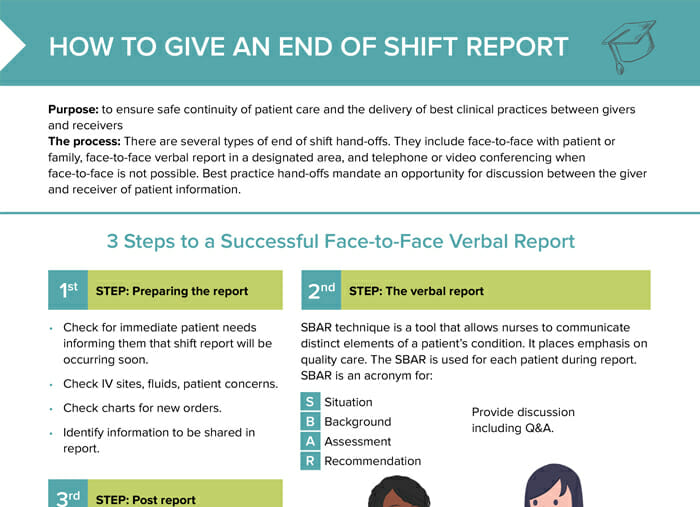
Nursing Shift Report (Template)
FREE CHEAT SHEET
Free Download
Nursing Cheat Sheet
Master the topic with a unique study combination of a concise summary paired with video lectures.
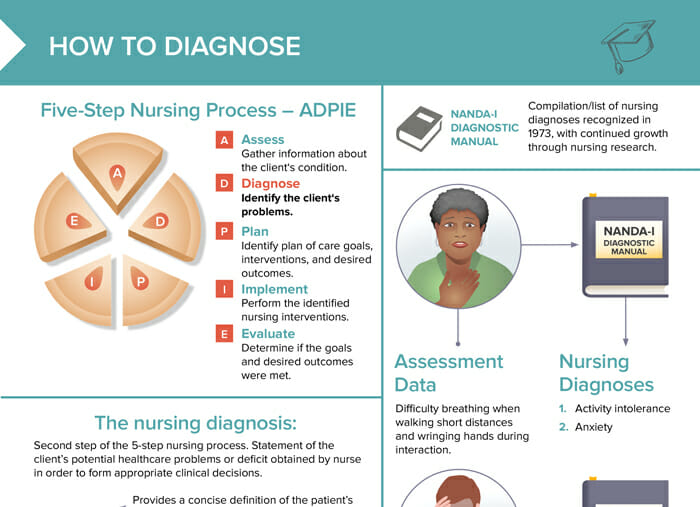
- Data Privacy
- Terms and Conditions
- Legal Information
USMLE™ is a joint program of the Federation of State Medical Boards (FSMB®) and National Board of Medical Examiners (NBME®). MCAT is a registered trademark of the Association of American Medical Colleges (AAMC). NCLEX®, NCLEX-RN®, and NCLEX-PN® are registered trademarks of the National Council of State Boards of Nursing, Inc (NCSBN®). None of the trademark holders are endorsed by nor affiliated with Lecturio.
Create a Free Account to Download
Your free account gives you access to:
- Extensive video library covering all nursing school topics
- 300+ Nursing cheat hseets incl. downloadable PDFs
- Smart exam prep tools
User Reviews

Nursing Diagnosis Guide: Everything You Need to Know
For many of us, a nursing diagnosis can sound like a strange concept. Signs and symptoms from our patients frequently lead to a medical diagnosis from a practitioner who specializes in disease. So we may be used to labels such as pneumonia or hepatitis. Not impaired gas exchange or risk for impaired liver function. So how then do we go from “patient can’t breath” to impaired gas exchange anyway? In this article, we will guide you on writing a nursing diagnosis, show examples of nursing diagnosis, types of nursing diagnosis and common nursing diagnosis that you may come across in your practice. So let’s get started!
What is a Nursing Diagnosis?

A nursing diagnosis is when a healthcare provider makes a judgment about how a person or a group of people respond to health issues or life events, or how likely they are to respond in a certain way. This diagnosis helps guide the selection of nursing actions to reach specific goals for which the nurse is responsible. Nursing diagnoses stem from data collected during assessments and help nurses plan care.
Through NANDA International, definitions and classifications guide these diagnoses and are approved and reviewed by the NANDA International (NANDA-I) Diagnosis Development Committee (DDC). So NANDA guides the diagnosis, and the diagnosis guides the nursing care.
In other words, the nursing diagnosis is a fundamental component of the nursing process. Mastering this process is crucial in nursing education, essential for exams and clinical practice alike, and will remain a guiding principle throughout your nursing career. Master the nursing process with the ADPIE mnemonic and use Picmonic to help you ace the topic .
Simply put, in order to determine an appropriate nursing diagnosis, a thorough and accurate nursing assessment is required. This ensures we have gained a clear picture of the patients physical, emotional and social needs. From here we can properly address any health concerns that may require attention and management by a physician and prioritize this care.
What does NANDA stand for?
NANDA was used as an acronym for the North American Nursing Diagnosis Association prior to 2002. After this time, NANDA became NANDA international and dropped its use as an acronym, but retained its name due to its familiarity. So the accurate name of this organization is NANDA International or NANDA-I. NANDA’s intent is to give nurses a platform that allows for communication and sharing of ideas to enhance understanding. Lets face it, nurses make professional judgments every day that help guide diagnosis and improve patient outcomes. Nursing diagnosis then allows us to pass on this knowledge to our patients and colleagues to ensure quality care is implemented.
What are the most common nursing diagnoses?
A nursing diagnosis is a conclusion that a nurse can determine independently without the need for input from an advanced medical provider and differs from a medical diagnosis. More on that later. Common nursing diagnoses may include activity intolerance, acute confusion, anxiety, pain, risk of infection, constipation, and impaired skin integrity. To name a few. So clinical judgment about how our patients are responding to health issues or life events allows nurses to provide nursing interventions that lead to outcomes to which the nurse is responsible.
Purpose of a Nursing Diagnosis
As mentioned above, the purpose of the nursing diagnosis is to determine the response the patient is having to health issues or life events, and then develop a plan of care to support them. A proper plan of care addresses important aspects such as available resources and nursing interventions to be implemented. In addition, it serves as a foundation for communication, provides a patients baseline and fine-tunes problem-solving and critical thinking skills for new and seasoned nurses.
The intent then, is to promote high quality care and improved patient outcomes. Quality care, documentation and clear communication ultimately improves clinical practice. Important insights are conveyed to other members of the care team when team communication is improved, which ultimately benefits everyone.
Nursing Diagnosis vs. Medical Diagnosis

A medical diagnosis focuses on the medical problem and its presenting symptoms and is performed by the physician or advanced healthcare practitioner. So our patient who can’t breathe may be assessed by a physician or nurse practitioner and given the medical diagnosis of chronic bronchitis or pneumonia . The nurse then implements any prescribed treatments and therapies and observes the patient’s response to those. Important to note, that while nursing diagnoses can evolve over time, medical diagnoses typically remain permanently recorded in the patient’s medical history.
A nursing diagnosis then, focuses on the care to be delivered based on how the patient is responding or reacting to a health condition. The collected patient data of difficulty breathing due to chronic bronchitis, directs the choice of nursing actions to achieve particular objectives for which the nurse is accountable. Nursing diagnoses stem from data collected during assessments and aid nurses in developing care plans.
Nursing Diagnosis Classification
Nursing diagnosis classification helps nurses to organize and categorize health issues, in addition to identifying risks, and strengths in patients. They are split into three levels: domains, classes, and nursing diagnoses. Within each domain, there are typically three to six classes of nursing diagnoses, which are further subdivided into individual diagnoses.

For more thorough and updated information regarding the domains, classes and nursing diagnosis, be sure to check out the latest edition of NANDA International- Nursing Diagnoses Definitions and Classification , 13th Edition.
Types of Nursing Diagnosis
Now we move on from Nursing Diagnosis Classification to Types of Nursing Diagnosis. According to NANDA international, nursing diagnoses fall into four categories: problem-focused, risk, health promotion, and syndrome diagnoses.
Problem-Focused
A problem-focused diagnosis identifies the patient’s actual or current issue as observed during the nursing assessment. Indicators such as a productive cough or inability to breathe help us to formulate our nursing diagnosis. It relies on the signs and symptoms noted during this evaluation, and how the patient is responding to a health issue. Problem-focused nursing diagnoses are the most common and usually easy to spot as they have three components to them. (1) nursing diagnosis, (2) related factors, and (3) defining characteristics. Lets use our above example of our patient who can’t breathe and was diagnosed with chronic bronchitis by the physician. We also determined that their 02 saturations were 88% with 2L oxygen via nasal cannula.
Example: (1) Impaired gas exchange related to (2) chronic bronchitis as evidenced by (3) O2 saturation level of 88% on 2L oxygen via nasal cannula.
This diagnosis identifies the actions required to reduce the risk associated with a patient’s health issue. Therefore, a problem does not yet exist, but based on clinical judgment, one may develop unless the nurse takes action. The difference with this one is there are no etiological factors as they have not yet occurred. For example, the patient with chronic bronchitis is not yet dehydrated, but is at risk for this happening. Components of a risk nursing diagnosis include (1) risk diagnostic label, and (2) risk factors.
Example: (1) risk for (2) dehydration and drying of mucus secretions
Health Promotion
Health promotion diagnosis is a judgment on how ready or motivated an individual, family or community is to improve their health outcomes. The purpose being to improve patient/population health and well-being. These types of diagnosis generally include just the diagnostic label or a one-part statement. With our above patient we have determined that they understand and are willing to apply information required to follow their complex treatment plans.
Example: readiness for enhanced health literacy
Syndrome diagnoses are clinical judgments about a group of nursing diagnoses that happen together and require similar treatments. For example, when a patient is experiencing multiple health problems that form a pattern. So here, one or more nursing diagnoses are used as defining characteristics. To add clarity, related factors can be used but are not required. So let’s say our patient who has been diagnosed with chronic bronchitis is also experiencing dehydration and hypoventilation. They may be given the following syndrome diagnosis.
Example: Ineffective peripheral tissue perfusion
What Are the Components of a Nursing Diagnosis?
A nursing diagnosis typically consists of three components that follow a specific template recommended by NANDA International. The problem statement, the etiology/related factors, and defining characteristics/risk factors. These are written in a problem/etiology/related factors (PES) framework.
(1) problem statement
(2) etiology/related factors
(3) defining characteristics/risk factors
The Problem Statement
The problem statement describes what the patient’s current health problem is and any nursing interventions that may be required. This can also be referred to as the diagnostic label. Let’s use the example for a problem-focused diagnosis that we indicated above and break it down into the problem statement.
The problem statement: (1) Impaired gas exchange
The etiology, or related factors, pinpoint likely causes of the health issue and any contributing conditions. This provides guidance for any necessary nursing interventions or therapy that may be required.
The Etiology: related to (2) chronic bronchitis
Defining Characteristics or Risk factors
Defining Characteristics or risk factors are signs and symptoms the patient is exhibiting that are causing a problem right now or may cause them to be vulnerable towards a health problem later on down the road. Ensure you are using “as evidenced by” to support your diagnostic label.
Defining Characteristics or Risk factors: as evidenced by (3) O2 saturation level of 88% on 2L oxygen via nasal cannula.
Writing a Nursing Diagnosis
Now that we have defined the types of nursing diagnosis and their components, let’s put this into practice with some other examples.

How to Write a NANDA Nursing Diagnosis
Remember, in order to develop a nursing diagnosis, we need the components from our clinical assessment that we have determined may actually or potentially cause the patient health risks. With this information we then plug this data into a PES framework as specified by NANDA International. We will focus on the most common type of nursing diagnosis, the problem diagnosis, which means we are looking for the following three components.
- Problem Statement
- Etiology/related factors
- Defining characteristics/risk factors
How to Write a Good Nursing Diagnosis
Problem-focused diagnosis formula.
To write this type of nursing diagnosis, use the PES format as we mentioned above. Start with what the patient is experiencing. For this example, we have a patient who has been diagnosed with chronic kidney disease by the physician, with little to no urine output and demonstrating signs of edema. (1) urinary retention followed by the etiologic factors (related factors in an actual diagnosis) (2) chronic kidney disease, then identify the signs and symptoms that the patient is exhibiting. (3) urinary output less than 400 ml per day or less than 20 ml per hour. Plug this data into PES below.
(Problem-Focused Diagnosis) related to________(Related Factors) as evidenced by _____________ (Defining Characteristics).
Example: Impaired urinary retention related to chronic kidney disease as evidenced by urinary output less than 400 ml per day or less than 20 ml per hour.
Risk Diagnosis Formula
This one is a bit more straightforward, as there are no related factors, just a potential problem. However, now we will need to use our critical thinking skills to see how this one plays out. So with our patient above, as kidney function declines, we may start to see peripheral and pulmonary edema, and hypertension due to sodium retention. This may lead to a reduction in cardiac output to enhance kidney perfusion. Plug in this data below.
Risk for_____as evidenced by_____(Risk Factors).
Example: risk for decreased cardiac output as evidenced by fluid imbalance affecting circulating volume and myocardial workload.
So, If you think of a nursing diagnosis as a template or framework, then you know what to look for and be best prepared to assess your patient.
Be sure to check out the Picmonic on how to write a nursing diagnosis and follow along to master this important nursing skill.
And be sure to check out more content to master nursing school and remember more in less time with nursing mnemonics .
About the Author
Pamela Schutz, RPN, Medical-Nursing Scholar
As a registered psychiatric nurse with over 23 years of experience, in addition to coordinating events, managing social media platforms, and crafting compelling content, Pamela effectively conveys messages and drives participation. Pamela has the talent for simplifying complex ideas and making the captivating world of medicine less mysterious.
You may also like
- How to Remember Antibiotic Endings

- The Hardest Nursing Classes: Tips for Success

How to Become a Licensed Practical Nurse (LPN)
Recent posts.
- Common Suffixes in Medical Terminology
- How to Study Pharmacy: 7 Top Tips for Students
- How to Study Effectively in PA School

Remember more in less time and boost your test scores with Picmonic, the world’s best visual mnemonic learning resource and study aid for medical school, nursing school, and more!

Company Information
- Picmonic Shop
- Creator Community
Get Picmonic and start your journey now.

- Pre-Nursing
- Nursing School
- After Graduation
Nursing Diagnosis: A Complete Guide for Students & Professionals

- Over 125 Years of Healthcare Expertise: 125+ years of combined healthcare experience with a focus in nursing education.
- Exceptional User Satisfaction: 4.9/5 average rating from 3,500+ reviews across TrustPilot , WorthePenny , Better Business Bureau, and other trusted review sites.
- Proven Success: Over 1 million nurses served since 2012 with a 99% NCLEX pass rate ( 2024 NCLEX average pass rate = 79%).
- Team Composition: Staff includes RNs, MSNs, DHSs, nursing professors, and current/former NCLEX question writers.
Jump to Sections
What is one of the most essential tools in a nurse’s toolkit?
If you answered a stethoscope or a blood pressure cuff, you’re right. But another important tool is the foundation of quality client care — the nursing diagnosis.
In this comprehensive guide, we’ll explore everything you need to know about nursing diagnoses, including their purpose, process, and how to write one effectively.
What is a Nursing Diagnosis?
A nursing diagnosis is a clinical judgment a nurse makes to identify client problems and their causes.
It serves as the basis for planning interventions and evaluating client outcomes.
Unlike medical diagnoses, which focus on identifying diseases, nursing diagnoses focus on:
- The client’s response to the illness
- The associated symptoms
- How the symptoms affect the client’s daily lives
For example, while a medical diagnosis might identify pneumonia, a nursing diagnosis might focus on the client’s ineffective airway clearance due to the disease. A nursing diagnosis allows nurses to create a nursing care plan (NCP) to guide how they care for the client.
NANDA International (NANDA-I) provides a comprehensive list of standardized nursing diagnoses to ensure consistency and accuracy globally. NANDA-I continuously updates its guidelines to reflect the latest in nursing knowledge, making it easier for nurses to deliver high-quality care.
The standards date back to the 1950s, and about 20 years later, NANDA-I held its first national conference to classify nursing diagnoses.
The organization continues to host these meetings to keep the definitions of diagnoses current. Nurses can also submit new diagnoses to the organization for review.

Purpose of Nursing Diagnosis
The primary purpose of nursing diagnosis is to provide a framework for identifying and addressing the client’s health needs to improve client outcomes.
It provides a holistic view of the client by considering physical, emotional, social, and environmental factors.
Here’s why nursing diagnoses matter:
- Identification of client needs : Nursing diagnoses help nurses identify the most critical issues affecting a client’s health. By systematically assessing the client, nurses can determine the most pressing concerns, such as pain, risk of infection, or anxiety.
- Early detection and intervention : Early identification of potential health problems allows for timely interventions , preventing complications and improving client outcomes. For example, identifying the risk for falls early on can lead to preventive measures that keep the client safe.
Guidance in developing care plans : Nursing diagnoses are integral in creating effective NCPs. They provide a clear framework for the interventions needed and the expected outcomes. This ensures that care is efficient and effective, meeting the client’s needs.
Get Your Free Care Template Today

Nursing Diagnosis within the Nursing Process
The nursing process is a systematic, client-centered method nurses use to ensure quality care.
It consists of five steps: assessment, diagnosis, planning, implementation, and evaluation (often referred to as ADPIE ).
- Assessment : Gather comprehensive information about the client’s physical, psychological, sociocultural, and spiritual needs.
- Diagnosis : Use the data gathered during the assessment to identify the client’s problems.
- Planning : Set measurable, achievable short- and long-term goals for the client, then identify appropriate nursing interventions.
- Implementation : Carry out the planned interventions.
- Evaluation : Assess the effectiveness of the interventions and adjust the care plan as necessary.
For example, a nurse might note a client experiencing shortness of breath during the assessment phase. Based on this assessment, the nurse might diagnose the client with an ineffective breathing pattern (IBP) , a common nursing diagnosis.
This diagnosis will guide the care plan, which might include interventions such as oxygen therapy and teaching the client breathing exercises. The nurse will then evaluate the effectiveness of these interventions and adjust as needed to improve the client’s breathing pattern.
Nursing diagnoses are essential to the nursing process because they provide a framework for identifying and addressing the client’s needs. They also allow nurses to communicate effectively with other health care professionals, ensuring all team members work towards common goals.
Common Nursing Diagnoses
Below is a common nursing diagnosis list with brief descriptions of how nurses might apply diagnoses in different settings.
- Acute pain : This diagnosis applies to clients experiencing pain that has a sudden onset, typically associated with injury, surgery, or a medical condition. Nurses assess the severity and cause of the pain and implement interventions such as administering pain medication or teaching relaxation techniques.
- Impaired gas exchange : This diagnosis applies to clients with a decreased ability to oxygenate and eliminate carbon dioxide. Nurses monitor respiratory status, administer oxygen therapy as needed, and educate the client on breathing techniques.
- Activity intolerance : An activity intolerance diagnosis applies to clients who have difficulty moving or performing activities of daily living independently. This may arise because of a medical condition or injury. Nurses assess the client’s level of mobility and implement interventions such as range-of-motion exercises, ambulation assistance, or assistive devices.
- Ineffective airway clearance: This diagnosis applies to clients with an obstruction that hinders airflow in the respiratory tract. Nurses assess for signs and symptoms such as coughing, wheezing, or shortness of breath. They then implement interventions such as suctioning, deep breathing exercises, and chest physiotherapy.
- Impaired skin integrity : This diagnosis is for clients with conditions that affect the skin, such as pressure ulcers, surgical wounds, or burns. Nurses would then focus on wound care, repositioning the client regularly, and using moisture barriers to protect the skin.
- Anxiety : This diagnosis is for clients experiencing excessive worry, fear, or nervousness, often related to a medical condition or hospitalization. Interventions may include providing emotional support, teaching relaxation techniques, or referring the client to a counselor.

How to Write a Nursing Diagnosis
Writing a nursing diagnosis involves a systematic approach to ensure clarity and accuracy.
The PES format is widely used in nursing and stands for Problem, Etiology, and Symptoms.
- Problem (P) : Give a problem statement, also known as the diagnostic label, articulating the client’s condition. It might include modifiers or qualifiers that provide additional information about the diagnosis. You’ll also have a focus that explains the diagnosis’ center point.
- Etiology (E) : This refers to the cause or contributing factors of the problem. It’s linked to the problem using the phrase “related to.” For example, “related to immobility” or “related to surgical incision.”
- Symptoms (S) : These are the signs and symptoms the nurse identified during the assessment, providing evidence for the nursing diagnosis. They’re linked to the etiology using the phrase “as evidenced by.” For example, “as evidenced by redness and swelling at the incision site” or “as evidenced by a pain rating of 8/10.”
Correctly written nursing diagnosis example :
- Acute pain related to a surgical incision as evidenced by a pain rating of 8/10 and guarding behavior.
Incorrectly written nursing diagnosis example :
- Pain due to surgery.
The incorrect example is vague and lacks the structure to create an effective care plan. It doesn’t follow the PES format or provide clear evidence to support the diagnosis.
NANDA-I Nursing Diagnosis: 4 Types
There are four main categories of nursing diagnoses.
- Problem-Focused
A problem-focused diagnosis revolves around the symptoms and signs that the client presents with.
This category comprises the largest proportion of nursing diagnoses. The diagnosis in this situation aims to identify the client’s central problem.
The problem-focused diagnosis includes three main parts:
- The nursing diagnosis itself
- Any related factors
- Any defining characteristics
Nurses use risk nursing diagnoses to determine the interventions needed to prevent certain medical conditions or other problems from developing.
Nurses must use their training and experience to help them see the risks that will impact the client.
A risk nursing diagnosis will include:
- The nursing diagnosis
- Any risk factors
- Health Promotion
A nurse uses this diagnosis to help improve the client’s health.
These diagnoses take a holistic look at the client treated and determine how interventions can help them improve their condition globally. These diagnoses help to promote self-care.
A health promotion diagnosis will include:
However, a nurse can complete the health promotion diagnosis with just a diagnostic label.
A syndrome diagnosis looks for patterns or clusters of nursing diagnoses that all call for related interventions.
For example, a nurse might note that an older adult meets the requirements for frail elderly syndrome. This syndrome requires related interventions that are all targeted at helping the client improve their quality of life while remaining protected from common risks and ailments that come with advanced aging.
A syndrome diagnosis requires only the diagnostic label component.
6 Tips for Writing a Nursing Diagnosis
- Use clear and specific terms to describe the PES.
- Avoid using medical jargon or abbreviations.
- Refer to evidence-based resources such as NANDA-I or your institution’s standardized nursing language.
- Collaborate with the client to verify accuracy and gather additional information.
- Continuously reassess and revise the nursing diagnosis as the client’s condition changes.
- Seek guidance from experienced nurses or use tools such as concept maps or care plans to develop a comprehensive and individualized nursing diagnosis.
Nursing Diagnoses and Care Plans
Nursing diagnoses are the foundation upon which nurses build NCPs.
They provide the basis for:
- Setting goals
- Selecting interventions
- Evaluating outcomes
A well-formulated care plan ensures targeted, effective interventions and better health outcomes.
For example, if a nurse diagnoses a client with a “knowledge deficit” about administering medication, the care plan should include education on drug safety and correct administration techniques. By addressing this problem directly, the nurse can improve client understanding and decrease medication errors.
Effective nursing diagnoses also involve collaboration with clients. Clients often have valuable insight into their health and can provide information to help accurately identify problems.
By involving clients in the process, nurses promote autonomy and encourage active participation in their care. Additionally, collaborating with clients helps build trust between the nurse and client, leading to better communication.
Sample Care Plan Including Nursing Diagnoses
In this sample care plan, the nursing diagnosis of “risk for injury” directly addresses the identified problem and sets specific goals or interventions to decrease the risk of falls.
- Diagnosis : Risk for injury related to unsteady gait and decreased muscle strength secondary to Parkinson’s disease.
- Goals : Client will maintain safety during daily activities.
- Educate client on proper use of assistive devices, such as a walker or cane.
- Ensure clear pathways and remove any potential tripping hazards in the home environment.
- Assist client with transfers and ambulation as needed.
- Evaluation : After two weeks, the client has not experienced any falls or injuries, demonstrating improved safety during daily activities.
Interventions Based on Nursing Diagnoses
Selecting appropriate interventions is critical to addressing the issues identified in the nursing diagnosis.
Tailor interventions to the client’s unique needs and circumstances. This will ensure the most effective and individualized care plan.
Interventions can include independent nursing and collaborative actions with other health care professionals.
For example, in the case of a client with diabetes who is at risk for infection due to poor wound healing, an independent intervention is educating the client on proper wound care and hygiene. A collaborative intervention could involve consulting with a wound care specialist or dietitian to develop a specialized diet plan to promote healing.
Nurses should also incorporate evidence-based practices and standards of care when selecting interventions, ensuring they’re rooted in current research and best practices. Here are more examples of interventions based on common nursing diagnoses.
Risk for surgical site infection
- Educate client and family on proper wound care techniques.
- Monitor the incision site and look for signs of infection, such as redness or drainage.
Impaired physical mobility
- Encourage regular range of motion exercises to maintain joint mobility.
- Collaborate with physical therapy to develop an exercise plan.
Deficient fluid volume
- Monitor fluid intake and output.
- Provide oral or IV fluids as prescribed.
Ineffective coping
- Encourage the client to express their concerns and feelings.
- Refer to counseling or support groups as needed.
Learn more about nursing interventions and what they are with SimpleNursing.
NANDA-I Nursing Diagnoses: Key Updates
Staying current with NANDA-I guidelines is essential for accurate nursing diagnosis and effective intervention selection.
Here are some key updates from the latest version of NANDA-I:
- Introduced 54 new diagnoses
- Revised 98 diagnoses
- Retired unilateral neglect (00123) due to a lack of research evidence to support diagnoses
- Retired “constipation” and “diarrhea,” which are now defining characteristics in a new diagnosis — impaired intestinal elimination (00344)
- Retired “decreased cardiac output” because it’s another name for a medical diagnosis instead of an independent nursing judgment
- Insomnia and sleep are now diagnostic indicators of an ineffective sleep pattern (00337)
- Revised nursing diagnosis definitions, including those related to risk diagnoses
- Standardized terminology for diagnostic indicators — associated conditions, at-risk populations, defining characteristics, related factors, and risk factors — to provide clarity
- Updated nursing diagnosis labels that align with current literature and accurately represent human responses
Keep Learning with SimpleNursing
Nursing diagnoses are an essential tool for providing high-quality client care.
They help nurses identify and address the most pressing health issues, guide the development of care plans, and ultimately improve client outcomes. To continue learning about nursing diagnoses, interventions, and other important topics in nursing, check out SimpleNursing’s nursing school resources .
Our platform offers a range of materials, including video lectures, quizzes, and study tools to help you succeed.
Join SimpleNursing today to enhance your nursing knowledge and provide the best possible care for clients.
Get FREE Stuff
Let us email you free weekly content to help you pass nursing school and the NCLEX
- Nursing school study guides
- Exclusive video access
- Exam practice questions
- Subscriber-only discounts
Share this post
Nursing students trust simplenursing.

SimpleNursing Student Testimonial
Most recent posts.

Depolarization vs Repolarization of the Heart
The human heart beats approximately 100,000 times a day to drive the circulation of blood…

Where to Find Pulse Points on Your Patients
In your daily practice as a nurse, you will complete client assessments. And one of…

Comparing LPNs vs CNAs: Duties, Education, and Career Insights
What do LPNs and CNAs have in common? They're part of the big bowl of…

How to Become a Legal Nurse Consultant
Have you ever watched a courtroom drama and imagined yourself as one of the experts…
Find what you are interested in
Education: Bachelor of Arts in Communications, University of Alabama


IMAGES
VIDEO
COMMENTS
Examples of this type of nursing diagnosis include: Decreased cardiac output Chronic functional constipation; Impaired gas exchange; Problem-focused nursing diagnoses are typically based on signs and symptoms present in the patient. They are the most common nursing diagnoses and the easiest to identify. 2. Risk nursing diagnosis
Syndrome diagnoses also have no related factors. Examples of one-part nursing diagnosis statements include: Readiness for enhanced coping; Rape Trauma Syndrome; Two-Part Nursing Diagnosis Statement. Risk and possible nursing diagnoses have two-part statements: the first part is the diagnostic label and the second is the validation for a risk ...
To clarify this distinction, here are two examples of how medical and nursing diagnoses can work together. Example 1: A patient with a medical diagnosis of cerebrovascular accident (stroke) may lead to the complementary nursing diagnosis of unilateral neglect. ... Like a problem-focused diagnosis, the risk-focused statement should also use a ...
Examples of Nursing Diagnoses; Health Promotion: Health Awareness: Sedentary lifestyle: Health Management: Frail elderly syndrome Ineffective health maintenance: Nutrition: ... According to NANDA recommendations, a nursing diagnosis is a statement that includes both the diagnosis itself and related factors seen through defining characteristics ...
One-Part Nursing Diagnosis Statement. Health promotion nursing diagnoses are usually written as one-part statements because related factors are always the same: motivated to achieve a higher level of wellness though related factors may be used to improve the of the chosen diagnosis. Syndrome diagnoses also have no related factors. Examples of ...
Nursing diagnosis is an essential component of nursing practice that helps nurses identify actual or potential health problems and formulate individualized care plans for their patients. Definition of Nursing Diagnosis. Nursing diagnosis is a clinical judgment made by nurses based on data collected during a patient assessment. It identifies ...
The three-part nursing diagnosis statement is also known as the PES format that contains the Problem, Etiology, and Signs and Symptoms. The following are some examples of three-part nursing diagnosis statements: Impaired Physical Mobility related to decreased muscle control as evidenced by difficulty to move lower extremities.
Learn what official nursing diagnoses are, how they differ from medical diagnoses, and practice with examples and practice questions ... A nursing diagnosis is a clinical judgment and a statement about a patient's response to actual or potential health conditions or needs. It serves as the basis for selecting nursing interventions and making ...
In this article, we will guide you on writing a nursing diagnosis, show examples of nursing diagnosis, types of nursing diagnosis and common nursing diagnosis that you may come across in your practice. So let's get started! ... These types of diagnosis generally include just the diagnostic label or a one-part statement. With our above patient ...
Nursing Diagnosis within the Nursing Process. The nursing process is a systematic, client-centered method nurses use to ensure quality care.. It consists of five steps: assessment, diagnosis, planning, implementation, and evaluation (often referred to as ADPIE).. Assessment: Gather comprehensive information about the client's physical, psychological, sociocultural, and spiritual needs.