What is Problem-Solving in Nursing? (With Examples, Importance, & Tips to Improve)
Whether you have been a nurse for many years or you are just beginning your nursing career, chances are, you know that problem-solving skills are essential to your success. With all the skills you are expected to develop and hone as a nurse, you may wonder, “Exactly what is problem solving in nursing?” or “Why is it so important?” In this article, I will share some insight into problem-solving in nursing from my experience as a nurse. I will also tell you why I believe problem-solving skills are important and share some tips on how to improve your problem-solving skills.

What Exactly Is Problem-Solving In Nursing?
5 reasons why problem-solving is important in nursing, reason #1: good problem-solving skills reflect effective clinical judgement and critical thinking skills, reason #2: improved patient outcomes, reason #3: problem-solving skills are essential for interdisciplinary collaboration, reason #4: problem-solving skills help promote preventative care measures, reason #5: fosters opportunities for improvement, 5 steps to effective problem-solving in nursing, step #1: gather information (assessment), step #2: identify the problem (diagnosis), step #3: collaborate with your team (planning), step #4: putting your plan into action (implementation), step #5: decide if your plan was effective (evaluation), what are the most common examples of problem-solving in nursing, example #1: what to do when a medication error occurs, how to solve:, example #2: delegating tasks when shifts are short-staffed, example #3: resolving conflicts between team members, example #4: dealing with communication barriers/lack of communication, example #5: lack of essential supplies, example #6: prioritizing care to facilitate time management, example #7: preventing ethical dilemmas from hindering patient care, example #8: finding ways to reduce risks to patient safety, bonus 7 tips to improve your problem-solving skills in nursing, tip #1: enhance your clinical knowledge by becoming a lifelong learner, tip #2: practice effective communication, tip #3: encourage creative thinking and team participation, tip #4: be open-minded, tip #5: utilize your critical thinking skills, tip #6: use evidence-based practices to guide decision-making, tip #7: set a good example for other nurses to follow, my final thoughts, list of sources used for this article.

30 Top Nursing Interview Questions & How to Answer Them
- Types of Interview Questions
- Question Themes
- How to Answer
- Common Interview Questions & Answers
Questions to Ask the Employer
Things to do before leaving the interview.
- Interview Prep

Wondering which nursing interview questions you might be asked at your next job interview? You've come to the right place. Read on for the top nursing interview questions and answers to help you nail that next interview.
Types of Nursing Interview Questions
Healthcare employers tend to lean towards asking behavioral-based interview questions.
Behavioral-based questions are about how you acted in a specific situation. The goal is to gauge how you react under different circumstances. It is best to answer these questions with real-life stories and examples.
Nursing Interview Question Themes
Most behavioral interview questions asked of nurses are based on the following themes:
- Patient-care
- Adaptability
- Time management
- Communication style
- Motivation and core values
How to Answer Behavioral-Based Questions
When telling stories during interviews, we suggest using the S-T-A-R format - this will ensure your story is direct, concise and to the point. So, what does the acronym S-T-A-R stand for?
A ction-steps
You can learn more about answering interview questions by using the S-T-A-R format by reading our complete guide to nursing interviews.
30 Common Nursing Interview Questions & Answers
- Teamwork questions
- Patient care questions
- Adaptability questions
- Time management questions
- Communication style questions
- Motivation and core values questions
Sample Nurse Interview Questions: Teamwork
Interviewers want to envision how you will fit in with their team and how you work well with various personalities. We suggest telling a story about a time you dealt with a co-worker who had a conflicting personality, a disagreement within your healthcare team, or a challenging patient case involving your team. Always remember to talk about what you learned from the situation and if anything positive came from it.
1. Describe a situation when you had to work closely with a difficult coworker. How did you handle the situation? Were you able to build a relationship with this person?
Never talk badly about anyone during an interview. Explain the situation and why the individual was difficult. Share how you handled the situation. Try to turn anything negative into a positive. What did you learn from the situation? What might you do differently now? What was the “silver lining”? Were you able to talk through your differences? Did you become friends?
Sample answer:
Working closely with difficult coworkers can be challenging, but it is important to remember the patient, their care, and their family is most important. Putting aside differences is essential for all nurses because not everyone is the same. Sometimes this means not discussing specific topics such as religion or politics at work. With that being said, not everyone will become friends in the workplace but working together is key for the successful care of patients.
2. Talk about a conflict within your healthcare team. What was the conflict, and how did you handle it?
Explain the conflict surrounding the situation. Who was involved? What was your role? Did anything positive come from this? What did you learn?
Conflict often occurs in the hospital setting, particularly between new nurses and more seasoned staff, as well as doctors and nurses. At one specific time, there was concern from a parent that a newer nurse was not monitoring a patient’s breathing postoperatively as closely as she would have liked.
I was covering the nurse for lunch and the mother brought her concerns to me. I discussed and validated her concerns. Once the nurse was back from lunch, I spoke with her regarding the mother’s concerns. The nurse was very upset and felt it was not my place to say anything to her regarding this. A parent or patient’s concerns should never be dismissed. I spoke to the nurse educator on the unit to use the opportunity as a teaching moment.
3. Describe a time when you were particularly proud of your healthcare team. What was your role in this situation?
Describe the circumstances and actions step-by-step. What happened to make you feel proud? What was your role? Who was involved? What was the result?
Working in the ICU setting, there are countless moments that make me proud to be a nurse and proud to be part of this amazing community. Watching a patient survive a code, take their first steps on prosthetic legs, or be in the room when a patient I tell is receiving a new heart is the moment we all want to be a part of. Even if I am not delivering the news or caring personally, the information my patient receives directly affects me.
4. Tell me about a time you stepped into a leadership role.
This doesn’t need to be anything official. Think about a time when you stepped up to the plate and took charge of a situation. What was the circumstance? What made you take the lead? Who was involved? Did any opportunities arise from this situation?
I have acted as a charge nurse numerous times in my career. I have had to lead code teams, respond to rapid responses, and make difficult staffing decisions. As a charge nurse I have determined patient assignments to ensure that assignments are fair and equal. Furthermore, I have to ensure that the nurses’ skill set is sufficient for the assignment.
Sample Nurse Interview Questions: Patient Care
Healthcare hiring professionals want to hire nurses who provide excellent patient care. Education is of utmost importance to healthcare employers. We suggest telling stories about times you provided top-notch patient care or went out of your way to educate patients and/or their families.
1. Tell me about a time when a patient’s family was dissatisfied with your care. How did you handle that situation?
Make sure to explain the situation in detail, including both perspectives (the patient’s family and yours). Never talk badly about patients or their families. Take ownership if you indeed did something wrong. Share any positives that came from this - what did you learn? What would you do differently now? How did you turn this into a positive?
I once was floated to a unit that I had never worked in and wasn’t sure where supplies were located. The patient's mother did not recognize me as a regular floor nurse on the unit, which already made the family leery of me from the start of the shift. I continually had to prove myself throughout the day because, as nurses, we all do things slightly differently.
There is not always a wrong way or a right way to do things but in this case, there was a policy to be followed. I followed it, and apparently, my dressing change was slightly different than the previous ones. I communicated regularly with the charge nurse, and she came to check in with the family to address any issues in real time.
2. What approach do you take in communicating with people who do not know medical jargon? Give an example of a time you explained medical terminology to someone who is not medically trained.
Explain step-by-step how you’ve performed in a similar situation. What specific words and terminology did you use? How did you know that the individual understood your explanation?
It is imperative that we use simple words for our patients and families who are not medically trained and utilize a teach-back method to ensure they understand the information that is communicated to them. I once had to explain post-operative care to a family whose child had tonsil surgery. I had to use words such as poop instead of bowel movement. I used Tylenol instead of acetaminophen.
3. Describe a time you provided effective patient or family education.
Tell a story about a time when you knew your patient or family retained your teachings. How did you know that you effectively communicated the piece of education?
After teaching families, I ask them to repeat the information in their own words. Using a teach-back method allows nurses to know if families truly understood the information that was given to them. It is also important to provide the family with written educational material and use other forms of education, such as videos or hands-on, when possible.
I taught a family post-operative spine care after a posterior spinal fusion. The parents were able to properly demonstrate how to transfer their child from the bed to the chair. In doing so, I was able to determine that they had retained the information.
4. Talk about a time a patient or their family was particularly pleased and appreciative of your care.
Tell a story about a family who was happy with your care. What did you do in particular that they were pleased with? How did you know they were happy? What were the results of this situation?
Working in pediatrics can be challenging but also very rewarding. There are times when parents are unable to stay at the bedside 24/7 because of work, other children, or previous commitments.
I was taking care of a 6-month-old twin during a specific shift. The family was unable to be at the bedside because the father had to work, and the mother was at home with the twin sister and the other children. I spent my shift playing with the infant with age-appropriate toys, and when the mother called to check in – I put the phone next to the infant. The mother was able to hear her baby laughing while singing to her. This brought them closer together and the mother to tears. She stated that no other nurse had done that during the hospitalization, and she was eternally grateful.
5. Give an example of a time you had to interact with a hostile patient. How did you handle the situation, and what was the outcome?
Tell a story about a hostile patient and your step-by-step actions. What was the patient doing that was hostile? How did you react? How did you feel? What procedures did you follow to interact with the patient? What was the result of your actions?
Unfortunately, hostile patients often are part of the job. It’s important to remember some of the patients are being hostile because they are in pain, away from family, and in the hospital setting.
T here was a time when a patient refused to take her medication. I tried everything, but she would spit them out at me when she tried to take them. Because of this behavior, I involved my charge nurse, the physician in charge of her care, and the social worker.
After many conversations and phone calls, it was determined the patient was spitting the medication out because she liked it mixed in chocolate pudding. The woman was elderly and suffered from dementia. It was only after speaking with the social worker that we learned of her medication preference. She was not able to communicate with us her wants and needs and this led to hostility.
6. Describe a time you were faced with a patient who chose not to communicate or disclose important information. How did you handle the situation, and what was the outcome?
Tell a story about a patient you worked with in a similar situation. What step-by-step actions did you take to obtain the information from the patient? What were the results of your actions?
A parent once didn’t disclose that the father of the child was not her current boyfriend. This was important as the patient was going to need consent forms signed, and legally, this boyfriend was not able to sign the consent forms. Additionally, there was a man calling the unit, claiming to be the father of the child. Social work and the nurse manager were notified.
Through an open conversation, the mother disclosed the correct identity of the father. While I personally did not discover the information, it is essential to know the resources that are available to you and utilize them to the best of your ability.
Interviewing isn’t easy—for anyone! It’s important to be overly prepared to put your best foot forward during every stage of the process. Nurse.org put together this super helpful workbook packed full of exercises, sample questions, and checklists to help you ace your next interview.

By clicking download, you agree to receive email newsletters and special offers from Nurse.org. You may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.
Your request has been received. Thanks!
Sample Nurse Interview Questions: Adaptability
The nursing profession is one of constant urgency, crisis, and uncertainty. Tell stories of challenges and follow up with key takeaways and learned lessons.
1. Tell me about a time you were under a lot of pressure. What was going on, and how did you get through it?
Tell a story about a time you were stressed and under pressure to perform. Explain the situation and why you felt pressured. Describe step-by-step the actions you took to make it through the situation. What was the result? What did you learn? What might you do differently now?
I was the most senior nurse in the unit by over a decade. I had to handle my patient assignments and act as a resource to the other newer nurses on the unit. I had to make sure my time management was great, as well as my ability to drop everything and help someone else. I had to stay organized; otherwise, I would not have been able to assist others.
2. Describe a time when your facility was undergoing some change. How did that impact you, and how did you adapt?
Talk about a time your facility changed. Maybe they were acquired by another facility. Perhaps they transitioned to a new computer system. Describe the change and the steps you took to adapt to such change.
One healthcare system I worked for switched from paper charting to electronic medical records and computerized charting. This transition was confusing and often overwhelming. I was able to adapt quickly, but unfortunately, some of my coworkers were not able to.
3. Tell me about a time when you didn’t know the answer to something at work. How did you go about finding the information?
Tell a story about a time when you did not know the answer. Explain step-by-step the action you took to find the information. Talk about the result of your actions.
As nurses, there is no way that we can possibly know everything. Knowing where to go for help is the first step. At the beginning of every shift, I identify a nurse that I can use as a resource, such as the charge nurse, nurse educator, or unit resource nurse. This individual is generally someone who is more senior with an advanced skill set.
If I am unable to get the answer from them or they are busy I look at the healthcare systems policy and procedure manager. If there is a concern regarding a medication dosage or interaction, I look to Lexi-Comp.
4. Give me an example of an awkward situation at work. How did you remove yourself from the situation?
Tell a story about an uncomfortable situation. What was the situation, and why did it feel awkward? Explain the steps you took to leave the situation. What were the results of your actions? What did you learn?
I once had a teenage male patient make very inappropriate sexual comments towards me. At first, I ignored them, thinking it was a one-time thing. The second time, I told him that the comments were inappropriate and I did not want him to say those things to me. The third time, I left the patient’s room and went directly to the charge nurse.
I explained the situation and how uncomfortable I was in caring for the patient. She gathered a team to speak to the patient. My assignment was switched for the remainder of the shift.
5. Tell me about a time you failed. How did you deal with this situation?
Share a story about when you experience failure. Talk about your feelings and why you felt that you failed. Discuss anything positive that came from this failure. What did you learn from failing? What might you do differently now?
Failing is one of the worst feelings in the world, either professionally or personally. Working in the ICU setting, patients die. We fail them when this happens. I fail them when this happens.
After every death, there is a debriefing to discuss what went well and what could have been done differently. I took that time to reflect on my participation in the event and if there was something I could have done differently. Failure doesn’t equal weakness. It simply is something that we must improve upon.
Sample Nurse Interview Questions: Time Management
Nurses are masters at multitasking - for example, managing multiple patients and administering medication on time while maintaining detailed notes. Tell stories about your punctuality, ability to meet deadlines, and how you remain organized through it all.
1. Talk about a time you worked in a fast-paced setting. How do you prioritize tasks while maintaining excellent patient care?
Give an example of a time you had to prioritize your tasks quickly. Explain your thought process in detail and why you chose to complete the duties in such an order.
Working in an ICU setting is extremely fast-paced, and it is essential to prioritize your tasks for the day. At the beginning of the shift, I make a to-do list with everything that needs to be accomplished. I put the must-do things at the top of the list and the things I would like to do at the bottom.
Administering medications is placed at the top of the list, and washing a patient’s hair is further down. While I would love to accomplish everything, it just isn’t possible.
2. Describe your experience with a very ill patient who required a lot of your time. How did you manage this patient’s care while ensuring your other patients were adequately cared for?
Talk about the patient’s care and why they needed much of your time. What was the illness, trauma or injury? How did you ensure that this patient received quality care? How did you manage your other patients?
Delegation is key here. Knowing when to ask for help is important. Without identifying resources and asking for help, success is impossible.
3. Talk about a time when you felt overwhelmed with your work or patient load. What did you do?
Give a specific example of a time you were overwhelmed. Explain step-by-step the actions you took to overcome this feeling and to focus on the task at hand.
I asked for help during these situations. Without identifying resources and asking for help, success is impossible.
4. Give an example of an important goal you set for yourself. Did you accomplish that goal? How did you ensure that you accomplished it?
Make sure the goal you share is related to your career. Explain the steps you took to accomplish your goal. What challenges did you face? How did you feel once you accomplished your goal?
I set the goal of earning my pediatric certification and made a list of things that I must do to achieve that. I signed up for the exam and paid the fee, so I had to take it. There was no backing out.
Sample Nurse Interview Questions: Communication Style
It is important to convey your particular communication style and techniques. Tell stories about specific times you either had difficulty communicating or times you communicated well. If you can, walk through your step-by-step thought process and give examples.
1. Give an example of a time when you were able to successfully persuade a patient to agree to something. How did you persuade this person?
Tell a story about a specific time when you had a difficult time getting a patient to agree to something at work. What was the situation, and what did they need to agree to? What specific actions did you take to get them to agree? What was the result?
Ideally, we never want to persuade a patient to do something. We would like the patient to agree to it freely. However, I did bargain with a child that if he ate his breakfast, I would play video games with him afterward. Using a bargaining system worked well to ensure the patient was well nourished.
2. Tell me about a time when you had to rely on written communication to explain yourself to your team or to a patient.
Talk about a time when you successfully relied on written (or typed) communication. What were the circumstances? What was being discussed? How did you ensure success?
Most hospitals utilize a text feature to communicate quickly with the medical team. It is important to be concise and provide all of the important information so that the medical team can determine the best course of action.
3. Talk about a time when you had not communicated well. How did you correct the situation?
No one is perfect; we all have flaws. Discuss a time when you experienced miscommunication at work. What were the circumstances? How did you know you did not communicate well? What did you learn? What were the results?
This often happens when there is a language barrier. I learned that it is always better to ask for an in-person interpreter or utilize computer translation software. This ensures there is no miscommunication of information. Unfortunately, hand gestures and speaking louder don’t always work.
4. Describe a time when you received negative feedback and turned it into something positive.
Discuss a time at work when you received negative feedback. What was the feedback and circumstances surrounding the feedback? Who gave you the negative feedback? How did it make you feel? What did you do as a result of the feedback?
I was once told that I needed to be more social at work and try and bond with my work colleagues. I disagreed with my manager because I felt that we were there to work and take care of our patients, not to make friends. Becoming close friends with coworkers is an added bonus.
While I didn’t become best friends with anyone from the unit, I was able to spend downtime reading and studying to earn additional certifications, which helped me secure better jobs and opportunities in nursing.
Sample Nurse Interview Questions: Motivation and Core Values
These questions are designed to help interviewers understand your motivation and personal values. When answering such questions, you should share motivational stories from your life that convey your core values.
1. What is one professional accomplishment that you are most proud of and why?
Tell a story about one of your most noteworthy accomplishments at work. What was the accomplishment? What steps did you take to achieve it? Who else was involved in this accomplishment? What happened as a result of the accomplishment?
Earning my advanced pediatric certification is something I worked very hard for, and it validates the years I have spent at the bedside.
2. Have you ever felt dissatisfied with your work as a Nurse? What could have been done to make it better?
Most nurses encounter difficulties while working. Talk about a time when you felt dissatisfied with your work. What were the circumstances, and what happened? What was your role? Why did you feel dissatisfied? What would you do differently now? What did you learn?
I once became extremely dissatisfied because I was consistently being given easier assignments and not being given the ICU level of patients. It became frustrating, and while I understood that others needed to learn and gain experience, it quickly left me annoyed with my position, the unit, and the healthcare system.
I sat down and spoke to my nurse manager about my concerns and inquired why it was happening. The nurse manager was not aware of the situation and it was later determined that a few of the charge nurses were giving the sicker patients to their friends and not spreading them out amongst the nurses.
3. Describe a time when you went over and above your job requirements. What motivated you to put forth the extra effort?
Talk about a specific instance when you went out of your way for your job or for a patient. What were the circumstances? Why did you choose to take the action? What did you do? What were the results?
I personally feel like I give 110% to all of my patients every shift, but there was one that I grew especially close with. For some reason, the patient had been dropped off by a family member, and no one had come to see the child for months. It was obvious the patient was missing key developmental milestones and was becoming increasingly lonely and depressed.
I asked to become the primary nurse for the patient, which meant every time I worked, he would be assigned to me. I worked with him over several months to get him potty trained and to improve his vocabulary. I don’t know exactly why I was extra motivated, but at that time in our lives, the patient and I needed each other.
4. Give an example of a mistake you’ve made. How did you handle it?
It is important to admit that you make mistakes and to own up to them. Talk about the specific mistake and why it happened. What was your role in the mistake? How did you know that you made a mistake? Who was involved? What did you learn? What have you done to improve? What were the results?
Mistakes are part of nursing, whether we like to admit to it or not. It’s important to learn from those mistakes and become a better nurse. One mistake that I will never forget is leaving the gastronomy tube unclamped with medication administration.
Because it was unclamped when I opened the port to give the next medication, the last medication, as well as formula, came out. I was unable to clamp it quickly enough, and the medications I had already given were leaking onto the bed.
I had to speak with the medical team and pharmacy to discuss replacing them. I have never forgotten to clamp the gastronomy tube again.
5. What do you find most difficult about being a Nurse? How do you overcome this difficulty?
Be honest and talk about the most difficult component of nursing. Maybe it’s working with a specific patient population. Or acting in a leadership role. Whatever it is to you, always make sure to talk about the steps and actions you’ve taken to cope with the difficulty.
The most difficult aspect of being a nurse is watching a patient die, especially one that I have cared for when they were healthy. Watching the family lose a loved one is heartbreaking. Sometimes I sit in the bathroom and take a moment for myself to cry, to reflect, and to pause to remember the patient. Death is part of our everyday world, and sometimes that is hard to remember.
Interviewing is a two-way street. Often, nurses are so excited and nervous about answering questions well during their interviews that they forget to ask questions to their potential future employers.
After all, how do you know if the job is an excellent fit unless you ask about the details that are important to you?
Most of the time, when you reach the end of your interview, employers will ask interviewees if they have any questions about the position. This is a great opportunity to show that you have done your research on their facility and expected job duties and demonstrate how excited you are about the position.
Depending on time, you may want to consider limiting your questions to two or three questions. Most nursing administrators set aside an allotted amount of time to interview each potential new hire, and you don’t want to be disrespectful of their time.
Many of these questions may also be great to ask after you have the job and work 1:1 with a preceptor or other helpful nurses. Experienced nurses are great resources for questions once you get the job!
Sample Questions To Ask During an Interview: Onboarding
- How long is the training period, and what does it entail?
- How will my training success be measured?
- Will I have orientation days, and what will they entail?
- What advice would you give to a nurse who is just starting on the unit?
- How quickly are you looking to hire someone?
- Who will I be reporting to?
- What shifts are you hiring for: night, day, mid-shift, or alternating?
- Will I be required to work on-call shifts?
Sample Questions To Ask During an Interview: Mentoring
- Will I be assigned a preceptor?
- How will my success as a new hire be measured?
- What is your training process for new hires?
- What advice do you have for a new hire who wants to succeed in this unit?
- How frequently do you perform performance reviews?
Sample Questions To Ask During an Interview: Culture
- Can you explain what the nursing culture is like here?
- Does the nursing staff face any ongoing challenges on the unit? What are the most critical challenges?
- What is the management style of this unit?
- What does an ideal candidate look like for this role?
- How does this nursing environment facilitate collaboration and unity?
Sample Questions To Ask During an Interview: Professional Development
- Are there any professional development opportunities?
- How long do nurses work at the bedside before taking on a charge nurse role?
- Do you offer tuition reimbursement for nurses advancing their education to take on higher-level nursing roles?
- Are nurses encouraged to become certified in their specialties?
- Will I be expected to float to other units? How often will that occur?
Sample Questions for New Nursing Graduates
- Do you offer a new nursing graduate program, how long is it, and what does it entail?
- How are new graduates measured on performance and competency?
- Do new graduates have a mentor? How long do they provide supervision and nursing support?
- What are the most common challenges new grads experience in this unit?
- When will I be eligible to become involved on unit committees?
Other Important Questions You May Want to Ask
You will not have enough time to ask all of these questions during your interview, but you may want to pick one or two to ask if there is any remaining time left.
Otherwise, keep these questions handy for when you have an opportunity to ask them in the future. They may help provide essential information to help you exceed expectations in your new job!
- What electronic medical record (EMR) system does this facility use?
- Describe the patient population on the unit and how many patients will we have at capacity?
- Do you have overtime policies for nurses who want to work extra shifts?
- What are staffing ratios here?
- How does the scheduling process work?
- What are your protocols for dealing with challenging or difficult patients?
Remember to ask what the next steps in the interview process are and express your interest in the position.
You may also want to ask if the hiring manager has any hesitations about hiring you based on your resume and work experience. That way, if they have any reservations, they can tell you, and you can rebuke them by explaining why they have no reason for hesitation.
For example, if the hiring manager says something like, “I am not sure that you have enough critical care experience to take on this position,” you can respond and assure them that you are perfect for the role.
You may want to say something like, “I have always wanted to work in a high-acuity environment. I am extremely dedicated and eager to learn new skills necessary to succeed in this role. I am like a sponge and ready to learn!”
Remember to close the interview on a high note before walking away.
How to Prepare for Your Nursing Interview
1. dress for success.
You don’t get a second chance to make a first impression! In fact, many hiring managers say they know if they are interested in hiring someone within the first five minutes.
It is essential to look professional and air on the more conservative side of style versus wearing bright and flashy clothing. Keep jewelry simple and understated. If it is appropriate to wear a suit, stick to neutral colors such as black, navy, or dark brown shades.
Your goal is to look as professional as possible so the person you are speaking with can focus on the essential skills you will bring to their organization.
2. Practice answering as many interview questions as you can out loud
Many interviewees review interview questions by reading them alone. But that may not help prepare you as well as speaking your answers out loud. In fact, you may find that you aren’t as clear on many of your answers as you thought you were.
Consider enlisting a friend or family member to act as the interviewer and ask you sample questions. Practice answering your questions and focus on ways you can communicate more effectively. Be assertive and don’t ramble. You will know if you are ready if you can answer questions clearly and constantly.
3. Research the institution thoroughly
LinkedIn is a great resource for learning about healthcare facilities and the types of employees who work there. Employers usually appreciate it when candidates show they have basic knowledge about an organization's goals.
The last thing you want is to be asked something about the organization and not have an answer for it.
4. Arrive at least 20 minutes or more before your interview starts
Arrive early enough that you can use the restroom if needed, straighten yourself up, and not feel rushed walking into the interview.
5. Bring a great attitude
Make sure you get plenty of shut-eye the night before your interview and eat a good breakfast. Drink coffee if it helps you perform at your best, but avoid it as it can make you jittery.
But most importantly, smile and bring a positive vibe. You are going to do great!
Phone Interviews
Many employers do an initial phone interview before bringing candidates in to meet face-to-face. This often helps recruiters weed out candidates who aren’t serious about a position and offer additional information to candidates to make sure they really want the job.
Bu phone interviews are just as important as in-person or online interviews.
Here are a few tips to remember:
- Prepare for a phone interview the same way you would for a face-to-face interview. You have no way of predicting what questions will be asked, and it's better to be overly prepared than under-prepared.
- Stand up while you are talking. Standing during a phone interview may help you project your answers more clearly than if you are sitting down.
- Keep your resume and cover letter within reach in case you are asked about them.
- Don’t eat or drink during the phone interview, even though they can’t see you.
- Shower and get ready as if it were a face-to-face interview. You will feel more confident and professional, and it may help you perform better.
Zoom Interview Tips
Ever since the start of the pandemic, Zoom interviews have become exceedingly common. Employers continue to utilize online interviewing because it is often more accessible and convenient for everyone involved.
Preparing for a Zoom interview is similar to preparing for an in-person or phone interview. However, there are several tips you should keep in mind:
1. Dress professionally as if you were going to a face-to-face interview
If you would have worn a suit to an in-person interview, consider wearing it for your Zoom interview. Remember that even though employers usually don’t see your lower half on Zoom, there is a slight chance you may have to stand up or grab something. So no pajama pants!
2. Make sure your background is set up nicely
The interviewer will see your surroundings, so make sure your background is clean and organized. Consider a blank wall so nothing distracts your interviewer from your amazing skills. Also, never have a window behind you because the light can drown you out.
3. Keep it quiet
If you have roommates, let them know you will be on a Zoom interview, and they must stay quiet. If you have pets that have the potential to interrupt your interview, make arrangements for them beforehand. The last thing you want is for your cat to walk right in front of your screen!
4. Set up your Zoom space and practice the day before
If you are new to Zoom, don’t fret! It is a fairly simple platform to use. But it may be a good idea to set yourself up beforehand and practice so there are no surprises.
5. Ensure a good internet connection
No connection, no interview! Ensure that a quality connection is set up early so you don’t have to scramble when you should be starting your interview.
6. Practice with a friend
If you are new to Zoom, you may not be aware of your body language or how you present over video. Consider making a few Zoom calls with friends and family to get comfortable with it and ensure that you have an excellent video presence.
Nursing Behavioral Interview Flash Cards With Answers
Healthcare employers are increasingly asking behavioral questions - this means they want to know exactly how you will perform during different circumstances. They will be asking for you to provide examples of specific scenarios. Sound overwhelming? Don’t fret; Nurse.org has over 50 behavioral interview questions to help you practice. We’ve even included sample answers!

What questions are asked in a nursing interview?
- Healthcare hiring managers usually ask behavioral-based interview questions. These questions help provide information about how you may handle specific situations in the workplace and allow you to show your critical thinking skills.
How do I prepare for a nursing interview?
- Preparing for your interview starts well in advance of your actual interview date. Here are a few essential tips to prepare for your nursing interview: Practice as many interview questions as you can, dress professionally, research the institution thoroughly, show up early, bring a great attitude, and relax. You will do great!
What are the four skills of a nursing interview?
- Listening actively and taking notes when appropriate. Asking important questions. Good non-verbal communication - ways to do this include leaning forward slightly, smiling, making good eye contact, and head nodding when appropriate. Answer behavioral questions with examples from your own work experience.
How do you introduce yourself in a nursing interview?
- Start with your name and a brief history of your education and work history. You may want to explain why you chose this career and are so passionate about it. It is also important to talk about why you make a good fit for the position and what your career goals are in the future.

Kathleen Gaines (nee Colduvell) is a nationally published writer turned Pediatric ICU nurse from Philadelphia with over 13 years of ICU experience. She has an extensive ICU background having formerly worked in the CICU and NICU at several major hospitals in the Philadelphia region. After earning her MSN in Education from Loyola University of New Orleans, she currently also teaches for several prominent Universities making sure the next generation is ready for the bedside. As a certified breastfeeding counselor and trauma certified nurse, she is always ready for the next nursing challenge.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. We will not sell or distribute your email address to any third party, and you may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.

ANA Nursing Resources Hub
Search Resources Hub

Critical Thinking in Nursing: Tips to Develop the Skill
4 min read • February, 09 2024
Critical thinking in nursing helps caregivers make decisions that lead to optimal patient care. In school, educators and clinical instructors introduced you to critical-thinking examples in nursing. These educators encouraged using learning tools for assessment, diagnosis, planning, implementation, and evaluation.
Nurturing these invaluable skills continues once you begin practicing. Critical thinking is essential to providing quality patient care and should continue to grow throughout your nursing career until it becomes second nature.
What Is Critical Thinking in Nursing?
Critical thinking in nursing involves identifying a problem, determining the best solution, and implementing an effective method to resolve the issue using clinical decision-making skills.
Reflection comes next. Carefully consider whether your actions led to the right solution or if there may have been a better course of action.
Remember, there's no one-size-fits-all treatment method — you must determine what's best for each patient.
How Is Critical Thinking Important for Nurses?
As a patient's primary contact, a nurse is typically the first to notice changes in their status. One example of critical thinking in nursing is interpreting these changes with an open mind. Make impartial decisions based on evidence rather than opinions. By applying critical-thinking skills to anticipate and understand your patients' needs, you can positively impact their quality of care and outcomes.
Elements of Critical Thinking in Nursing
To assess situations and make informed decisions, nurses must integrate these specific elements into their practice:
- Clinical judgment. Prioritize a patient's care needs and make adjustments as changes occur. Gather the necessary information and determine what nursing intervention is needed. Keep in mind that there may be multiple options. Use your critical-thinking skills to interpret and understand the importance of test results and the patient’s clinical presentation, including their vital signs. Then prioritize interventions and anticipate potential complications.
- Patient safety. Recognize deviations from the norm and take action to prevent harm to the patient. Suppose you don't think a change in a patient's medication is appropriate for their treatment. Before giving the medication, question the physician's rationale for the modification to avoid a potential error.
- Communication and collaboration. Ask relevant questions and actively listen to others while avoiding judgment. Promoting a collaborative environment may lead to improved patient outcomes and interdisciplinary communication.
- Problem-solving skills. Practicing your problem-solving skills can improve your critical-thinking skills. Analyze the problem, consider alternate solutions, and implement the most appropriate one. Besides assessing patient conditions, you can apply these skills to other challenges, such as staffing issues .

How to Develop and Apply Critical-Thinking Skills in Nursing
Critical-thinking skills develop as you gain experience and advance in your career. The ability to predict and respond to nursing challenges increases as you expand your knowledge and encounter real-life patient care scenarios outside of what you learned from a textbook.
Here are five ways to nurture your critical-thinking skills:
- Be a lifelong learner. Continuous learning through educational courses and professional development lets you stay current with evidence-based practice . That knowledge helps you make informed decisions in stressful moments.
- Practice reflection. Allow time each day to reflect on successes and areas for improvement. This self-awareness can help identify your strengths, weaknesses, and personal biases to guide your decision-making.
- Open your mind. Don't assume you're right. Ask for opinions and consider the viewpoints of other nurses, mentors , and interdisciplinary team members.
- Use critical-thinking tools. Structure your thinking by incorporating nursing process steps or a SWOT analysis (strengths, weaknesses, opportunities, and threats) to organize information, evaluate options, and identify underlying issues.
- Be curious. Challenge assumptions by asking questions to ensure current care methods are valid, relevant, and supported by evidence-based practice .
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills.
Images sourced from Getty Images
Related Resources

Item(s) added to cart

How To Improve Critical Thinking Skills In Nursing? 24 Strategies With Examples
Last updated on August 19th, 2023
Nurses play a critical role in making critical decisions that directly impact patient outcomes in the dynamic field of healthcare. Developing strong critical thinking skills is essential for success in this role.
In this article, we present a comprehensive list of 23 nursing-specific strategies aimed at improving critical thinking and improve the quality of patient care.
24 Strategies to improve critical thinking skills in nursing
You may also want to check out: 15 Attitudes of Critical Thinking in Nursing (Explained W/ Examples)
1. Reflective Journaling: Delving into Deeper Understanding
Reflective journaling is a potent tool for nurses to explore their experiences, actions, and decisions.
By regularly pondering over situations and analyzing their thought processes, nurses can identify strengths and areas for improvement.
This practice encourages the conscious development of critical thinking by comparing past experiences with current knowledge and exploring alternative solutions.
After a particularly challenging case, a nurse reflects on their decision-making process, exploring what worked well and what could have been done differently.
2. Meeting with Colleagues: Collaborative Learning for Critical Thinking
Regular interactions with colleagues foster a collaborative learning environment. Sharing experiences, discussing diverse viewpoints, and providing constructive feedback enhance critical thinking skills .
Colleagues’ insights can challenge assumptions and broaden perspectives, ultimately leading to more well-rounded clinical judgments.
A nursing team gathers to discuss a recent complex case, sharing their perspectives, insights, and lessons learned to collectively improve patient care strategies.
3. Concept Mapping: Visualizing Complexity
Concept mapping is an excellent technique to synthesize intricate patient information. By creating visual representations of patient problems and interventions, nurses can identify relationships and patterns that might not be apparent otherwise.
This strategy aids in comprehensive care planning and encourages nurses to think holistically about patient care.
Creating a concept map to connect patient symptoms, diagnostics, and interventions reveals patterns that help the nurse formulate a comprehensive care plan.
4. Socratic Questioning: Digging Deeper into Situations
The art of Socratic questioning involves asking probing questions that lead to deeper understanding.
Applying this technique allows nurses to uncover assumptions, examine inconsistencies, and explore multiple viewpoints.
This approach is especially valuable when reviewing patient history, discussing conditions, and planning care strategies.
When assessing a patient’s deteriorating condition, a nurse asks probing questions to uncover potential underlying causes and prioritize appropriate interventions.
5. Inductive and Deductive Reasoning: From Specifics to Generalizations
Developing skills in both inductive and deductive reasoning equips nurses to analyze situations from different angles.
Inductive reasoning involves drawing conclusions from specific observations, while deductive reasoning starts with general premises to arrive at specific conclusions.
Proficient use of these methods enhances nurses’ ability to make accurate clinical judgments.
When encountering a series of patients with similar symptoms, a nurse uses inductive reasoning to identify a common pattern and deduce potential causes.
6. Distinguishing Statements: Fact, Inference, Judgment, and Opinion
Clear thinking demands the ability to differentiate between statements of fact, inference, judgment, and opinion.
Nurses must critically evaluate information sources, ensuring they rely on evidence-based practice.
This skill safeguards against misinformation and supports informed decision-making.
While reviewing a patient’s history, a nurse differentiates factual medical information from inferences and subjective judgments made by different healthcare professionals.
7. Clarifying Assumptions: Promoting Effective Communication
Recognizing assumptions and clarifying their underlying principles is vital for effective communication. Nurses often hold differing assumptions, which can impact patient care.
By acknowledging these assumptions and encouraging open discussions, nursing teams can collaboratively create care plans that align with patients’ best interests.
Before suggesting a treatment plan, a nurse engages in a conversation with a patient to understand their cultural beliefs and preferences, ensuring assumptions are not made.
8. Clinical Simulations: Learning through Virtual Scenarios
Clinical simulations provide nurses with a risk-free environment to practice decision-making and problem-solving skills.
These virtual scenarios mimic real-life patient situations and allow nurses to test different approaches, assess outcomes, and reflect on their choices.
By engaging in simulations, nurses can refine their critical thinking abilities, learn from mistakes, and gain confidence in their clinical judgment.
Engaging in a simulated scenario where a patient’s condition rapidly changes challenges a nurse’s decision-making skills in a controlled environment.
9. Case Studies and Grand Rounds: Analyzing Complex Cases
Engaging in case studies and participating in grand rounds exposes nurses to complex patient cases that require in-depth analysis.
Working through these scenarios encourages nurses to consider various factors, potential interventions, and their rationale.
Discussing these cases with colleagues and experts fosters collaborative critical thinking and widens the spectrum of possible solutions.
Nurses participate in grand rounds, discussing a challenging case involving multiple medical specialties, encouraging a holistic approach to patient care.
10. Continuing Education and Lifelong Learning: Expanding Knowledge
Staying up-to-date with the latest advancements in nursing and healthcare is crucial for effective critical thinking.
Pursuing continuing education opportunities, attending conferences, and engaging in self-directed learning keeps nurses informed about new research, technologies, and best practices.
This continuous learning enriches their knowledge base, enabling them to approach patient care with a well-rounded perspective.
Attending a nursing conference on the latest advancements in wound care equips a nurse with evidence-based techniques to improve patient outcomes.
11. Debates and Discussions: Encouraging Thoughtful Dialogue
Organizing debates or participating in structured discussions on healthcare topics stimulates critical thinking.
Engaging in debates requires researching and presenting evidence-based arguments, promoting the evaluation of different perspectives.
Nurses can exchange insights, challenge assumptions, and refine their ability to defend their viewpoints logically.
Engaging in a debate on the pros and cons of a new treatment method encourages nurses to critically analyze different viewpoints and strengthen their own understanding.
12. Multidisciplinary Collaboration: Gaining Insights from Various Disciplines
Collaborating with professionals from diverse healthcare disciplines enriches nurses’ critical thinking.
Interacting with doctors, pharmacists, therapists, and other experts allows nurses to benefit from different viewpoints and approaches.
This cross-disciplinary collaboration broadens their understanding and encourages innovative problem-solving.
Collaborating with physical therapists, nutritionists, and pharmacists helps a nurse develop a holistic care plan that addresses all aspects of a patient’s recovery.
13. Ethical Dilemma Analysis: Balancing Patient Autonomy and Best Practice
Ethical dilemmas are common in nursing practice. Analyzing these situations requires nurses to weigh the principles of beneficence, non-maleficence, autonomy, and justice.
By critically examining ethical scenarios, nurses develop the capacity to navigate morally complex situations, prioritize patient welfare, and make ethically sound decisions.
When faced with a patient’s refusal of treatment due to religious beliefs, a nurse evaluates the ethical considerations, respects autonomy, and seeks alternatives.
14. Root Cause Analysis: Investigating Adverse Events
When adverse events occur, performing a root cause analysis helps identify the underlying causes and contributing factors.
Nurses engage in a systematic process of analyzing events, exploring the “5 Whys” technique , and developing strategies to prevent similar occurrences in the future.
This approach cultivates a thorough and analytical approach to problem-solving.
After a medication error, a nurse leads a root cause analysis to identify system failures and implement preventive measures to enhance patient safety.
15. Creative Thinking Exercises: Expanding Solution Repertoire
Encouraging creative thinking through brainstorming sessions or scenario-based exercises widens the range of possible solutions nurses consider.
By thinking outside the box and exploring innovative approaches, nurses develop adaptable problem-solving skills that can be applied to complex patient care challenges.
Brainstorming creative approaches to comfort a distressed pediatric patient empowers a nurse to find innovative methods beyond routine interventions.
16. Journal Clubs: Fostering Evidence-Based Discussion
Participating in journal clubs involves healthcare professionals coming together to dissect recent research articles.
This practice ignites critical thinking by allowing nurses to evaluate study methodologies, scrutinize findings, and consider the implications for their practice.
Engaging in evidence-based discussions not only cultivates a culture of critical inquiry but also reinforces continuous learning.
At the monthly journal club meeting, Nurse Mark engages in a discussion on a recent research article focusing on pain management strategies for post-operative patients.
The group analyzes the study design, scrutinizes the findings, and considers the potential implications for their practice.
During the discussion, Mark raises thought-provoking questions about the study’s methodology and suggests potential applications in their hospital’s patient care protocols.
This active participation in journal clubs not only refines Mark’s critical thinking but also instills evidence-based practices into his nursing approach.
17. Critical Reflection Groups: Collaborative Learning and Analysis
Similarly, establishing critical reflection groups, where nurses meet regularly to discuss experiences, cases, and challenges, fosters collective learning.
These sessions encourage the exchange of diverse perspectives, enriching the analysis process and ultimately enhancing patient care strategies.
Through shared insights and discussions, nurses can refine their clinical reasoning and broaden their problem-solving capabilities.
Nurse Emma actively participates in critical reflection groups in order to broaden her clinical knowledge. During a recent meeting, the group tackled a difficult patient case with complicated symptomatology.
Emma suggests alternative diagnostic pathways based on her own experiences. Emma’s critical thinking skills are honed as a result of the group’s dynamic interaction, which also emphasizes the importance of collaborative decision-making in complex scenarios.
18. Mindfulness and Reflection Practices: Enhancing Self-Awareness
Mindfulness techniques, such as meditation and deep breathing, encourage self-awareness and a clear mind.
Engaging in these practices helps nurses become more attuned to their thoughts and emotions, leading to better self-regulation and improved decision-making during high-pressure situations.
Engaging in mindfulness exercises before a demanding shift helps a nurse maintain focus, manage stress, and make clear-headed decisions.
19. Problem-Based Learning: Applying Knowledge in Real Scenarios
Problem-based learning involves presenting nurses with real-world patient cases and encouraging them to collaboratively solve the problems.
This approach bridges the gap between theoretical knowledge and practical application, fostering critical thinking through active problem-solving.
Working through a simulated patient case challenges nurses to apply theoretical knowledge to practical situations, refining their clinical reasoning.
20. Self-Assessment and Feedback: Evaluating Decision-Making Skills
Regularly assessing one’s own decision-making process and seeking feedback from peers and mentors is essential for improvement.
Reflecting on past decisions, considering alternative approaches, and understanding the rationale behind them contribute to the refinement of critical thinking skills.
A nurse evaluates their performance after a patient’s unexpected complication, seeking feedback from peers and mentors to identify areas for improvement.
21. Cultural Competence Training: Navigating Diverse Perspectives
Cultural competence training enhances critical thinking by enabling nurses to understand the diverse cultural beliefs and practices of patients.
This knowledge is vital for providing patient-centered care, as it encourages nurses to think critically about the unique needs of each individual.
A nurse attends cultural competence training to understand the dietary preferences of a diverse patient population, ensuring respectful and patient-centered care.
22. Active Listening and Empathetic Communication: Gathering Insights
Active listening and empathetic communication with patients and their families enable nurses to gather comprehensive information about their conditions, concerns, and preferences.
This data forms the basis for critical analysis and informed decision-making in patient care.
Through attentive listening, a nurse uncovers a patient’s underlying concerns, leading to an informed care plan that addresses both medical needs and emotional well-being.
23. Mentorship and Preceptorship: Learning from Experienced Professionals
Having a mentor or preceptor provides novice nurses with the opportunity to learn from experienced professionals.
Mentors guide critical thinking by sharing their insights, challenging assumptions, and offering guidance in complex situations. This relationship fosters growth and expertise development.
A novice nurse gains valuable insight from a mentor, who guides them through complex cases, offering real-world wisdom and refining critical thinking skills.
24. Self-Assessment and Feedback: Evaluating Decision-Making Skills
Reflecting on past decisions, considering alternative approaches, and understanding the rationale behind them contribute to the refinement of critical thinking skills .
Nurse Sarah regularly takes time to assess her decision-making skills by reviewing past patient cases. After a challenging case involving conflicting symptoms, she reflects on her initial approach, the outcomes, and what she could have done differently.
She seeks feedback from her senior colleague, who provides insights on alternative diagnostic paths. Sarah’s self-assessment and feedback-seeking process enable her to identify areas for improvement and refine her critical thinking in similar situations.
- Clinical Reasoning In Nursing (Explained W/ Example)
- 8 Stages Of The Clinical Reasoning Cycle
- What is Critical Thinking in Nursing? (Explained W/ Examples)
Enhancing critical thinking skills is an ongoing journey that transforms nursing practice.
Reflective journaling, collaborative learning, concept mapping, Socratic questioning , reasoning techniques, distinguishing statements, and clarifying assumptions all play integral roles in nurturing these skills.
By incorporating these strategies into their daily routines, nurses can improve their critical thinking skills.
Additionally, this will help nurses in navigating the complexities of the healthcare field with confidence, expertise, and the ability to make well-informed decisions that improve patient outcomes.
Comments are closed.
Medical & Legal Disclaimer
All the contents on this site are for entertainment, informational, educational, and example purposes ONLY. These contents are not intended to be used as a substitute for professional medical advice or practice guidelines. However, we aim to publish precise and current information. By using any content on this website, you agree never to hold us legally liable for damages, harm, loss, or misinformation. Read the privacy policy and terms and conditions.
Privacy Policy
Terms & Conditions
© 2024 nurseship.com. All rights reserved.

The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.
How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
- Nursing School
Critical Thinking Nursing Interview Questions
Critical thinking nursing interview questions feature prominently in any interview. They aren’t supposed to trip you up, but they will do just that if you aren’t ready.
Along with your nursing school application cover letter and your nursing school letter of intent , your nursing school interview questions give you an opportunity to show an admissions board, in your own words, how perfect you are for nursing school.
This article will show you how to take that opportunity and maximally utilize it to your advantage. We will go through what exactly a critical thinking question is, why they are being asked, and what types of responses you can give. Finally, we will cover several sample answers so that you can prepare your own answers for your upcoming interview.
>> Want us to help you get accepted? Schedule a free strategy call here . <<
Article Contents 7 min read
Why are critical thinking questions asked.
While critical thinking questions may relate to aspects of healthcare and nursing, including patient care, working as part of a team, and response to emergencies, they may also deal with dilemmas that have nothing to do with healthcare. For example, you may be faced with a conflict of interest scenario, or an ethical dilemma with a close friend.
Essentially, you’re being tested on your decision-making processes and how you solve problems, whether they are healthcare related or not. Your interviewer is trying to find out if you think logically, quickly, and in ways that provide good solutions in real-world scenarios.
Critical thinking is important to any job, but is of particular importance to nursing. Any healthcare professional deals with immense challenges on a daily basis. These challenges come up with little warning and require clearheaded responses.
Because the question is looking for your decision-making processes, you need to make sure that your responses put those processes in the limelight. Therefore, your answers should focus on the steps of how you made your decision and the why behind those steps: in other words, how you arrived at that response. You should show off how you evaluate situations and respond, but also how you concluded that your response was the most logical course of action.
Even if the question you are asked is hypothetical or situational, as we like to call it, you can definitely use your personal experiences to answer. Make sure to demonstrate non-judgmental attitude and objectivity when making your decision.
With nursing school interview questions, expert responses are required.
Let’s look at a sample critical thinking question and an expert response.
Prompt: Describe the most stressful event of your life. Why was it stressful, and how did you handle the situation?
Example: I\u2019m not saying it was easy, but that organization made things much more straightforward, and it helped to keep my mind calm and disciplined in all that chaos. I learned how to not only balance all of these disparate elements of my life, but that I could use the very act of balancing as a calming influence. "}]">
Nurses often have to deal with hostile patients. Can you recall a time you had to deal with hostility? What did you do and what were the results?
Sample answer:
I was working in a supporting role at a psychiatric institution, and one of the patients was a very angry person. He had a very quick temper and would often be physically violent, in addition to uncooperative or verbally abusive. The nurses said that giving meds felt like playing Russian roulette.
So, I would always make sure that I was around for that patient’s med time, ready to call security if he became violent.
He didn’t like taking his pills, either. One day, I was speaking with him and I discovered that his anger over medication was coming from a lack of understanding; he didn’t fully know what the pills did. So, I talked to his nurse about it, and she went over the reasons for his particular drugs and their side-effects. I also let his physician know about his concerns so that the doctor could have a conversation about it at her next visit in.
Once those issues had been dealt with, medication was much easier to distribute. It didn’t solve all the problems, but it helped make his days a lot smoother.
Critical thinking questions can be daunting and difficult, but they can also show some of your best talents and establish your abilities in a very concrete way. These aren’t abstract. These are demonstrations of actual actions taken. Use these questions to show off your impressive side with a committee.
The focus is the main difference, and with a critical thinking question, that focus is on how you use problem-solving and decision-making in different scenarios. They are to get a sense of how you deal with challenges and obstacles on a day-to-day basis.
Contrast this to more open-ended questions like “Tell us a little bit about yourself,” or “ Why do you want to be a nurse? ”
Fairly compact; you should answer in less than a minute.
Use just enough language to set up the problem you faced, your thought processes on how to deal with those problems, the actions you took, and the outcomes that those actions produced. This can be done in a fairly swift amount of time.
That doesn’t mean you should skimp on detail. While the interviewers don’t need every small thing that happened, they shouldn’t be confused or feel like they’re missing anything. Remember to showcase your abilities – don't brush past them: highlight!
Use mock interviews as part of your nursing school interview preparation to hone your answers for time and detail.
The most important reason is that you will wind up sounding robotic and insincere.
Additionally, the critical thinking questions might be slight variants, so a memorized answer could (or will) end up not quite fitting the question.
Better to memorize scenarios than words so that you can apply those examples to any question that comes up.
You can, and sometimes are directly asked to provide an example of failure.
If an interviewer asks you to describe a time you failed at implementing critical thinking, of course you must supply them with something, and should prepare for such questions in their own right.
Remember that they are looking for your decision-making processes and skills, so the outcome might have been bad, but if your processes were excellent, the interviewer will make note of that. Sometimes even good decisions lead to negative outcomes – sometimes that’s inevitable.
If you failed to apply good critical thinking in a situation, you can highlight what you learned from the experience and how it has improved subsequent actions and decision-making processes.
Failure is only truly failure if no lessons were learned.
You can take a short pause to think, and give yourself enough time to recall an appropriate event or incident. It’s important to research the different types of nursing school interview questions and prepare a relevant story for a variety of scenarios.
While it is unlikely that you will be asked about something that you can’t relate to at all (most of the questions are broad enough to allow some sort of connection) it might happen that you just haven’t had a given experience yet.
You can’t just say, “That’s never happened to me,” and leave it at that.
However, you might want to acknowledge this by saying, “That exact thing has never happened to me, but I have had a similar experience,” and speak of the closest thing you have to what was asked. Perhaps it wasn’t a work or healthcare setting, but maybe something that happened with family members or friends in a social setting, for instance – that will do.
Get as close as you can to the question, acknowledge the discrepancy, and answer to the best of your ability.
Expect anything, because depending on the interview, almost anything can be covered.
Even the type of interview can change, depending on the school. Some will use a traditional panel-style interview, but others will use the multiple mini-interview (MMI) format. If the latter, you might want to learn more about how to prepare for your multiple mini interview .
What exactly is in the interview depends on the school and panel, so be ready for anything.
Want more free tips? Subscribe to our channels for more free and useful content!
Apple Podcasts
Like our blog? Write for us ! >>
Have a question ask our admissions experts below and we'll answer your questions, get started now.
Talk to one of our admissions experts
Our site uses cookies. By using our website, you agree with our cookie policy .
FREE Training Webclass:
How to improve your nursing school interview practice score by 27% , using the proven strategies they don’t want you to know.
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Effective decision-making: applying the theories to nursing practice.
Samantha Watkins
Emergency Department Staff Nurse, Frimley Health NHS Foundation Trust, Frimley
View articles · Email Samantha
Many theories have been proposed for the decision-making conducted by nurses across all practices and disciplines. These theories are fundamental to consider when reflecting on our decision-making processes to inform future practice. In this article three of these theories are juxtaposed with a case study of a patient presenting with an ST-segment elevation myocardial infarction (STEMI). These theories are descriptive, normative and prescriptive, and will be used to analyse and interpret the process of decision-making within the context of patient assessment.
Decision-making is a fundamental concept of nursing practice that conforms to a systematic trajectory involving the assessment, interpretation, evaluation and management of patient-specific situations ( Dougherty et al, 2015 ). Shared decision-making is vital to consider in terms of patient autonomy and professional duty of care as set out in the Nursing and Midwifery Council (NMC) (2018) Code, which underpins nursing practice. Consequently, the following assessment and decision-making processes were conducted within the remits of practice as a student nurse. Decision-making is a dynamic process in nursing practice, and the theories emphasise the importance of adaptability and reflective practice to identify factors that impact on patient care ( Pearson, 2013 ). Three decision-making theories will be explored within the context of a decision made in practice. To abide by confidentiality requirements, the pseudonym ‘Linda’ will be used throughout. Patient consent was obtained prior to writing.
Register now to continue reading
Thank you for visiting British Journal of Nursing and reading some of our peer-reviewed resources for nurses. To read more, please register today. You’ll enjoy the following great benefits:
What's included
Limited access to clinical or professional articles
Unlimited access to the latest news, blogs and video content
Signing in with your registered email address
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Nurse leaders as problem-solvers
Addressing lateral and horizontal violence.
Anthony, Michelle R. PhD, RN; Brett, Anne Liners PhD, RN
Michelle R. Anthony is a program coordinator at Columbia (S.C.) VA Health Care System. Anne Liners Brett is doctoral faculty at the University of Phoenix in Tempe, Ariz.
Acknowledgment: The authors acknowledge the support of the University of Phoenix Center for Educational and Instructional Technology Research.
The contents of this article do not represent the views of the US Department of Veterans Affairs or the United States Government.
The authors and planners have disclosed no potential conflicts of interest, financial or otherwise.
For more than 126 additional continuing-education articles related to management topics, go to NursingCenter.com/CE .
Earn CE credit online: Go to http://nursing.ceconnection.com and receive a certificate within minutes .
Read about a qualitative, grounded theory study that looked to gain a deeper understanding of nurse leaders' perceptions of their role in addressing lateral and horizontal violence, and the substantive theory developed from the results.

The issue of lateral and horizontal violence (LHV) has plagued the nursing profession for more than 3 decades, yet solutions remain elusive. The significance of LHV isn't lost on nurse leaders because it creates an unhealthy work environment. Research literature worldwide has continued to report the prevalence of disruptive behaviors experienced by nursing students, novice nurses, and seasoned nurses in the workforce. The World Health Organization, International Council of Nurses, and Public Services International have recognized this issue as a major global public health priority. 1
LHV, also called nurse-on-nurse aggression, disruptive behavior, or incivility, undermines a culture of safety and negatively impacts patient care. 2,3 This experience, known to nurses as “eating their young,” isn't only intimidating and disruptive, it's also costly and demoralizing to the nursing profession and healthcare organizations. 4,5 Although the impact of LHV can be dreadful for both the institution and its staff, little is known about the reasons for these behaviors among nursing professionals. 2
LHV encompasses all acts of meanness, hostility, disruption, discourtesy, backbiting, divisiveness, criticism, lack of unison, verbal or mental abuse, and scapegoating. 6 The sole intent of bullying behaviors is to purposefully humiliate and demean victims. Bullying behaviors also taint healthcare organizations; cause irreparable harm to workplace culture; breakdown team communication; and severely impact the quality of the care provided, thereby jeopardizing patient safety. 7,8 Researchers have reported that acts of LHV are used to demonstrate power, domination, or aggression; for retribution; to control others; and to enhance self-image. 9-12
Previous studies have shown that the frequency of LHV in healthcare organizations is quite severe, with about 90% of new nurses surveyed reporting acts of incivility by their coworkers. 13 Sixty-five percent of nurses in one survey reported witnessing incidents of despicable acts, whereas another 46% of coworkers in the same survey reported the issue as “very serious” and “somewhat serious.” 13
LHV poses a significant challenge for nurse leaders who are legally and morally responsible for providing a safe working environment. 2,6 The purpose of this qualitative, grounded theory study was to gain a deeper understanding of nurse leaders' perceptions of their role in addressing LHV and develop a substantive theory from the results.
Literature review
A paucity of evidence exists in the literature regarding how nurse leaders perceive their role in addressing LHV. 14 Studies have shown that this phenomenon is attributed to heavy workloads, a stressful work environment, and lack of workgroup cohesiveness, as well as organizational factors such as misuse of authority and the lack of organizational policies and procedures for addressing LHV behaviors. 15
In one study, one-third of the nurses reported that they had observed emotional abuse during several of their work shifts. 16 Another study indicated that 30% of survey respondents (n = 2,100) stated LHV occurs weekly. 17 A third study revealed that 25% of participants noted LHV happened monthly, and a fourth study of ED nurses reported that about 27.3% of the nurses had experienced LHV perpetrated by nursing leadership (managers, supervisors, charge nurses, and directors), physicians, or peers in the last 6 months. 18
In a survey completed by members of the Washington State Emergency Nurses Association, 27% of respondents experienced acts of bullying in the past 6 months. 19 Another study reported that 27% to 85% of nurse respondents had experienced some form of uncivil behavior. 20 Other data have shown that those more vulnerable to violent, disruptive, and intimidating behaviors are newly licensed nurses beginning their careers. 21
Although nurse leaders can be perpetrators of LHV, they play an essential role in addressing LHV behaviors and creating a safe work environment. 22 The literature suggests that, in many cases, a lack of awareness and response by nurse leaders adds to the prevalence of LHV. 23 This may be due, in part, to nurse leaders being aligned with the perpetrators who are creating the toxic work environment. 6 The literature suggests that an environment where staff members feel safe to practice results in a culture that decreases burnout and promotes nurse retention and quality outcomes. 24,25
This qualitative, grounded theory study focused on nurse leaders' perception of their role in breaking the cycle of LHV for staff members whom they supervise. Two research questions guided the study: 1. How do nurse leaders perceive their role in addressing LHV among nursing staff members under their supervision? 2. What substantive theory may emerge from the data collected during interviews with nurse leaders?
A grounded theory methodology was used to explore the nurse leader's role in addressing LHV with the intent of developing a substantive theory through the meaningful organization of data themes to provide a framework to address the phenomenon of LHV. Purposive sampling was used to recruit a total of 14 participants for this study from a large healthcare system in the Southeastern US. The participants were chosen because of their experience with LHV and their ability to discuss and reflect on those experiences. Informed consent was obtained before the start of the study, which included explaining the reason for the study and what to expect. In addition, permission was obtained from the Institutional Review Board.
Data collection and analysis
Demographic data collected to describe the sample included gender, age range, number of years holding a management position, supervisory responsibility, and highest degree obtained. (See Table 1 .)

Semistructured, in-depth interviews were the primary mode of data collection. The recorded interviews were conducted face-to-face and lasted about 60 minutes. Data collection continued until saturation was achieved. Data saturation occurred when no new descriptive codes, categories, or themes were emerging from the analyzed data. The interviews were transcribed verbatim and verified through a member check process.
During the data analysis process, themes and patterns were identified. Data from each participant's interview were examined to determine if the responses were aligned with the identified themes. Analysis of the data included coding at increasingly abstract levels and constant comparison. Qualitative software assisted in coding the information and uncovering subtle trends.
Four themes emerged from core categories developed during the qualitative data coding process.
Theme 1: Understanding/addressing LHV . In question one, participants were asked to describe their understanding of LHV. Five subthemes emerged from the data collected with this question. (See Table 2 .)

Theme 2: Experience addressing LHV . In the second question, participants were asked about their experience with addressing incidents of LHV. Six subthemes were identified. (See Table 3 .)

Theme 3: Role perception in addressing LHV . In the third question, participants were asked what they perceive their role to be in addressing LHV. Six subthemes resulted from this question. (See Table 4 .)

Theme 4: Organizational impediment to addressing LHV . In question four, participants were asked to describe the factors within the organization that influence or impede their role in addressing LHV. This question yielded nine subthemes. (See Table 5 .)

Substantive theory
As a result of the themes that emerged from the data, a substantive theory was developed. This is especially important for the nursing profession to develop as a scientifically based practice. Theories help guide research and provide the expansion, generation, and validation of the science of nursing knowledge. 26 The substantive theory will help nurse leaders become more cognizant of the role that effective leadership plays in preventing or intervening in incidents of LHV in the workplace. The analysis revealed that nurse leaders are aware that the quality of patient care and staff well-being can be adversely affected by the impact of LHV.
Data themes were used to formulate the following theory: Nurse leaders address LHV affecting their staff members by solving problems, creating a safe work environment, and reducing institutional barriers that impede addressing LHV in a timely fashion. Nurse leaders perceive their role as a problem-solver, which is a necessary step in advocacy. 27 Problem-solving is a process that contains the elements of decision-making and critical thinking. 28
The theory that emerged from the core categories explicitly focused on the central phenomenon of LHV in the nursing work environment. Figure 1 shows the interrelatedness of the themes to the resultant substantive theory.

Discussion and implications
The study results have several implications for both the nursing profession and nurse leaders. The nursing profession requires decisive and robust leadership, and the role of the nurse leader is to be a combination of nurturer, investigator, and judge to examine incidents of LHV. 26,29-32 Nurse leaders are responsible for setting the tone and expectations for a safe work environment. This includes modeling the expected ethical behaviors; for example, doing the right things for the right reasons, being collegial toward each other, and being respectful of other's differences. One participant remarked, “This is a different world based on how I was raised. I was raised to be respectful to people.”
In addition, nurse leaders are responsible for enforcing policies created to address disruptive behaviors and working with the administration as soon as an incident occurs. Past research indicates that a healthy and collaborative work environment fosters nurse engagement and patient safety. 25,30 Staff members and patients need a leader to protect them when necessary; thus, the nurse leader needs to “walk the walk” in providing a safe environment for all. Nurse leaders engaged in these kinds of behaviors are providing strong leadership and practicing strong decision-making, thus ensuring the continued robustness of their organizations.
Recommendations and limitations
Future research could replicate this study in a different geographic region to explore the causes of LHV by soliciting the views of nursing students, new graduate nurses, and nurse educators from unionized and nonunionized hospital systems and comparing the results to further understand this phenomenon. Additionally, developing a tool to test the substantive theory could substantiate the nurse leader's role as a problem-solver to address incidence of LHV in the workplace.
The decision to conduct this study in one type of healthcare organization limits the ability to compare the interviewed nurse leaders' experiences with nurse leaders in other healthcare organizations. The experiences of nurses in other healthcare organizations may be different; thus, overall generalizability of the study may be limited.
Say “no” to the status quo
The results of this study support the findings of previous researchers. 23,31,33,34 Accepting the status quo is unacceptable and can cause irreparable harm to organizational well-being if LHV isn't addressed. Collaboration between nurse leaders and administrators is essential to successfully reduce institutional obstacles that prevent the timely handling of LHV incidents. The role of the nurse leader as a problem-solver should be clear, defined, and well supported to seek resolutions to toxic behaviors that are hurting the work environment. But we must remember that creating a policy doesn't equal change. Every employee from the lowest level in the organization to the highest ranks of administration must model civil behaviors.
INSTRUCTIONS Nurse leaders as problem-solvers: Addressing lateral and horizontal violence
Test instructions.
- Read the article. The test for this CE activity is to be taken online at http://nursing.ceconnection.com .
- You'll need to create (it's free!) and login to your personal CE Planner account before taking online tests. Your planner will keep track of all your Lippincott Professional Development online CE activities for you.
- There's only one correct answer for each question. A passing score for this test is 14 correct answers. If you pass, you can print your certificate of earned contact hours and access the answer key. If you fail, you have the option of taking the test again at no additional cost.
- For questions, contact Lippincott Professional Development: 1-800-787-8985 .
- Registration deadline is June 3, 2022 .
PROVIDER ACCREDITATION
Lippincott Professional Development will award 1.5 contact hours for this continuing nursing education activity.
Lippincott Professional Development is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center's Commission on Accreditation.
This activity is also provider approved by the California Board of Registered Nursing, Provider Number CEP 11749 for 1.5 contact hours, and the District of Columbia, Georgia, and Florida CE Broker #50-1223.
Payment: The registration fee for this test is $17.95.
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Leadership strategies to promote frontline nursing staff engagement, how leadership matters: clinical nurses' perceptions of leader behaviors..., keeping the peace: conflict management strategies for nurse managers, quality improvement engagement: barriers and facilitators, relational leadership: a contemporary and evidence-based approach to improve....
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Fundamentals [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2021.

Nursing Fundamentals [Internet].
- About Open RN
Chapter 4 Nursing Process
4.1. nursing process introduction, learning objectives.
- Use the nursing process to provide patient care
- Identify nursing diagnoses from evidence-based sources
- Describe the development of a care plan
- Prioritize patient care
- Describe documentation for each step of the nursing process
- Differentiate between the role of the PN and RN
Have you ever wondered how a nurse can receive a quick handoff report from another nurse and immediately begin providing care for a patient they previously knew nothing about? How do they know what to do? How do they prioritize and make a plan?
Nurses do this activity every shift. They know how to find pertinent information and use the nursing process as a critical thinking model to guide patient care. The nursing process becomes a road map for the actions and interventions that nurses implement to optimize their patients’ well-being and health. This chapter will explain how to use the nursing process as standards of professional nursing practice to provide safe, patient-centered care.
4.2. BASIC CONCEPTS
Before learning how to use the nursing process, it is important to understand some basic concepts related to critical thinking and nursing practice. Let’s take a deeper look at how nurses think.
Critical Thinking and Clinical Reasoning
Nurses make decisions while providing patient care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.” [ 1 ] Using critical thinking means that nurses take extra steps to maintain patient safety and don’t just “follow orders.” It also means the accuracy of patient information is validated and plans for caring for patients are based on their needs, current clinical practice, and research.
“Critical thinkers” possess certain attitudes that foster rational thinking. These attitudes are as follows:
- Independence of thought: Thinking on your own
- Fair-mindedness: Treating every viewpoint in an unbiased, unprejudiced way
- Insight into egocentricity and sociocentricity: Thinking of the greater good and not just thinking of yourself. Knowing when you are thinking of yourself (egocentricity) and when you are thinking or acting for the greater good (sociocentricity)
- Intellectual humility: Recognizing your intellectual limitations and abilities
- Nonjudgmental: Using professional ethical standards and not basing your judgments on your own personal or moral standards
- Integrity: Being honest and demonstrating strong moral principles
- Perseverance: Persisting in doing something despite it being difficult
- Confidence: Believing in yourself to complete a task or activity
- Interest in exploring thoughts and feelings: Wanting to explore different ways of knowing
- Curiosity: Asking “why” and wanting to know more
Clinical reasoning is defined as, “A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions.” [ 2 ] To make sound judgments about patient care, nurses must generate alternatives, weigh them against the evidence, and choose the best course of action. The ability to clinically reason develops over time and is based on knowledge and experience. [ 3 ]
Inductive and Deductive Reasoning and Clinical Judgment
Inductive and deductive reasoning are important critical thinking skills. They help the nurse use clinical judgment when implementing the nursing process.
Inductive reasoning involves noticing cues, making generalizations, and creating hypotheses. Cues are data that fall outside of expected findings that give the nurse a hint or indication of a patient’s potential problem or condition. The nurse organizes these cues into patterns and creates a generalization. A generalization is a judgment formed from a set of facts, cues, and observations and is similar to gathering pieces of a jigsaw puzzle into patterns until the whole picture becomes more clear. Based on generalizations created from patterns of data, the nurse creates a hypothesis regarding a patient problem. A hypothesis is a proposed explanation for a situation. It attempts to explain the “why” behind the problem that is occurring. If a “why” is identified, then a solution can begin to be explored.
No one can draw conclusions without first noticing cues. Paying close attention to a patient, the environment, and interactions with family members is critical for inductive reasoning. As you work to improve your inductive reasoning, begin by first noticing details about the things around you. A nurse is similar to the detective looking for cues in Figure 4.1 . [ 4 ] Be mindful of your five primary senses: the things that you hear, feel, smell, taste, and see. Nurses need strong inductive reasoning patterns and be able to take action quickly, especially in emergency situations. They can see how certain objects or events form a pattern (i.e., generalization) that indicates a common problem (i.e., hypothesis).
Inductive Reasoning Includes Looking for Cues
Example: A nurse assesses a patient and finds the surgical incision site is red, warm, and tender to the touch. The nurse recognizes these cues form a pattern of signs of infection and creates a hypothesis that the incision has become infected. The provider is notified of the patient’s change in condition, and a new prescription is received for an antibiotic. This is an example of the use of inductive reasoning in nursing practice.
Deductive reasoning is another type of critical thinking that is referred to as “top-down thinking.” Deductive reasoning relies on using a general standard or rule to create a strategy. Nurses use standards set by their state’s Nurse Practice Act, federal regulations, the American Nursing Association, professional organizations, and their employer to make decisions about patient care and solve problems.
Example: Based on research findings, hospital leaders determine patients recover more quickly if they receive adequate rest. The hospital creates a policy for quiet zones at night by initiating no overhead paging, promoting low-speaking voices by staff, and reducing lighting in the hallways. (See Figure 4.2 ). [ 5 ] The nurse further implements this policy by organizing care for patients that promotes periods of uninterrupted rest at night. This is an example of deductive thinking because the intervention is applied to all patients regardless if they have difficulty sleeping or not.
Deductive Reasoning Example: Implementing Interventions for a Quiet Zone Policy
Clinical judgment is the result of critical thinking and clinical reasoning using inductive and deductive reasoning. Clinical judgment is defined by the National Council of State Boards of Nursing (NCSBN) as, “The observed outcome of critical thinking and decision-making. It uses nursing knowledge to observe and assess presenting situations, identify a prioritized patient concern, and generate the best possible evidence-based solutions in order to deliver safe patient care.” [ 6 ] The NCSBN administers the national licensure exam (NCLEX) that measures nursing clinical judgment and decision-making ability of prospective entry-level nurses to assure safe and competent nursing care by licensed nurses.
Evidence-based practice (EBP) is defined by the American Nurses Association (ANA) as, “A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and patient, family, group, community, and population preferences and values.” [ 7 ]
Nursing Process
The nursing process is a critical thinking model based on a systematic approach to patient-centered care. Nurses use the nursing process to perform clinical reasoning and make clinical judgments when providing patient care. The nursing process is based on the Standards of Professional Nursing Practice established by the American Nurses Association (ANA). These standards are authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently. [ 8 ] The mnemonic ADOPIE is an easy way to remember the ANA Standards and the nursing process. Each letter refers to the six components of the nursing process: A ssessment, D iagnosis, O utcomes Identification, P lanning, I mplementation, and E valuation.
The nursing process is a continuous, cyclic process that is constantly adapting to the patient’s current health status. See Figure 4.3 [ 9 ] for an illustration of the nursing process.
The Nursing Process
Review Scenario A in the following box for an example of a nurse using the nursing process while providing patient care.
Patient Scenario A: Using the Nursing Process [ 10 ]

A hospitalized patient has a prescription to receive Lasix 80mg IV every morning for a medical diagnosis of heart failure. During the morning assessment, the nurse notes that the patient has a blood pressure of 98/60, heart rate of 100, respirations of 18, and a temperature of 98.7F. The nurse reviews the medical record for the patient’s vital signs baseline and observes the blood pressure trend is around 110/70 and the heart rate in the 80s. The nurse recognizes these cues form a pattern related to fluid imbalance and hypothesizes that the patient may be dehydrated. The nurse gathers additional information and notes the patient’s weight has decreased 4 pounds since yesterday. The nurse talks with the patient and validates the hypothesis when the patient reports that their mouth feels like cotton and they feel light-headed. By using critical thinking and clinical judgment, the nurse diagnoses the patient with the nursing diagnosis Fluid Volume Deficit and establishes outcomes for reestablishing fluid balance. The nurse withholds the administration of IV Lasix and contacts the health care provider to discuss the patient’s current fluid status. After contacting the provider, the nurse initiates additional nursing interventions to promote oral intake and closely monitor hydration status. By the end of the shift, the nurse evaluates the patient status and determines that fluid balance has been restored.
In Scenario A, the nurse is using clinical judgment and not just “following orders” to administer the Lasix as scheduled. The nurse assesses the patient, recognizes cues, creates a generalization and hypothesis regarding the fluid status, plans and implements nursing interventions, and evaluates the outcome. Additionally, the nurse promotes patient safety by contacting the provider before administering a medication that could cause harm to the patient at this time.
The ANA’s Standards of Professional Nursing Practice associated with each component of the nursing process are described below.
The “Assessment” Standard of Practice is defined as, “The registered nurse collects pertinent data and information relative to the health care consumer’s health or the situation.” [ 11 ] A registered nurse uses a systematic method to collect and analyze patient data. Assessment includes physiological data, as well as psychological, sociocultural, spiritual, economic, and lifestyle data. For example, a nurse’s assessment of a hospitalized patient in pain includes the patient’s response to pain, such as the inability to get out of bed, refusal to eat, withdrawal from family members, or anger directed at hospital staff. [ 12 ]
The “Assessment” component of the nursing process is further described in the “ Assessment ” section of this chapter.
The “Diagnosis” Standard of Practice is defined as, “The registered nurse analyzes the assessment data to determine actual or potential diagnoses, problems, and issues.” [ 13 ] A nursing diagnosis is the nurse’s clinical judgment about the client's response to actual or potential health conditions or needs. Nursing diagnoses are the bases for the nurse’s care plan and are different than medical diagnoses. [ 14 ]
The “Diagnosis” component of the nursing process is further described in the “ Diagnosis ” section of this chapter.
Outcomes Identification
The “Outcomes Identification” Standard of Practice is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.” [ 15 ] The nurse sets measurable and achievable short- and long-term goals and specific outcomes in collaboration with the patient based on their assessment data and nursing diagnoses.
The “Outcomes Identification” component of the nursing process is further described in the “ Outcomes Identification ” section of this chapter.
The “Planning” Standard of Practice is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.” [ 16 ] Assessment data, diagnoses, and goals are used to select evidence-based nursing interventions customized to each patient’s needs and concerns. Goals, expected outcomes, and nursing interventions are documented in the patient’s nursing care plan so that nurses, as well as other health professionals, have access to it for continuity of care. [ 17 ]
The “Planning” component of the nursing process is further described in the “ Planning ” section of this chapter.
NURSING CARE PLANS
Creating nursing care plans is a part of the “Planning” step of the nursing process. A nursing care plan is a type of documentation that demonstrates the individualized planning and delivery of nursing care for each specific patient using the nursing process. Registered nurses (RNs) create nursing care plans so that the care provided to the patient across shifts is consistent among health care personnel. Some interventions can be delegated to Licensed Practical Nurses (LPNs) or trained Unlicensed Assistive Personnel (UAPs) with the RN’s supervision. Developing nursing care plans and implementing appropriate delegation are further discussed under the “ Planning ” and “ Implementing ” sections of this chapter.
Implementation
The “Implementation” Standard of Practice is defined as, “The nurse implements the identified plan.” [ 18 ] Nursing interventions are implemented or delegated with supervision according to the care plan to assure continuity of care across multiple nurses and health professionals caring for the patient. Interventions are also documented in the patient’s electronic medical record as they are completed. [ 19 ]
The “Implementation” Standard of Professional Practice also includes the subcategories “Coordination of Care” and “Health Teaching and Health Promotion” to promote health and a safe environment. [ 20 ]
The “Implementation” component of the nursing process is further described in the “ Implementation ” section of this chapter.
The “Evaluation” Standard of Practice is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.” [ 21 ] During evaluation, nurses assess the patient and compare the findings against the initial assessment to determine the effectiveness of the interventions and overall nursing care plan. Both the patient’s status and the effectiveness of the nursing care must be continuously evaluated and modified as needed. [ 22 ]
The “Evaluation” component of the nursing process is further described in the “ Evaluation ” section of this chapter.
Benefits of Using the Nursing Process
Using the nursing process has many benefits for nurses, patients, and other members of the health care team. The benefits of using the nursing process include the following:
- Promotes quality patient care
- Decreases omissions and duplications
- Provides a guide for all staff involved to provide consistent and responsive care
- Encourages collaborative management of a patient’s health care problems
- Improves patient safety
- Improves patient satisfaction
- Identifies a patient’s goals and strategies to attain them
- Increases the likelihood of achieving positive patient outcomes
- Saves time, energy, and frustration by creating a care plan or path to follow
By using these components of the nursing process as a critical thinking model, nurses plan interventions customized to the patient’s needs, plan outcomes and interventions, and determine whether those actions are effective in meeting the patient’s needs. In the remaining sections of this chapter, we will take an in-depth look at each of these components of the nursing process. Using the nursing process and implementing evidence-based practices are referred to as the “science of nursing.” Let’s review concepts related to the “art of nursing” while providing holistic care in a caring manner using the nursing process.
Holistic Nursing Care
The American Nurses Association (ANA) recently updated the definition of nursing as, “Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in the recognition of the connection of all humanity.” [ 23 ]
The ANA further describes nursing is a learned profession built on a core body of knowledge that integrates both the art and science of nursing. The art of nursing is defined as, “Unconditionally accepting the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care.” [ 24 ]
Nurses care for individuals holistically, including their emotional, spiritual, psychosocial, cultural, and physical needs. They consider problems, issues, and needs that the person experiences as a part of a family and a community as they use the nursing process. Review a scenario illustrating holistic nursing care provided to a patient and their family in the following box.
Holistic Nursing Care Scenario
A single mother brings her child to the emergency room for ear pain and a fever. The physician diagnoses the child with an ear infection and prescribes an antibiotic. The mother is advised to make a follow-up appointment with their primary provider in two weeks. While providing discharge teaching, the nurse discovers that the family is unable to afford the expensive antibiotic prescribed and cannot find a primary care provider in their community they can reach by a bus route. The nurse asks a social worker to speak with the mother about affordable health insurance options and available providers in her community and follows up with the prescribing physician to obtain a prescription for a less expensive generic antibiotic. In this manner, the nurse provides holistic care and advocates for improved health for the child and their family.
Review how to provide culturally responsive care and reduce health disparities in the “ Diverse Patients ” chapter.
Caring and the nursing process.
The American Nurses Association (ANA) states, “The act of caring is foundational to the practice of nursing.” [ 25 ] Successful use of the nursing process requires the development of a care relationship with the patient. A care relationship is a mutual relationship that requires the development of trust between both parties. This trust is often referred to as the development of rapport and underlies the art of nursing. While establishing a caring relationship, the whole person is assessed, including the individual’s beliefs, values, and attitudes, while also acknowledging the vulnerability and dignity of the patient and family. Assessing and caring for the whole person takes into account the physical, mental, emotional, and spiritual aspects of being a human being. [ 26 ] Caring interventions can be demonstrated in simple gestures such as active listening, making eye contact, touching, and verbal reassurances while also respecting and being sensitive to the care recipient’s cultural beliefs and meanings associated with caring behaviors. [ 27 ] See Figure 4.4 [ 28 ] for an image of a nurse using touch as a therapeutic communication technique to communicate caring.
Touch as a Therapeutic Communication Technique
Review how to communicate with patients using therapeutic communication techniques like active listening in the “ Communication ” chapter.
Dr. Jean Watson is a nurse theorist who has published many works on the art and science of caring in the nursing profession. Her theory of human caring sought to balance the cure orientation of medicine, giving nursing its unique disciplinary, scientific, and professional standing with itself and the public. Dr. Watson’s caring philosophy encourages nurses to be authentically present with their patients while creating a healing environment. [ 29 ]
Read more about Dr. Watson’s theory of caring at the Watson Caring Science Institute .
Now that we have discussed basic concepts related to the nursing process, let’s look more deeply at each component of the nursing process in the following sections.
4.3. ASSESSMENT
Assessment is the first step of the nursing process (and the first Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse collects pertinent data and information relative to the health care consumer’s health or the situation.” This includes collecting “pertinent data related to the health and quality of life in a systematic, ongoing manner, with compassion and respect for the wholeness, inherent dignity, worth, and unique attributes of every person, including but not limited to, demographics, environmental and occupational exposures, social determinants of health, health disparities, physical, functional, psychosocial, emotional, cognitive, spiritual/transpersonal, sexual, sociocultural, age-related, environmental, and lifestyle/economic assessments.” [ 1 ]
Nurses assess patients to gather clues, make generalizations, and diagnose human responses to health conditions and life processes. Patient data is considered either subjective or objective, and it can be collected from multiple sources.
Subjective Assessment Data
Subjective data is information obtained from the patient and/or family members and offers important cues from their perspectives. When documenting subjective data stated by a patient, it should be in quotation marks and start with verbiage such as, The patient reports. It is vital for the nurse to establish rapport with a patient to obtain accurate, valuable subjective data regarding the mental, emotional, and spiritual aspects of their condition.
There are two types of subjective information, primary and secondary. Primary data is information provided directly by the patient. Patients are the best source of information about their bodies and feelings, and the nurse who actively listens to a patient will often learn valuable information while also promoting a sense of well-being. Information collected from a family member, chart, or other sources is known as secondary data . Family members can provide important information, especially for individuals with memory impairments, infants, children, or when patients are unable to speak for themselves.
See Figure 4.5 [ 2 ] for an illustration of a nurse obtaining subjective data and establishing rapport after obtaining permission from the patient to sit on the bed.
Example. An example of documented subjective data obtained from a patient assessment is, “The patient reports, ‘My pain is a level 2 on a 1-10 scale.’”
Objective Assessment Data
Objective data is anything that you can observe through your sense of hearing, sight, smell, and touch while assessing the patient. Objective data is reproducible, meaning another person can easily obtain the same data. Examples of objective data are vital signs, physical examination findings, and laboratory results. See Figure 4.6 [ 3 ] for an image of a nurse performing a physical examination.
Physical Examination
Example. An example of documented objective data is, “The patient’s radial pulse is 58 and regular, and their skin feels warm and dry.”
Sources of Assessment Data
There are three sources of assessment data: interview, physical examination, and review of laboratory or diagnostic test results.
Interviewing
Interviewing includes asking the patient questions, listening, and observing verbal and nonverbal communication. Reviewing the chart prior to interviewing the patient may eliminate redundancy in the interview process and allows the nurse to hone in on the most significant areas of concern or need for clarification. However, if information in the chart does not make sense or is incomplete, the nurse should use the interview process to verify data with the patient.
After performing patient identification, the best way to initiate a caring relationship is to introduce yourself to the patient and explain your role. Share the purpose of your interview and the approximate time it will take. When beginning an interview, it may be helpful to start with questions related to the patient’s medical diagnoses to gather information about how they have affected the patient’s functioning, relationships, and lifestyle. Listen carefully and ask for clarification when something isn’t clear to you. Patients may not volunteer important information because they don’t realize it is important for their care. By using critical thinking and active listening, you may discover valuable cues that are important to provide safe, quality nursing care. Sometimes nursing students can feel uncomfortable having difficult conversations or asking personal questions due to generational or other cultural differences. Don’t shy away from asking about information that is important to know for safe patient care. Most patients will be grateful that you cared enough to ask and listen.
Be alert and attentive to how the patient answers questions, as well as when they do not answer a question. Nonverbal communication and body language can be cues to important information that requires further investigation. A keen sense of observation is important. To avoid making inappropriate inferences , the nurse should validate any cues. For example, a nurse may make an inference that a patient is depressed when the patient avoids making eye contact during an interview. However, upon further questioning, the nurse may discover that the patient’s cultural background believes direct eye contact to be disrespectful and this is why they are avoiding eye contact. To read more information about communicating with patients, review the “ Communication ” chapter of this book.
A physical examination is a systematic data collection method of the body that uses the techniques of inspection, auscultation, palpation, and percussion. Inspection is the observation of a patient’s anatomical structures. Auscultation is listening to sounds, such as heart, lung, and bowel sounds, created by organs using a stethoscope. Palpation is the use of touch to evaluate organs for size, location, or tenderness. Percussion is an advanced physical examination technique typically performed by providers where body parts are tapped with fingers to determine their size and if fluid is present. Detailed physical examination procedures of various body systems can be found in the Open RN Nursing Skills textbook with a head-to-toe checklist in Appendix C . Physical examination also includes the collection and analysis of vital signs.
Registered Nurses (RNs) complete the initial physical examination and analyze the findings as part of the nursing process. Collection of follow-up physical examination data can be delegated to Licensed Practical Nurses/Licensed Vocational Nurses (LPNs/LVNs) , or measurements such as vital signs and weight may be delegated to trained Unlicensed Assistive Personnel (UAP) when appropriate to do so. However, the RN remains responsible for supervising these tasks, analyzing the findings, and ensuring they are documented .
A physical examination can be performed as a comprehensive, head-to-toe assessment or as a focused assessment related to a particular condition or problem. Assessment data is documented in the patient’s Electronic Medical Record (EMR) , an electronic version of the patient’s medical chart.
Reviewing Laboratory and Diagnostic Test Results
Reviewing laboratory and diagnostic test results provides relevant and useful information related to the needs of the patient. Understanding how normal and abnormal results affect patient care is important when implementing the nursing care plan and administering provider prescriptions. If results cause concern, it is the nurse’s responsibility to notify the provider and verify the appropriateness of prescriptions based on the patient’s current status before implementing them.
Types of Assessments
Several types of nursing assessment are used in clinical practice:
- Primary Survey: Used during every patient encounter to briefly evaluate level of consciousness, airway, breathing, and circulation and implement emergency care if needed.
- Admission Assessment: A comprehensive assessment completed when a patient is admitted to a facility that involves assessing a large amount of information using an organized approach.
- Ongoing Assessment: In acute care agencies such as hospitals, a head-to-toe assessment is completed and documented at least once every shift. Any changes in patient condition are reported to the health care provider.
- Focused Assessment: Focused assessments are used to reevaluate the status of a previously diagnosed problem.
- Time-lapsed Reassessment: Time-lapsed reassessments are used in long-term care facilities when three or more months have elapsed since the previous assessment to evaluate progress on previously identified outcomes. [ 4 ]
Putting It Together
Review Scenario C in the following box to apply concepts of assessment to a patient scenario.
Scenario C [5]

Ms. J. is a 74-year-old woman who is admitted directly to the medical unit after visiting her physician because of shortness of breath, increased swelling in her ankles and calves, and fatigue. Her medical history includes hypertension (30 years), coronary artery disease (18 years), heart failure (2 years), and type 2 diabetes (14 years). She takes 81 mg of aspirin every day, metoprolol 50 mg twice a day, furosemide 40 mg every day, and metformin 2,000 mg every day.
Ms. J.’s vital sign values on admission were as follows:
- Blood Pressure: 162/96 mm Hg
- Heart Rate: 88 beats/min
- Oxygen Saturation: 91% on room air
- Respiratory Rate: 28 breaths/minute
- Temperature: 97.8 degrees F orally
Her weight is up 10 pounds since the last office visit three weeks prior. The patient states, “I am so short of breath” and “My ankles are so swollen I have to wear my house slippers.” Ms. J. also shares, “I am so tired and weak that I can’t get out of the house to shop for groceries,” and “Sometimes I’m afraid to get out of bed because I get so dizzy.” She confides, “I would like to learn more about my health so I can take better care of myself.”
The physical assessment findings of Ms. J. are bilateral basilar crackles in the lungs and bilateral 2+ pitting edema of the ankles and feet. Laboratory results indicate a decreased serum potassium level of 3.4 mEq/L.
As the nurse completes the physical assessment, the patient’s daughter enters the room. She confides, “We are so worried about mom living at home by herself when she is so tired all the time!”
Critical Thinking Questions
Identify subjective data.
Identify objective data.
Provide an example of secondary data.
Answers are located in the Answer Key at the end of the book.
4.4. DIAGNOSIS
Diagnosis is the second step of the nursing process (and the second Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse analyzes assessment data to determine actual or potential diagnoses, problems, and issues.” The RN “prioritizes diagnoses, problems, and issues based on mutually established goals to meet the needs of the health care consumer across the health–illness continuum and the care continuum.” Diagnoses, problems, strengths, and issues are documented in a manner that facilitates the development of expected outcomes and a collaborative plan. [ 1 ]
Analyzing Assessment Data
After collection of assessment data, the registered nurse analyzes the data to form generalizations and create hypotheses for nursing diagnoses. Steps for analyzing assessment data include performing data analysis, clustering of information, identifying hypotheses for potential nursing diagnosis, performing additional in-depth assessment as needed, and establishing nursing diagnosis statements. The nursing diagnoses are then prioritized and drive the nursing care plan. [ 2 ]
Performing Data Analysis
After nurses collect assessment data from a patient, they use their nursing knowledge to analyze that data to determine if it is “expected” or “unexpected” or “normal” or “abnormal” for that patient according to their age, development, and baseline status. From there, nurses determine what data are “clinically relevant” as they prioritize their nursing care. [ 3 ]
Example. In Scenario C in the “Assessment” section of this chapter, the nurse analyzes the vital signs data and determines the blood pressure, heart rate, and respiratory rate are elevated, and the oxygen saturation is decreased for this patient. These findings are considered “relevant cues.”
Clustering Information/Seeing Patterns/Making Hypotheses
After analyzing the data and determining relevant cues, the nurse clusters data into patterns. Assessment frameworks such as Gordon’s Functional Health Patterns assist nurses in clustering information according to evidence-based patterns of human responses. See the box below for an outline of Gordon’s Functional Health Patterns. [ 4 ] Concepts related to many of these patterns will be discussed in chapters later in this book.
Example. Refer to Scenario C of the “Assessment” section of this chapter. The nurse clusters the following relevant cues: elevated blood pressure, elevated respiratory rate, crackles in the lungs, weight gain, worsening edema, shortness of breath, a medical history of heart failure, and currently prescribed a diuretic medication. These cues are clustered into a generalization/pattern of fluid balance, which can be classified under Gordon’s Nutritional-Metabolic Functional Health Pattern. The nurse makes a hypothesis that the patient has excess fluid volume present.
Gordon’s Functional Health Patterns [ 5 ]
Health Perception-Health Management: A patient’s perception of their health and well-being and how it is managed
Nutritional-Metabolic: Food and fluid consumption relative to metabolic need
Elimination: Excretory function, including bowel, bladder, and skin
Activity-Exercise: Exercise and daily activities
Sleep-Rest: Sleep, rest, and daily activities
Cognitive-Perceptual: Perception and cognition
Self-perception and Self-concept: Self-concept and perception of self-worth, self-competency, body image, and mood state
Role-Relationship: Role engagements and relationships
Sexuality-Reproductive: Reproduction and satisfaction or dissatisfaction with sexuality
Coping-Stress Tolerance: Coping and effectiveness in terms of stress tolerance
Value-Belief: Values, beliefs (including spiritual beliefs), and goals that guide choices and decisions
Identifying Nursing Diagnoses
After the nurse has analyzed and clustered the data from the patient assessment, the next step is to begin to answer the question, “What are my patient’s human responses (i.e., nursing diagnoses)?” A nursing diagnosis is defined as, “A clinical judgment concerning a human response to health conditions/life processes, or a vulnerability for that response, by an individual, family, group, or community.” [ 6 ] Nursing diagnoses are customized to each patient and drive the development of the nursing care plan. The nurse should refer to a care planning resource and review the definitions and defining characteristics of the hypothesized nursing diagnoses to determine if additional in-depth assessment is needed before selecting the most accurate nursing diagnosis.
Nursing diagnoses are developed by nurses, for use by nurses. For example, NANDA International (NANDA-I) is a global professional nursing organization that develops nursing terminology that names actual or potential human responses to health problems and life processes based on research findings. [ 7 ] Currently, there are over 220 NANDA-I nursing diagnoses developed by nurses around the world. This list is continuously updated, with new nursing diagnoses added and old nursing diagnoses retired that no longer have supporting evidence. A list of commonly used NANDA-I diagnoses are listed in Appendix A . For a full list of NANDA-I nursing diagnoses, refer to a current nursing care plan reference.
NANDA-I nursing diagnoses are grouped into 13 domains that assist the nurse in selecting diagnoses based on the patterns of clustered data. These domains are similar to Gordon’s Functional Health Patterns and include health promotion, nutrition, elimination and exchange, activity/rest, perception/cognition, self-perception, role relationship, sexuality, coping/stress tolerance, life principles, safety/protection, comfort, and growth/development.
Knowledge regarding specific NANDA-I nursing diagnoses is not assessed on the NCLEX. However, analyzing cues and creating hypotheses are part of the measurement model used to assess a candidate’s clinical judgment. Read more about the NCLEX and Next Generation NCLEX in the “ Scope of Practice ” chapter.
Nursing diagnoses vs. medical diagnoses.
You may be asking yourself, “How are nursing diagnoses different from medical diagnoses?” Medical diagnoses focus on diseases or other medical problems that have been identified by the physician, physician’s assistant, or advanced nurse practitioner. Nursing diagnoses focus on the human response to health conditions and life processes and are made independently by RNs. Patients with the same medical diagnosis will often respond differently to that diagnosis and thus have different nursing diagnoses. For example, two patients have the same medical diagnosis of heart failure. However, one patient may be interested in learning more information about the condition and the medications used to treat it, whereas another patient may be experiencing anxiety when thinking about the effects this medical diagnosis will have on their family. The nurse must consider these different responses when creating the nursing care plan. Nursing diagnoses consider the patient’s and family’s needs, attitudes, strengths, challenges, and resources as a customized nursing care plan is created to provide holistic and individualized care for each patient.
Example. A medical diagnosis identified for Ms. J. in Scenario C in the “Assessment” section is heart failure. This cannot be used as a nursing diagnosis, but it can be considered as an “associated condition” when creating hypotheses for nursing diagnoses. Associated conditions are medical diagnoses, injuries, procedures, medical devices, or pharmacological agents that are not independently modifiable by the nurse, but support accuracy in nursing diagnosis. The nursing diagnosis in Scenario C will be related to the patient’s response to heart failure.
Additional Definitions Used in NANDA-I Nursing Diagnoses
The following definitions of patient, age, and time are used in association with NANDA-I nursing diagnoses:
The NANDA-I definition of a “patient” includes:
- Individual: a single human being distinct from others (i.e., a person).
- Caregiver: a family member or helper who regularly looks after a child or a sick, elderly, or disabled person.
- Family: two or more people having continuous or sustained relationships, perceiving reciprocal obligations, sensing common meaning, and sharing certain obligations toward others; related by blood and/or choice.
- Group: a number of people with shared characteristics generally referred to as an ethnic group.
- Community: a group of people living in the same locale under the same governance. Examples include neighborhoods and cities. [ 8 ]
The age of the person who is the subject of the diagnosis is defined by the following terms: [ 9 ]
- Fetus: an unborn human more than eight weeks after conception, until birth.
- Neonate: a person less than 28 days of age.
- Infant: a person greater than 28 days and less than 1 year of age.
- Child: a person aged 1 to 9 years
- Adolescent: a person aged 10 to 19 years
- Adult: a person older than 19 years of age unless national law defines a person as being an adult at an earlier age.
- Older adult: a person greater than 65 years of age.
The duration of the diagnosis is defined by the following terms: [ 10 ]
- Acute: lasting less than 3 months.
- Chronic: lasting greater than 3 months.
- Intermittent: stopping or starting again at intervals
- Continuous: uninterrupted, going on without stop.
New Terms Used in 2018-2020 NANDA-I Diagnoses
The 2018-2020 edition of Nursing Diagnoses includes two new terms to assist in creating nursing diagnoses: at-risk populations and associated conditions. [ 11 ]
At-Risk Populations are groups of people who share a characteristic that causes each member to be susceptible to a particular human response, such as demographics, health/family history, stages of growth/development, or exposure to certain events/experiences.
Associated Conditions are medical diagnoses, injuries, procedures, medical devices, or pharmacological agents. These conditions are not independently modifiable by the nurse, but support accuracy in nursing diagnosis [ 12 ]
Types of Nursing Diagnoses
There are four types of NANDA-I nursing diagnoses: [ 13 ]
- Problem-Focused
- Health Promotion – Wellness
A problem-focused nursing diagnosis is a “clinical judgment concerning an undesirable human response to health condition/life processes that exist in an individual, family, group, or community.” [ 14 ] To make an accurate problem-focused diagnosis, related factors and defining characteristics must be present. Related factors (also called etiology) are causes that contribute to the diagnosis. Defining characteristics are cues, signs, and symptoms that cluster into patterns. [ 15 ]
A health promotion-wellness nursing diagnosis is “a clinical judgment concerning motivation and desire to increase well-being and to actualize human health potential.” These responses are expressed by the patient’s readiness to enhance specific health behaviors. [ 16 ] A health promotion-wellness diagnosis is used when the patient is willing to improve a lack of knowledge, coping, or other identified need.
A risk nursing diagnosis is “a clinical judgment concerning the vulnerability of an individual, family, group, or community for developing an undesirable human response to health conditions/life processes.” [ 17 ] A risk nursing diagnosis must be supported by risk factors that contribute to the increased vulnerability. A risk nursing diagnosis is different from the problem-focused diagnosis in that the problem has not yet actually occurred. Problem diagnoses should not be automatically viewed as more important than risk diagnoses because sometimes a risk diagnosis can have the highest priority for a patient. [ 18 ]
A syndrome diagnosis is a “clinical judgment concerning a specific cluster of nursing diagnoses that occur together, and are best addressed together and through similar interventions.” [ 19 ]
Establishing Nursing Diagnosis Statements
When using NANDA-I nursing diagnoses, NANDA-I recommends the structure of a nursing diagnosis should be a statement that includes the nursing diagnosis and related factors as exhibited by defining characteristics . The accuracy of the nursing diagnosis is validated when a nurse is able to clearly link the defining characteristics, related factors, and/or risk factors found during the patient’s assessment. [ 20 ]
To create a nursing diagnosis statement, the registered nurse completes the following steps. After analyzing the patient’s subjective and objective data and clustering the data into patterns, the nurse generates hypotheses for nursing diagnoses based on how the patterns meet defining characteristics of a nursing diagnosis. Defining characteristics is the terminology used for observable signs and symptoms related to a nursing diagnosis. [ 21 ] Defining characteristics are included in care planning resources for each nursing diagnosis, along with a definition of that diagnosis, so the nurse can select the most accurate diagnosis. For example, objective and subjective data such as weight, height, and dietary intake can be clustered together as defining characteristics for the nursing diagnosis of nutritional status.
When creating a nursing diagnosis statement, the nurse also identifies the cause of the problem for that specific patient. Related factors is the terminology used for the underlying causes (etiology) of a patient’s problem or situation. Related factors should not be a medical diagnosis, but instead should be attributed to the underlying pathophysiology that the nurse can treat. When possible, the nursing interventions planned for each nursing diagnosis should attempt to modify or remove these related factors that are the underlying cause of the nursing diagnosis. [ 22 ]
Creating nursing diagnosis statements has traditionally been referred to as “using PES format.” The PES mnemonic no longer applies to the current terminology used by NANDA-I, but the components of a nursing diagnosis statement remain the same. A nursing diagnosis statement should contain the problem, related factors, and defining characteristics. These terms fit under the former PES format in this manner:
Problem (P) – the patient p roblem (i.e., the nursing diagnosis)
Etiology (E) – related factors (i.e., the e tiology/cause) of the nursing diagnosis; phrased as “related to” or “R/T”
Signs and Symptoms (S) – defining characteristics manifested by the patient (i.e., the s igns and s ymptoms/subjective and objective data) that led to the identification of that nursing diagnosis for the patient; phrased with “as manifested by” or “as evidenced by.”
Examples of different types of nursing diagnoses are further explained below.
Problem-Focused Nursing Diagnosis
A problem-focused nursing diagnosis contains all three components of the PES format :
Problem (P) – statement of the patient response (nursing diagnosis)
Etiology (E) – related factors contributing to the nursing diagnosis
Signs and Symptoms (S) – defining characteristics manifested by that patient
SAMPLE PROBLEM-FOCUSED NURSING DIAGNOSIS STATEMENT
Refer to Scenario C of the “Assessment” section of this chapter. The cluster of data for Ms. J. (elevated blood pressure, elevated respiratory rate, crackles in the lungs, weight gain, worsening edema, and shortness of breath) are defining characteristics for the NANDA-I Nursing Diagnosis Excess Fluid Volume . The NANDA-I definition of Excess Fluid Volume is “surplus intake and/or retention of fluid.” The related factor (etiology) of the problem is that the patient has excessive fluid intake. [ 23 ]
The components of a problem-focused nursing diagnosis statement for Ms. J. would be:
Fluid Volume Excess
Related to excessive fluid intake
As manifested by bilateral basilar crackles in the lungs, bilateral 2+ pitting edema of the ankles and feet, increased weight of 10 pounds, and the patient reports, “ My ankles are so swollen .”
A correctly written problem-focused nursing diagnosis statement for Ms. J. would look like this:
Fluid Volume Excess related to excessive fluid intake as manifested by bilateral basilar crackles in the lungs, bilateral 2+ pitting edema of the ankles and feet, an increase weight of 10 pounds, and the patient reports, “My ankles are so swollen.”
Health-Promotion Nursing Diagnosis
A health-promotion nursing diagnosis statement contains the problem (P) and the defining characteristics (S). The defining characteristics component of a health-promotion nursing diagnosis statement should begin with the phrase “expresses desire to enhance”: [ 24 ]
Signs and Symptoms (S) – the patient’s expressed desire to enhance
SAMPLE HEALTH-PROMOTION NURSING DIAGNOSIS STATEMENT
Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. demonstrates a readiness to improve her health status when she told the nurse that she would like to “learn more about my health so I can take better care of myself.” This statement is a defining characteristic of the NANDA-I nursing diagnosis Readiness for Enhanced Health Management , which is defined as “a pattern of regulating and integrating into daily living a therapeutic regimen for the treatment of illness and its sequelae, which can be strengthened.” [ 25 ]
The components of a health-promotion nursing diagnosis for Ms. J. would be:
Problem (P): Readiness for Enhanced Health Management
Symptoms (S): Expressed desire to “learn more about my health so I can take better care of myself.”
A correctly written health-promotion nursing diagnosis statement for Ms. J. would look like this:
Enhanced Readiness for Health Promotion as manifested by expressed desire to “learn more about my health so I can take better care of myself.”
Risk Nursing Diagnosis
A risk nursing diagnosis should be supported by evidence of the patient’s risk factors for developing that problem. Different experts recommend different phrasing. NANDA-I 2018-2020 recommends using the phrase “as evidenced by” to refer to the risk factors for developing that problem. [ 26 ]
A risk diagnosis consists of the following:
As Evidenced By – Risk factors for developing the problem

SAMPLE RISK DIAGNOSIS STATEMENT
Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. has an increased risk of falling due to vulnerability from the dizziness and weakness she is experiencing. The NANDA-I definition of Risk for Falls is “increased susceptibility to falling, which may cause physical harm and compromise health.” [ 27 ]
The components of a risk diagnosis statement for Ms. J. would be:
Problem (P) – Risk for Falls
As Evidenced By – Dizziness and decreased lower extremity strength
A correctly written risk nursing diagnosis statement for Ms. J. would look like this:
Risk for Falls as evidenced by dizziness and decreased lower extremity strength.
Syndrome Diagnosis
A syndrome is a cluster of nursing diagnoses that occur together and are best addressed together and through similar interventions. To create a syndrome diagnosis, two or more nursing diagnoses must be used as defining characteristics (S) that create a syndrome. Related factors may be used if they add clarity to the definition, but are not required. [ 28 ]
A syndrome statement consists of these items:
Problem (P) – the syndrome
Signs and Symptoms (S) – the defining characteristics are two or more similar nursing diagnoses
SAMPLE SYNDROME DIAGNOSIS STATEMENT
Refer to Scenario C in the “Assessment” section of this chapter. Clustering the data for Ms. J. identifies several similar NANDA-I nursing diagnoses that can be categorized as a syndrome . For example, Activity Intolerance is defined as “insufficient physiological or psychological energy to endure or complete required or desired daily activities.” Social Isolation is defined as “aloneness experienced by the individual and perceived as imposed by others and as a negative or threatening state.” These diagnoses can be included under the the NANDA-I syndrome named Risk for Frail Elderly Syndrome. This syndrome is defined as a “dynamic state of unstable equilibrium that affects the older individual experiencing deterioration in one or more domains of health (physical, functional, psychological, or social) and leads to increased susceptibility to adverse health effects, in particular disability.” [ 29 ]
The components of a syndrome nursing diagnosis for Ms. J. would be:
– Risk for Frail Elderly Syndrome
– The nursing diagnoses of Activity Intolerance and Social Isolation
Additional related factor: Fear of falling
A correctly written syndrome diagnosis statement for Ms. J. would look like this:
Risk for Frail Elderly Syndrome related to activity intolerance, social isolation, and fear of falling
Prioritization
After identifying nursing diagnoses, the next step is prioritization according to the specific needs of the patient. Nurses prioritize their actions while providing patient care multiple times every day. Prioritization is the process that identifies the most significant nursing problems, as well as the most important interventions, in the nursing care plan.
It is essential that life-threatening concerns and crises are identified immediately and addressed quickly. Depending on the severity of a problem, the steps of the nursing process may be performed in a matter of seconds for life-threatening concerns. In critical situations, the steps of the nursing process are performed through rapid clinical judgment. Nurses must recognize cues signaling a change in patient condition, apply evidence-based practices in a crisis, and communicate effectively with interprofessional team members. Most patient situations fall somewhere between a crisis and routine care.
There are several concepts used to prioritize, including Maslow’s Hierarchy of Needs, the “ABCs” (Airway, Breathing and Circulation), and acute, uncompensated conditions. See the infographic in Figure 4.7 [30] on The How To of Prioritization .
The How To of Prioritization
Maslow’s Hierarchy of Needs is used to categorize the most urgent patient needs. The bottom levels of the pyramid represent the top priority needs of physiological needs intertwined with safety. See Figure 4.8 [31] for an image of Maslow’s Hierarchy of Needs. You may be asking yourself, “What about the ABCs – isn’t airway the most important?” The answer to that question is “it depends on the situation and the associated safety considerations.” Consider this scenario – you are driving home after a lovely picnic in the country and come across a fiery car crash. As you approach the car, you see that the passenger is not breathing. Using Maslow’s Hierarchy of Needs to prioritize your actions, you remove the passenger from the car first due to safety even though he is not breathing. After ensuring safety and calling for help, you follow the steps to perform cardiopulmonary resuscitation (CPR) to establish circulation, airway, and breathing until help arrives.
Maslow’s Hierarchy of Needs
In addition to using Maslow’s Hierarchy of Needs and the ABCs of airway, breathing, and circulation, the nurse also considers if the patient’s condition is an acute or chronic problem. Acute, uncompensated conditions generally require priority interventions over chronic conditions. Additionally, actual problems generally receive priority over potential problems, but risk problems sometimes receive priority depending on the patient vulnerability and risk factors.
Example. Refer to Scenario C in the “Assessment” section of this chapter. Four types of nursing diagnoses were identified for Ms. J.: Fluid Volume Excess, Enhanced Readiness for Health Promotion, Risk for Falls , and Risk for Frail Elderly Syndrome . The top priority diagnosis is Fluid Volume Excess because it affects the physiological needs of breathing, homeostasis, and excretion. However, the Risk for Falls diagnosis comes in a close second because of safety implications and potential injury that could occur if the patient fell.
American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020 . Thieme Publishers New York. ↵
Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
Gordon, M. (2008). Assess notes: Nursing assessment and diagnostic reasoning. F.A. Davis Company. ↵
NANDA International. (n.d.). Glossary of terms . https://nanda .org/nanda-i-resources /glossary-of-terms / ↵
NANDA International. (n.d.). Glossary of terms . https://nanda .org/nanda-i-resources /glossary-of-terms/ ↵
NANDA International. (n.d.). Glossary of terms. https://nanda .org/nanda-i-resources /glossary-of-terms/ ↵
“The How To of Prioritization” by Valerie Palarski for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
“ Maslow's hierarchy of needs.svg ” by J. Finkelstein is licensed under CC BY-SA 3.0 ↵
4.5. OUTCOME IDENTIFICATION
Outcome Identification is the third step of the nursing process (and the third Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.” The RN collaborates with the health care consumer, interprofessional team, and others to identify expected outcomes integrating the health care consumer’s culture, values, and ethical considerations. Expected outcomes are documented as measurable goals with a time frame for attainment. [ 1 ]
An outcome is a “measurable behavior demonstrated by the patient responsive to nursing interventions.” [ 2 ] Outcomes should be identified before nursing interventions are planned. After nursing interventions are implemented, the nurse will evaluate if the outcomes were met in the time frame indicated for that patient.
Outcome identification includes setting short- and long-term goals and then creating specific expected outcome statements for each nursing diagnosis.
Short-Term and Long-Term Goals
Nursing care should always be individualized and patient-centered. No two people are the same, and neither should nursing care plans be the same for two people. Goals and outcomes should be tailored specifically to each patient’s needs, values, and cultural beliefs. Patients and family members should be included in the goal-setting process when feasible. Involving patients and family members promotes awareness of identified needs, ensures realistic goals, and motivates their participation in the treatment plan to achieve the mutually agreed upon goals and live life to the fullest with their current condition.
The nursing care plan is a road map used to guide patient care so that all health care providers are moving toward the same patient goals. Goals are broad statements of purpose that describe the overall aim of care. Goals can be short- or long-term. The time frame for short- and long-term goals is dependent on the setting in which the care is provided. For example, in a critical care area, a short-term goal might be set to be achieved within an 8-hour nursing shift, and a long-term goal might be in 24 hours. In contrast, in an outpatient setting, a short-term goal might be set to be achieved within one month and a long-term goal might be within six months.
A nursing goal is the overall direction in which the patient must progress to improve the problem/nursing diagnosis and is often the opposite of the problem.
Example. Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. had a priority nursing diagnosis of Fluid Volume Excess. A broad goal would be, “ Ms. J. will achieve a state of fluid balance. ”
Expected Outcomes
Goals are broad, general statements, but outcomes are specific and measurable. Expected outcomes are statements of measurable action for the patient within a specific time frame that are responsive to nursing interventions. Nurses may create expected outcomes independently or refer to classification systems for assistance. Just as NANDA-I creates and revises standardized nursing diagnoses, a similar classification and standardization process exists for expected nursing outcomes. The Nursing Outcomes Classification (NOC) is a list of over 330 nursing outcomes designed to coordinate with established NANDA-I diagnoses. [ 3 ]
Patient-Centered
Outcome statements are always patient-centered. They should be developed in collaboration with the patient and individualized to meet a patient’s unique needs, values, and cultural beliefs. They should start with the phrase “The patient will…” Outcome statements should be directed at resolving the defining characteristics for that nursing diagnosis. Additionally, the outcome must be something the patient is willing to cooperate in achieving.
Outcome statements should contain five components easily remembered using the “SMART” mnemonic: [ 4 ]
- M easurable
- A ttainable/Action oriented
- R elevant/Realistic
See Figure 4.9 [ 5 ] for an image of the SMART components of outcome statements. Each of these components is further described in the following subsections.
SMART Components of Outcome Statements
Outcome statements should state precisely what is to be accomplished. See the following examples:
- Not specific: “The patient will increase the amount of exercise.”
- Specific: “The patient will participate in a bicycling exercise session daily for 30 minutes.”
Additionally, only one action should be included in each expected outcome. See the following examples:
- “The patient will walk 50 feet three times a day with standby assistance of one and will shower in the morning until discharge” is actually two goals written as one. The outcome of ambulation should be separate from showering for precise evaluation. For instance, the patient could shower but not ambulate, which would make this outcome statement very difficult to effectively evaluate.
- Suggested revision is to create two outcomes statements so each can be measured: The patient will walk 50 feet three times a day with standby assistance of one until discharge. The patient will shower every morning until discharge.
Measurable outcomes have numeric parameters or other concrete methods of judging whether the outcome was met. It is important to use objective data to measure outcomes. If terms like “acceptable” or “normal” are used in an outcome statement, it is difficult to determine whether the outcome is attained. Refer to Figure 4.10 [ 6 ] for examples of verbs that are measurable and not measurable in outcome statements.
Figure 4.10
Measurable Outcomes
See the following examples:
- Not measurable: “The patient will drink adequate fluid amounts every shift.”
- Measurable: “The patient will drink 24 ounces of fluids during every day shift (0600-1400).”
Action-Oriented and Attainable
Outcome statements should be written so that there is a clear action to be taken by the patient or significant others. This means that the outcome statement should include a verb. Refer to Figure 4.11 [ 7 ] for examples of action verbs.
Figure 4.11
Action Verbs
- Not action-oriented: “The patient will get increased physical activity.”
- Action-oriented: “The patient will list three types of aerobic activity that he would enjoy completing every week.”
Realistic and Relevant
Realistic outcomes consider the patient’s physical and mental condition; their cultural and spiritual values, beliefs, and preferences; and their socioeconomic status in terms of their ability to attain these outcomes. Consideration should be also given to disease processes and the effects of conditions such as pain and decreased mobility on the patient’s ability to reach expected outcomes. Other barriers to outcome attainment may be related to health literacy or lack of available resources. Outcomes should always be reevaluated and revised for attainability as needed. If an outcome is not attained, it is commonly because the original time frame was too ambitious or the outcome was not realistic for the patient.
- Not realistic: “The patient will jog one mile every day when starting the exercise program.”
- Realistic: “The patient will walk ½ mile three times a week for two weeks.”
Time Limited
Outcome statements should include a time frame for evaluation. The time frame depends on the intervention and the patient’s current condition. Some outcomes may need to be evaluated every shift, whereas other outcomes may be evaluated daily, weekly, or monthly. During the evaluation phase of the nursing process, the outcomes will be assessed according to the time frame specified for evaluation. If it has not been met, the nursing care plan should be revised.
- Not time limited: “The patient will stop smoking cigarettes.”
- Time limited: “The patient will complete the smoking cessation plan by December 12, 2021.”
In Scenario C in Box 4.3, Ms. J.’s priority nursing diagnosis statement was Fluid Volume Excess related to excess fluid intake as manifested by bilateral basilar crackles in the lungs, bilateral 2+ pitting edema of the ankles and feet, an increase weight of 10 pounds, and the patient reports, “My ankles are so swollen.” An example of an expected outcome meeting SMART criteria for Ms. J. is, “The patient will have clear bilateral lung sounds within the next 24 hours.”
4.6. PLANNING
Planning is the fourth step of the nursing process (and the fourth Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.” The RN develops an individualized, holistic, evidence-based plan in partnership with the health care consumer, family, significant others, and interprofessional team. Elements of the plan are prioritized. The plan is modified according to the ongoing assessment of the health care consumer’s response and other indicators. The plan is documented using standardized language or terminology. [ 1 ]
After expected outcomes are identified, the nurse begins planning nursing interventions to implement. Nursing interventions are evidence-based actions that the nurse performs to achieve patient outcomes. Just as a provider makes medical diagnoses and writes prescriptions to improve the patient’s medical condition, a nurse formulates nursing diagnoses and plans nursing interventions to resolve patient problems. Nursing interventions should focus on eliminating or reducing the related factors (etiology) of the nursing diagnoses when possible. [ 2 ] Nursing interventions, goals, and expected outcomes are written in the nursing care plan for continuity of care across shifts, nurses, and health professionals.
Planning Nursing Interventions
You might be asking yourself, “How do I know what evidence-based nursing interventions to include in the nursing care plan?” There are several sources that nurses and nursing students can use to select nursing interventions. Many agencies have care planning tools and references included in the electronic health record that are easily documented in the patient chart. Nurses can also refer to other care planning books our sources such as the Nursing Interventions Classification (NIC) system. Based on research and input from the nursing profession, NIC categorizes and describes nursing interventions that are constantly evaluated and updated. Interventions included in NIC are considered evidence-based nursing practices. The nurse is responsible for using clinical judgment to make decisions about which interventions are best suited to meet an individualized patient’s needs. [ 3 ]
Direct and Indirect Care
Nursing interventions are considered direct care or indirect care. Direct care refers to interventions that are carried out by having personal contact with patients. Examples of direct care interventions are wound care, repositioning, and ambulation. Indirect care interventions are performed when the nurse provides assistance in a setting other than with the patient. Examples of indirect care interventions are attending care conferences, documenting, and communicating about patient care with other providers.
Classification of Nursing Interventions
There are three types of nursing interventions: independent, dependent, and collaborative. (See Figure 4.12 [ 4 ] for an image of a nurse collaborating with the health care team when planning interventions.)
Figure 4.12
Collaborative nursing interventions, independent nursing interventions.
Any intervention that the nurse can independently provide without obtaining a prescription is considered an independent nursing intervention . An example of an independent nursing intervention is when the nurses monitor the patient’s 24-hour intake/output record for trends because of a risk for imbalanced fluid volume. Another example of independent nursing interventions is the therapeutic communication that a nurse uses to assist patients to cope with a new medical diagnosis.
Example. Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. was diagnosed with Fluid Volume Excess . An example of an evidence-based independent nursing intervention is, “The nurse will reposition the patient with dependent edema frequently, as appropriate.” [ 5 ] The nurse would individualize this evidence-based intervention to the patient and agency policy by stating, “The nurse will reposition the patient every 2 hours.”
Dependent Nursing Interventions
Dependent nursing interventions require a prescription before they can be performed. Prescriptions are orders, interventions, remedies, or treatments ordered or directed by an authorized primary health care provider. [ 6 ] A primary health care provider is a member of the health care team (usually a physician, advanced practice nurse, or physician’s assistant) who is licensed and authorized to formulate prescriptions on behalf of the client. For example, administering medication is a dependent nursing intervention. The nurse incorporates dependent interventions into the patient’s overall care plan by associating each intervention with the appropriate nursing diagnosis.
Example. Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. was diagnosed with Fluid Volume Excess . An example of a dependent nursing intervention is, “The nurse will administer scheduled diuretics as prescribed.”
Collaborative nursing interventions are actions that the nurse carries out in collaboration with other health team members, such as physicians, social workers, respiratory therapists, physical therapists, and occupational therapists. These actions are developed in consultation with other health care professionals and incorporate their professional viewpoint. [ 7 ]
Example. Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. was diagnosed with Fluid Volume Excess . An example of a collaborative nursing intervention is consulting with a respiratory therapist when the patient has deteriorating oxygen saturation levels. The respiratory therapist plans oxygen therapy and obtains a prescription from the provider. The nurse would document “ The nurse will manage oxygen therapy in collaboration with the respiratory therapist ” in the care plan.
Individualization of Interventions
It is vital for the planned interventions to be individualized to the patient to be successful. For example, adding prune juice to the breakfast meal of a patient with constipation will only work if the patient likes to drink the prune juice. If the patient does not like prune juice, then this intervention should not be included in the care plan. Collaboration with the patient, family members, significant others, and the interprofessional team is essential for selecting effective interventions. The number of interventions included in a nursing care plan is not a hard and fast rule, but enough quality, individualized interventions should be planned to meet the identified outcomes for that patient.
Creating Nursing Care Plans
Nursing care plans are created by registered nurses (RNs). Documentation of individualized nursing care plans are legally required in long-term care facilities by the Centers for Medicare and Medicaid Services (CMS) and in hospitals by The Joint Commission. CMS guidelines state, “Residents and their representative(s) must be afforded the opportunity to participate in their care planning process and to be included in decisions and changes in care, treatment, and/or interventions. This applies both to initial decisions about care and treatment, as well as the refusal of care or treatment. Facility staff must support and encourage participation in the care planning process. This may include ensuring that residents, families, or representatives understand the comprehensive care planning process, holding care planning meetings at the time of day when a resident is functioning best and patient representatives can be present, providing sufficient notice in advance of the meeting, scheduling these meetings to accommodate a resident’s representative (such as conducting the meeting in-person, via a conference call, or video conferencing), and planning enough time for information exchange and decision-making. A resident has the right to select or refuse specific treatment options before the care plan is instituted.” [ 8 ] The Joint Commission conceptualizes the care planning process as the structuring framework for coordinating communication that will result in safe and effective care. [ 9 ]
Many facilities have established standardized nursing care plans with lists of possible interventions that can be customized for each specific patient. Other facilities require the nurse to develop each care plan independently. Whatever the format, nursing care plans should be individualized to meet the specific and unique needs of each patient. See Figure 4.13 [ 10 ] for an image of a standardized care plan.
Figure 4.13
Standardized Care Plan
Nursing care plans created in nursing school can also be in various formats such as concept maps or tables. Some are fun and creative, while others are more formal. Appendix B contains a template that can be used for creating nursing care plans.
4.7. IMPLEMENTATION OF INTERVENTIONS
Implementation is the fifth step of the nursing process (and the fifth Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse implements the identified plan.” The RN may delegate planned interventions after considering the circumstance, person, task, communication, supervision, and evaluation, as well as the state Nurse Practice Act, federal regulation, and agency policy. [ 1 ]
Implementation of interventions requires the RN to use critical thinking and clinical judgment. After the initial plan of care is developed, continual reassessment of the patient is necessary to detect any changes in the patient’s condition requiring modification of the plan. The need for continual patient reassessment underscores the dynamic nature of the nursing process and is crucial to providing safe care.
During the implementation phase of the nursing process, the nurse prioritizes planned interventions, assesses patient safety while implementing interventions, delegates interventions as appropriate, and documents interventions performed.
Prioritizing Implementation of Interventions
Prioritizing implementation of interventions follows a similar method as to prioritizing nursing diagnoses. Maslow’s Hierarchy of Needs and the ABCs of airway, breathing, and circulation are used to establish top priority interventions. When possible, least invasive actions are usually preferred due to the risk of injury from invasive options. Read more about methods for prioritization under the “ Diagnosis ” subsection of this chapter.
The potential impact on future events, especially if a task is not completed at a certain time, is also included when prioritizing nursing interventions. For example, if a patient is scheduled to undergo a surgical procedure later in the day, the nurse prioritizes initiating a NPO (nothing by mouth) prescription prior to completing pre-op patient education about the procedure. The rationale for this decision is that if the patient ate food or drank water, the surgery time would be delayed. Knowing and understanding the patient’s purpose for care, current situation, and expected outcomes are necessary to accurately prioritize interventions.
Patient Safety
It is essential to consider patient safety when implementing interventions. At times, patients may experience a change in condition that makes a planned nursing intervention or provider prescription no longer safe to implement. For example, an established nursing care plan for a patient states, “The nurse will ambulate the patient 100 feet three times daily.” However, during assessment this morning, the patient reports feeling dizzy today, and their blood pressure is 90/60. Using critical thinking and clinical judgment, the nurse decides to not implement the planned intervention of ambulating the patient. This decision and supporting assessment findings should be documented in the patient’s chart and also communicated during the shift handoff report, along with appropriate notification of the provider of the patient’s change in condition.
Implementing interventions goes far beyond implementing provider prescriptions and completing tasks identified on the nursing care plan and must focus on patient safety. As front-line providers, nurses are in the position to stop errors before they reach the patient. [ 2 ]
In 2000 the Institute of Medicine (IOM) issued a groundbreaking report titled To Err Is Human: Building a Safer Health System . The report stated that as many as 98,000 people die in U.S. hospitals each year as a result of preventable medical errors. To Err Is Human broke the silence that previously surrounded the consequences of medical errors and set a national agenda for reducing medical errors and improving patient safety through the design of a safer health system. [ 3 ] In 2007 the IOM published a follow-up report titled Preventing Medication Errors and reported that more than 1.5 million Americans are injured every year in American hospitals, and the average hospitalized patient experiences at least one medication error each day. This report emphasized actions that health care systems could take to improve medication safety. [ 4 ]
Read additional information about specific actions that nurses can take to prevent medication errors; go to the “Preventing Medication Errors” section of the “ Legal/Ethical” chapter of the Open RN Nursing Pharmacology textbook.
In an article released by the Robert Wood Johnson Foundation, errors involving nurses that endanger patient safety cover broad territory. This territory spans “wrong site, wrong patient, wrong procedure” errors, medication mistakes, failures to follow procedures that prevent central line bloodstream and other infections, errors that allow unsupervised patients to fall, and more. Some errors can be traced to shifts that are too long that leave nurses fatigued, some result from flawed systems that do not allow for adequate safety checks, and others are caused by interruptions to nurses while they are trying to administer medications or provide other care. [ 5 ]
The Quality and Safety Education for Nurses (QSEN) project began in 2005 to assist in preparing future nurses to continuously improve the quality and safety of the health care systems in which they work. The vision of the QSEN project is to “inspire health care professionals to put quality and safety as core values to guide their work.” [ 6 ] Nurses and nursing students are expected to participate in quality improvement (QI) initiatives by identifying gaps where change is needed and assisting in implementing initiatives to resolve these gaps. Quality improvement is defined as, “The combined and unceasing efforts of everyone – health care professionals, patients and their families, researchers, payers, planners and educators – to make the changes that will lead to better patient outcomes (health), better system performance (care), and better professional development (learning).” [ 7 ]
Delegation of Interventions
While implementing interventions, RNs may elect to delegate nursing tasks. Delegation is defined by the American Nurses Association as, “The assignment of the performance of activities or tasks related to patient care to unlicensed assistive personnel or licensed practical nurses (LPNs) while retaining accountability for the outcome.” [ 8 ] RNs are accountable for determining the appropriateness of the delegated task according to condition of the patient and the circumstance; the communication provided to an appropriately trained LPN or UAP; the level of supervision provided; and the evaluation and documentation of the task completed. The RN must also be aware of the state Nurse Practice Act, federal regulations, and agency policy before delegating. The RN cannot delegate responsibilities requiring clinical judgment. [ 9 ] See the following box for information regarding legal requirements associated with delegation according to the Wisconsin Nurse Practice Act.
Delegation According to the Wisconsin Nurse Practice Act
During the supervision and direction of delegated acts a Registered Nurse shall do all of the following:
Delegate tasks commensurate with educational preparation and demonstrated abilities of the person supervised.
Provide direction and assistance to those supervised.
Observe and monitor the activities of those supervised.
Evaluate the effectiveness of acts performed under supervision. [ 10 ]
The standard of practice for Licensed Practical Nurses in Wisconsin states, “In the performance of acts in basic patient situations, the LPN. shall, under the general supervision of an RN or the direction of a provider:
Accept only patient care assignments which the LPN is competent to perform.
Provide basic nursing care. Basic nursing care is defined as care that can be performed following a defined nursing procedure with minimal modification in which the responses of the patient to the nursing care are predictable.
Record nursing care given and report to the appropriate person changes in the condition of a patient.
Consult with a provider in cases where an LPN knows or should know a delegated act may harm a patient.
Perform the following other acts when applicable:
Assist with the collection of data.
Assist with the development and revision of a nursing care plan.
Reinforce the teaching provided by an RN provider and provide basic health care instruction.
Participate with other health team members in meeting basic patient needs.” [ 11 ]
Read additional details about the scope of practice of registered nurses (RNs) and licensed practical nurses (LPNs) in Wisconsin’s Nurse Practice Act in Chapter N 6 Standards of Practice .
Read more about the American Nurses Association’s Principles of Delegation.
Table 4.7 outlines general guidelines for delegating nursing tasks in the state of Wisconsin according to the role of the health care team member.
General Guidelines for Delegating Nursing Tasks
Documentation of Interventions
As interventions are performed, they must be documented in the patient’s record in a timely manner. As previously discussed in the “Ethical and Legal Issues” subsection of the “ Basic Concepts ” section, lack of documentation is considered a failure to communicate and a basis for legal action. A basic rule of thumb is if an intervention is not documented, it is considered not done in a court of law. It is also important to document administration of medication and other interventions in a timely manner to prevent errors that can occur due to delayed documentation time.
Coordination of Care and Health Teaching/Health Promotion
ANA’s Standard of Professional Practice for Implementation also includes the standards 5A Coordination of Care and 5B Health Teaching and Health Promotion . [ 12 ] Coordination of Care includes competencies such as organizing the components of the plan, engaging the patient in self-care to achieve goals, and advocating for the delivery of dignified and holistic care by the interprofessional team. Health Teaching and Health Promotion is defined as, “Employing strategies to teach and promote health and wellness.” [ 13 ] Patient education is an important component of nursing care and should be included during every patient encounter. For example, patient education may include teaching about side effects while administering medications or teaching patients how to self-manage their conditions at home.
Refer to Scenario C in the “Assessment” section of this chapter. The nurse implemented the nursing care plan documented in Appendix C. Interventions related to breathing were prioritized. Administration of the diuretic medication was completed first, and lung sounds were monitored frequently for the remainder of the shift. Weighing the patient before breakfast was delegated to the CNA. The patient was educated about her medications and methods to use to reduce peripheral edema at home. All interventions were documented in the electronic medical record (EMR).
4.8. EVALUATION
Evaluation is the sixth step of the nursing process (and the sixth Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.” [ 1 ] Both the patient status and the effectiveness of the nursing care must be continuously evaluated and the care plan modified as needed. [ 2 ]
Evaluation focuses on the effectiveness of the nursing interventions by reviewing the expected outcomes to determine if they were met by the time frames indicated. During the evaluation phase, nurses use critical thinking to analyze reassessment data and determine if a patient’s expected outcomes have been met, partially met, or not met by the time frames established. If outcomes are not met or only partially met by the time frame indicated, the care plan should be revised. Reassessment should occur every time the nurse interacts with a patient, discusses the care plan with others on the interprofessional team, or reviews updated laboratory or diagnostic test results. Nursing care plans should be updated as higher priority goals emerge. The results of the evaluation must be documented in the patient’s medical record.
Ideally, when the planned interventions are implemented, the patient will respond positively and the expected outcomes are achieved. However, when interventions do not assist in progressing the patient toward the expected outcomes, the nursing care plan must be revised to more effectively address the needs of the patient. These questions can be used as a guide when revising the nursing care plan:
- Did anything unanticipated occur?
- Has the patient’s condition changed?
- Were the expected outcomes and their time frames realistic?
- Are the nursing diagnoses accurate for this patient at this time?
- Are the planned interventions appropriately focused on supporting outcome attainment?
- What barriers were experienced as interventions were implemented?
- Does ongoing assessment data indicate the need to revise diagnoses, outcome criteria, planned interventions, or implementation strategies?
- Are different interventions required?
Refer to Scenario C in the “Assessment” section of this chapter and Appendix C . The nurse evaluates the patient’s progress toward achieving the expected outcomes.
For the nursing diagnosis Fluid Volume Excess , the nurse evaluated the four expected outcomes to determine if they were met during the time frames indicated:
The patient will report decreased dyspnea within the next 8 hours.
The patient will have clear lung sounds within the next 24 hours.
The patient will have decreased edema within the next 24 hours.
The patient’s weight will return to baseline by discharge.
Evaluation of the patient condition on Day 1 included the following data: “ The patient reported decreased shortness of breath, and there were no longer crackles in the lower bases of the lungs. Weight decreased by 1 kg, but 2+ edema continued in ankles and calves .” Based on this data, the nurse evaluated the expected outcomes as “ Partially Met ” and revised the care plan with two new interventions:
Request prescription for TED hose from provider.
Elevate patient’s legs when sitting in chair.
For the second nursing diagnosis, Risk for Falls , the nurse evaluated the outcome criteria as “ Met ” based on the evaluation, “ The patient verbalizes understanding and is appropriately calling for assistance when getting out of bed. No falls have occurred. ”
The nurse will continue to reassess the patient’s progress according to the care plan during hospitalization and make revisions to the care plan as needed. Evaluation of the care plan is documented in the patient’s medical record.
4.9. SUMMARY OF THE NURSING PROCESS
You have now learned how to perform each step of the nursing process according to the ANA Standards of Professional Nursing Practice. Critical thinking, clinical reasoning, and clinical judgment are used when assessing the patient, creating a nursing care plan, and implementing interventions. Frequent reassessment, with revisions to the care plan as needed, is important to help the patient achieve expected outcomes. Throughout the entire nursing process, the patient always remains the cornerstone of nursing care. Providing individualized, patient-centered care and evaluating whether that care has been successful in achieving patient outcomes are essential for providing safe, professional nursing practice.
Video Review of Creating a Sample Care Plan [ 1 ]
4.10. LEARNING ACTIVITIES
Learning activities.
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Instructions: Apply what you’ve learned in this chapter by creating a nursing care plan using the following scenario. Use the template in Appendix B as a guide.
The client, Mark S., is a 57-year-old male who was admitted to the hospital with “severe” abdominal pain that was unable to be managed in the Emergency Department. The physician has informed Mark that he will need to undergo some diagnostic tests. The tests are scheduled for the morning.
After receiving the news about his condition and the need for diagnostic tests, Mark begins to pace the floor. He continues to pace constantly. He keeps asking the nurse the same question (“How long will the tests take?”) about his tests over and over again. The patient also remarked, “I’m so uptight I will never be able to sleep tonight.” The nurse observes that the client avoids eye contact during their interactions and that he continually fidgets with the call light. His eyes keep darting around the room. He appears tense and has a strained expression on his face. He states, “My mouth is so dry.” The nurse observes his vital signs to be: T 98, P 104, R 30, BP 180/96. The nurse notes that his skin feels sweaty (diaphoretic) and cool to the touch.
Critical Thinking Activity:
Group (cluster) the subjective and objective data.
Create a problem-focused nursing diagnosis (hypothesis).
Develop a broad goal and then identify an expected outcome in “SMART” format.
Outline three interventions for the nursing diagnosis to meet the goal. Cite an evidence-based source.
Imagine that you implemented the interventions that you identified. Evaluate the degree to which the expected outcome was achieved: Met – Partially Met – Not Met.

- IV GLOSSARY
The act or process of pleading for, supporting, or recommending a cause or course of action. [ 1 ]
Unconditionally acceptance of the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care. [ 2 ]
Groups of people who share a characteristic that causes each member to be susceptible to a particular human response, such as demographics, health/family history, stages of growth/development, or exposure to certain events/experiences. [ 3 ]
Medical diagnoses, injuries, procedures, medical devices, or pharmacological agents. These conditions are not independently modifiable by the nurse, but support accuracy in nursing diagnosis. [ 4 ]
Care that can be performed following a defined nursing procedure with minimal modification in which the responses of the patient to the nursing care are predictable. [ 5 ]
A relationship described as one in which the whole person is assessed while balancing the vulnerability and dignity of the patient and family. [ 6 ]
Individual, family, or group, which includes significant others and populations. [ 7 ]
The observed outcome of critical thinking and decision-making. It is an iterative process that uses nursing knowledge to observe and access presenting situations, identify a prioritized client concern, and generate the best possible evidence-based solutions in order to deliver safe client care. [ 8 ]
A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions. [ 9 ]
Grouping data into similar domains or patterns.
Nursing interventions that require cooperation among health care professionals and unlicensed assistive personnel (UAP).
While implementing interventions during the nursing process, includes components such as organizing the components of the plan with input from the health care consumer, engaging the patient in self-care to achieve goals, and advocating for the delivery of dignified and person-centered care by the interprofessional team. [ 10 ]
Reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow. [ 11 ]
Subjective or objective data that gives the nurse a hint or indication of a potential problem, process, or disorder.
“Top-down thinking” or moving from the general to the specific. Deductive reasoning relies on a general statement or hypothesis—sometimes called a premise or standard—that is held to be true. The premise is used to reach a specific, logical conclusion.
Observable cues/inferences that cluster as manifestations of a problem-focused, health-promotion diagnosis, or syndrome. This does not only imply those things that the nurse can see, but also things that are seen, heard (e.g., the patient/family tells us), touched, or smelled. [ 12 ]
The assignment of the performance of activities or tasks related to patient care to unlicensed assistive personnel while retaining accountability for the outcome. [ 13 ]
Interventions that require a prescription from a physician, advanced practice nurse, or physician’s assistant.
Interventions that are carried out by having personal contact with a patient.
An electronic version of the patient’s medical record.
A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and patient, family, group, community, and population preferences and values. [ 14 ]
Statements of measurable action for the patient within a specific time frame and in response to nursing interventions. “SMART” outcome statements are specific, measurable, action-oriented, realistic, and include a time frame.
An evidence-based assessment framework for identifying patient problems and risks during the assessment phase of the nursing process.
A judgment formed from a set of facts, cues, and observations.
Broad statements of purpose that describe the aim of nursing care.
Employing strategies to teach and promote health and wellness. [ 15 ]
Any intervention that the nurse can provide without obtaining a prescription or consulting anyone else.
Interventions performed by the nurse in a setting other than directly with the patient. An example of indirect care is creating a nursing care plan.
A type of reasoning that involves forming generalizations based on specific incidents.
Interpretations or conclusions based on cues, personal experiences, preferences, or generalizations.
Nurses who have had specific training and passed a licensing exam. The training is generally less than that of a Registered Nurse. The scope of practice of an LPN/LVN is determined by the facility and the state’s Nurse Practice Act.
A disease or illness diagnosed by a physician or advanced health care provider such as a nurse practitioner or physician’s assistant. Medical diagnoses are a result of clustering signs and symptoms to determine what is medically affecting an individual.
Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in the recognition of the connection of all humanity. [ 16 ]
Specific documentation of the planning and delivery of nursing care that is required by The Joint Commission.
A systematic approach to patient-centered care with steps including assessment, diagnosis, outcome identification, planning, implementation, and evaluation; otherwise known by the mnemonic “ADOPIE.”
Data that the nurse can see, touch, smell, or hear or is reproducible such as vital signs. Laboratory and diagnostic results are also considered objective data.
A measurable behavior demonstrated by the patient that is responsive to nursing interventions. [ 17 ]
The format of a nursing diagnosis statement that includes:
Problem (P) – statement of the patient problem (i.e., the nursing diagnosis)
Etiology (E) – related factors (etiology) contributing to the cause of the nursing diagnosis
Signs and Symptoms (S) – defining characteristics manifested by the patient of that nursing diagnosis
Orders, interventions, remedies, or treatments ordered or directed by an authorized primary health care provider. [ 18 ]
Information collected from the patient.
Member of the health care team (usually a medical physician, nurse practitioner, etc.) licensed and authorized to formulate prescriptions on behalf of the client. [ 19 ]
The skillful process of deciding which actions to complete first, second, or third for optimal patient outcomes and to improve patient safety.
The “combined and unceasing efforts of everyone — health care professionals, patients and their families, researchers, payers, planners, and educators — to make the changes that will lead to better patient outcomes (health), better system performance (care), and better professional development (learning).” [ 20 ]
Developing a relationship of mutual trust and understanding.
A nurse who has had a designated amount of education and training in nursing and is licensed by a state Board of Nursing.
The underlying cause (etiology) of a nursing diagnosis when creating a PES statement.
Patients have the right to determine what will be done with and to their own person.
Principles and procedures in the discovery of knowledge involving the recognition and formulation of a problem, the collection of data, and the formulation and testing of a hypothesis.
Information collected from sources other than the patient.
Data that the patient or family reports or data that the nurse makes as an inference, conclusion, or assumption, such as “The patient appears anxious.”
Any unlicensed personnel trained to function in a supportive role, regardless of title, to whom a nursing responsibility may be delegated. [ 21 ]
Obtaining Subjective Data in a Care Relationship
Licensed under a Creative Commons Attribution 4.0 International License. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/ .
- Cite this Page Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Fundamentals [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2021. Chapter 4 Nursing Process.
- PDF version of this title (216M)
In this Page
- NURSING PROCESS INTRODUCTION
- BASIC CONCEPTS
- OUTCOME IDENTIFICATION
- IMPLEMENTATION OF INTERVENTIONS
- SUMMARY OF THE NURSING PROCESS
- LEARNING ACTIVITIES
Other titles in this collection
- Open RN OER Textbooks
Related Items in Bookshelf
- All Textbooks
Bulk Download
- Bulk download content from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Chapter 4 Nursing Process - Nursing Fundamentals Chapter 4 Nursing Process - Nursing Fundamentals
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
MockQuestions
Situational Nursing Mock Interview
To help you prepare for your nursing interview, here are 50 situational nursing interview questions and answer examples.
Situational Nursing was updated by Krista Wenz on May 30th, 2023. Learn more here.
Question 1 of 50
How do you handle being asked to do a nursing task you've never completed before?
How to Answer
1st answer example, 2nd answer example.
Most situational interview questions are best answered using the STAR method which involves thinking about the situation, task, action and result and providing solid and thorough answers. This is not the time to say that you would jump in with both feet. The interviewer is not looking for someone who just jumps when someone says jump, but someone willing to jump with confidence and competence. Your job is to provide an answer that illustrates this difference.
"I really want to be liked and be a contributing member of the team, but I always stop and do a check-in before enthusiastically saying I'll do something I'm not sure about! I know the basics of nursing skills, so if I can look it up in the policy and procedure manual, such as a simple but different dressing change, I am able to do that independently. If it's totally novel, I will ask for supervision when first performing it so that I always work within the scope of my nursing practice."
"If I'm asked to complete a nursing task I've never done before, I will use our hospital's intranet site to read about the procedure and/or watch a video about completing the procedure. If I feel comfortable doing the task after looking up the instructions, I will do so. If the task is complex or very different from something I've done before, and I don't feel competent to do it without supervision, I will ask for help. I would ask either another floor nurse or the charge nurse to review the steps with me and supervise me while I perform the task. That way, I can make sure that I'm learning about a task that I am responsible for completing while ensuring that my patient receives safe care."
Next Question
50 Situational Nursing Interview Questions & Answers
Below is a list of our Situational Nursing interview questions. Click on any interview question to view our answer advice and answer examples. You may view 15 answer examples before our paywall loads. Afterwards, you'll be asked to upgrade to view the rest of our answers.
Table of Contents
- 1. Adaptability Questions
- 2. Communication Questions
- 3. Competency Questions
- 4. Conflict Questions
- 5. Creative Thinking Questions
- 6. Critical Thinking Questions
- 7. Customer Service Questions
- 8. Diligence Questions
- 9. Discovery Questions
- 10. Leadership Questions
- 11. Management Questions
- 12. Operational Questions
- 13. Performance Based Questions
- 14. Problem Solving Questions
- 15. Role-Specific Questions
- 16. Scenario Based Questions
- 17. Situational Questions
- 18. Teamwork Questions
- 19. Tough Questions
Situational questions are asked so the interviewer can gain insight into your thought process, how you problem-solve, and how you communicate in the workplace. Situational nursing questions can include inquiries about drug dosages, procedures, or specific signs and symptoms of a patient and how you would proceed. Additionally, interviewers can ask how you would respond when faced with an ethical dilemma, a challenging colleague, or when abruptly put into a leadership role. While these questions can be challenging, there are a few ways to prepare before your interview. First, think about your interview as having a chat with a friend. They ask you what you would do in a particular situation, and you respond using your knowledge and experience. Additional tips include the following: 1. Make sure you understand the question. If you are unsure how to respond, ask the interviewer to clarify. 2. Use your critical-thinking skills if asked about a situation you have not encountered in your career. 3. Use real-life examples as often as possible. 4. Practice answering these types of questions with a friend or colleague. 5. Be honest with the interviewer. If you are unsure of the answer, let the interviewer know that while you do not know the answer, you will find it after the interview. If you would like more practice questions to review before your interview, we have many great resources at Mockquestions. Here are 50 General Nursing Interview Questions that will help you prepare for many different kinds of nursing interviews. We have specific Behavioral Nursing Interview Questions as well! For more modern virtual nursing interviews, we have HireVue Nursing Interview Questions . Additionally, we have interview questions for a Registered Nurse that will help you better prepare for your interview than just our general nursing questions. Remember to approach your interview as if you are having a professional discussion with a friend. If you have successfully completed nursing school, you can ace your interview! Best of luck!
Adaptability
1. How do you handle being asked to do a nursing task you've never completed before?
Written by Dianne Barnard on March 9th, 2021
Written by Kate Buckley on January 10th, 2023
Communication
2. You are talking with a patient during rounds, and the patient tells you she does not understand what the doctors tell her and she is unsure of what is going on with her health. Tell me how you respond to the patient.
Unfortunately, these types of situations are very common in the healthcare system, as patients are often confused or misinformed about their health. This is particularly true for elderly patients and/or patients without someone present to advocate for them. In this situation, the nurse should take time to help the patient understand what is going on with her health. The interviewer is asking this question to determine if the candidate would take initiative to help the patient; and to effectively answer this question, the candidate should indicate they would explain the medical situation to the patient in layman's terms. A more successful answer to this question would include a specific example from the nurse's career where they helped clarify a diagnosis, procedure, or other medical-related situation when a patient was confused.
Written by Kelly Burlison on June 3rd, 2019
"This type of situation has to be so frightening for a patient, and unfortunately, it happens so often. I would take time to explain the patient's medical condition to them at a level in which they could understand, and I would not leave until I was sure they understood. I have dealt with this many times in my nursing career, but one time in particular sticks out to me. I was caring for a patient who had been admitted after a car accident, and after she had a CT scan on her head, a mass was found on her pituitary gland. The doctors did not think the mass was cancerous, and the patient was told it was likely benign; but unfortunately, she didn't know the meaning of benign. Later, when I went to check on the patient, she was devastated and thought she had brain cancer. Luckily, I was able to help explain the situation to her, just like I would do in the situation with the patient you described to me."
"In the hospital, it can be common for patients to feel confused and scared about their medical condition. Patients may be dealing with pain or poor sleep, which can make it difficult to focus on information from doctors or others in the hospital. Also, regardless of patients' education or socioeconomic status, we can't assume that we know a patient's 'health literacy,' which is their ability to understand health and medical information. So, I have encountered scenarios a lot like this at the bedside. In this case, I would stay in the patient's room and pull up her most recent clinical notes from her primary team and consulting teams. I would explain what their assessments are in simple terms, avoiding healthcare jargon. I would ask the patient if she now feels that she understands her condition and plan. In most cases, just taking the time to explain things in clear terms relieves much of the patient's anxiety."
Anonymous Interview Answers with Professional Feedback
Anonymous Answer

Cindy's Feedback
3. How would you explain a complex task to someone using verbal instructions?
Teaching patients in a way they can understand is an integral part of nursing. Healthcare is increasingly complex, so it makes sense that the instructions can be, as well. This question provides a chance to showcase your talent to take a complicated idea and explain it without losing the integrity of dumbing it down.
"I read once that most newspapers are written at a 5th grade level so that most people can understand the message. I think that today we are inundated with verbal messages and written messages, so what we choose to say should be prime real estate. That means no filler or fluff words for me, and to speak in a way that the patient or family can understand. Nurses are so used to throwing big words and acronyms around, and personally I am mindful not to do that. I break the information down into bite sized pieces and frequently check in with the person to see if they are understanding. I ask them to repeat back what I explained to them. I also watch them closely for non-verbal signs of confusion. I always feel so good when the patient is able to understand my instructions right away!"
"Because we can't know always know a patient's health literacy level, it's important to try to explain concepts about a patient's care in a way that anyone can understand. When I have to explain a complex task, such as how to check your own blood glucose, verbally only, I make sure to use simple terms and avoid healthcare jargon. I 'chunk' the main points so that I'm not explaining too many concepts at once. I speak slowly. And I ask the patient to repeat back the instructions to me, so I can check for understanding."
4. You were recently transferred to another unit and notice a fellow nurse consistently displaying incompetency in their work. How would you proceed?
The interviewer wants to gauge your level of professionalism and ability to handle difficult situations in the workplace. It's essential to approach this question with tact and diplomacy, as you don't want to come across as overly critical or negative toward your colleagues. Instead, focus on how you would approach the situation in a constructive and positive manner, such as subtly offering to help the coworker improve their skills or suggesting additional training opportunities to a supervisor. Ultimately, the goal is to demonstrate your ability to work collaboratively and supportively with your team, even in challenging circumstances. However, while you want to display that you can work well with others, you also want the interviewer to understand that the patient's safety is of utmost importance. If your colleague is incompetent to the level that it compromises patient care, you want to quickly bring it to the attention of a charge nurse.
Written by Krista Wenz on May 29th, 2023
"If I encountered a fellow nurse who I believed was struggling with their duties, I would approach the situation with empathy and understanding. I would first try to understand the root cause of their incompetence - whether it be a lack of training, personal issues, or being overwhelmed. Once I understand the situation better, I would offer my support and assistance in any way I can. This could include providing additional training, offering to help with their workload, or simply being a listening ear if they need to talk. It is essential to prioritize patient safety above all else. If a fellow nurse cannot provide safe and effective care, action must be taken to address the issue. If, after offering my support, I still believe their incompetence is putting patients at risk, I would bring my concerns to a supervisor or manager. Ultimately, my goal would be to approach the situation with kindness and empathy while prioritizing our patients' safety and well-being."
"If I recently transferred to another unit and encountered a coworker exhibiting incompetence, I would first try to assess the situation and determine the extent of their shortcomings. Depending on the severity of the issue, I might consider discussing the matter with my supervisor or seeking guidance from a more experienced colleague. However, I would always approach the situation with tact and sensitivity, recognizing that everyone has strengths and weaknesses and that we all have the potential to learn and improve. My goal would be to ensure the highest standards of patient care are being met and that my colleague is given the resources and support they need to succeed."
5. A coworker left her computer open with sensitive information on the screen. You are the only one in the nurses' station. How would you address this with her?
Patient confidentiality must be honored, and leaving a computer open even to run to the bathroom for a minute risks a serious breach of patient confidentiality. Even though you are the only person in the room, you should not have access to patient information that you have no need to know. Even if you wouldn't say a word to anyone and you are a professional nurse with integrity, you should not be able to see possible protected information on a patient that you are not personally taking care of. Leaving a computer wide open is a serious risk to confidentiality. If you see this, you could gently close the computer so that the screen is not visible and discuss the seriousness of this when your coworker returns. You must protect your license and you should report to supervision. It's uncomfortable to do so, but a nurse always takes the action that protects and advocates for the patient.
"I would immediately close or cover the computer. I would not look at the information, of course. If I wasn't sure where the coworker was or when he or she left, I would be compelled to report it to supervision because someone could have accessed the information. It's a tough call and may cause some coworker tension, but as a nurse, I must do what is best for my nursing license and the patient, and that is to protect the confidentiality of the patient."
"I would lock my coworker's computer without looking at anything on the screen and then let her know that I did so. If I knew for sure that no one looked at her computer screen while she was away, then I would remind her of the importance of locking her computer when she steps away. If I couldn't verify that no one had access to the sensitive information, I would have to let my supervisor know what happened. Potential violations of patient privacy are very serious."
6. Give an example of how you may connect and find common ground with a patient to gain understanding.
All patients are different and come from different backgrounds and life experiences. Sometimes, the patient will have biases and reject you as a competent individual. Learning how to connect and find common ground with a patient quickly can improve patient outcomes. There is always something that you can find in common with someone. It could be the weather, good or bad, a comment on a crossword they are completing, admiration for their turquoise necklace, anything that is authentic and sincere to start to build a bridge or connection. It doesn't have to be a colossal sharing of souls, but just looking quickly for similarities instead of differences can have real impact. Take the time to learn conversational techniques that can elicit conversation and build rapport.
"I try to establish conversational rapport with each patient and humanize our interaction a little bit. I want to be seen as a professional and competent nurse, but also as a warm and caring human being. I don't think idle chitchat is helpful overall, but I do believe an authentic comment about a picture of their dog or maybe a sweater they are wearing can leapfrog into more personalized conversations. I think that it makes people feel seen by the nurse and that helps."
"There are so many ways to connect with a patient during my shift. I think it always starts with identifying myself and my role. It sounds simple, but I always say a variation of 'Good morning, I'm Kate and I'll be your nurse until 7 p.m. today' when I first meet a patient. Over the years, many patients have told me that they feel frustrated or confused when people enter their rooms and just start talking without identifying themselves. Identifying myself to the patient in a friendly way helps to establish trust right away. After that, I may ask them about any drawings done by kids that I see in their room, the sports team they're watching on TV, the sodoku puzzle they're working on, or whatever type of Indiana weather we may be having. Talking about everyday things can help us develop a rapport that will be useful as we need to talk about medications and other aspects of treatment later."

Stephanie's Feedback
7. How do you handle difficult family members who disagree with the care that the patient agreed to?
Patient families can be challenging, and they do not always agree with the patient's decision. Sometimes they will pull you aside and tell you their opinion. As long as the patient is competent to make their own decisions, the best way to deal with these situations is to tell the family that they really need to talk with the patient. You should not be talking about the patient's condition when they are not present, anyway. Remember your license and advocate for your patient's rights.
"I would acknowledge that I understand they want the best for their family member, but explain that I cannot discuss the patient's care with them and that the patient has the right to make their own decision. I would encourage them to discuss their concerns with the patient directly and perhaps ask for a shared meeting with the doctor so their concerns could be addressed. I would definitely report the interaction to my nursing supervisor."
"When a patient is a competent adult who can make their own healthcare decision, I will respectfully direct the patient's family member back to the patient. I will remind the family member that I must respect the patient's privacy. If the patient agrees, I can call the doctor and ask the doctor to come to the patient's room and answer the family member's questions with the patient present."
8. You are caring for a young patient who is being discharged with a prescription for an inhaler. Upon asking the patient if he knows how to use the inhaler, he says, "Yes, I do." Tell me how you proceed.
Although most medications are dispensed with administration instructions at the pharmacy, many patients do not understand how to administer to themselves which results in their misuse. For medications such as beta agonists or corticosteroids which are administered via inhaler, misusing the inhalant device could mean the patient is not getting enough medication to help manage their condition. This is common for all medications which is why it is important for nurses to ensure patients understand how to properly take their medications before discharge. The interviewer is asking this question to determine if the candidate would ensure the understands how to use the inhaler before discharging him, rather than simply taking the patient's word for it. To effectively answer this question, the candidate should describe, in detail, how they would verify that the patient understands how to use the inhaler. A more successful answer to this question would include a specific example from the candidate's nursing career where they helped educate a patient on their medication regimen before discharge or how they developed patient education protocols or materials for their unit or organization.
"Even if the patient was adamant that he knew how to use the inhaler, I would get him to demonstrate how he uses an inhaler, either by using a teaching tool or by simply using an unrelated object to mock up the situation. Inhalers are more difficult to use than most people realize, and so many patients make mistakes when administering their inhaled medications to themselves. But this isn't only limited to inhaled medications, I always make sure my patients understand their medication regimen, and after I go over it with them, I have them demonstrate it to me or repeat it back to me, to ensure they understand. This is something I have always done in my nursing career and will continue to do so before I discharge my patients."
"Even if a patient assures me that he knows how to use his inhaler, I will ask him to demonstrate or explain its use to me. If we have a dose of his inhaler due soon, I will verbally review the steps of using his inhaler, and then I will ask him to show me using it. If he won't be due for a dose of his inhaler before discharge time, I will use the teach-back method, in which I will ask him to verbally 'teach me' to use his inhaler. It's important that patients can administer their medications to themselves upon discharge, and I always make sure to review patients' medications with them and check for understanding before discharge. I had a similar scenario with a patient who was being discharged with a new insulin pen. The patient told me he understood how to load the needle onto the pen, but when I asked him to demonstrate, he wasn't able to do it. We practiced a few times to make sure he understood the entire process, and he then was able to put the pen and needle together prior to discharge."

Chad's Feedback
9. How do you handle situations in which you disagree with a doctor's orders?
Nurses follow doctor's orders, but sometimes there are orders that a nurse feels are not in the patient's best interest. For example, if the doctor orders an antibiotic that the patient remembers she is allergic to, then it's easy for the nurse to tell the doctor that a different alternative is needed. But sometimes, the nurse disagrees with the validity of treatment that the doctor and patient agreed on. It's always helpful to say your dissension for the big stuff. You are more likely to be heard if you are known as a reasonable nurse who strives for excellence in their work ethic. If you have reasonable questions, ask the doctor if you could have several minutes of his time. Organize your thoughts, put your emotions in check, and outline your thoughts and rationales. The best outcome would be that the MD would do the same and it would be a learning moment. There is a chance that the doctor will not be as receptive as you would like and you will not impact the decision, but that should not stop you from advocating for your patient in a plain and reasonable manner.
"Dr. Welby, may I speak with you for a minute, privately? I see that you wrote an order to increase Mrs. Steinway's pain medication. I understand that she is rating her pain as a 10, and that's concerning to me, as well. However, when she takes her pain medication, she gets very tired and then refuses to get out of bed for PT and that has always helped her pain tremendously. Is there anything else we can do to help manage her pain, while still allowing her to have the energy to do the things she enjoys and that help her?"
"If I don't agree with a doctor's order, it's important to advocate for my patient in a respectful way. I once had an experience when taking care of a patient with an acute exacerbation of his heart failure. His doctor ordered a high dose of IV Lasix, and he said he was going to order a Foley catheter to make it easier to get a strict intake and output record for this patient. However, the patient was alert, oriented, and not a fall risk, and per our hospital guidelines, we shouldn't jump straight to using a urinary catheter in this case. The catheter could put the patient at risk of infection and skin breakdown. So, I asked the doctor if I could try using two urinals in the patient's room and providing the patient with education about why it was so important to record his urinary output. I also assured the doctor I would put a reminder sign above the toilet in the patient's room, reiterating the teaching to use the plastic urinal rather than the toilet. The doctor agreed to remove the catheter order, and we were able to accurately record the patient's urinary output without it."
10. How would you change your communication style if the patient's family was having trouble understanding what you were trying to tell them?
Nurses are teachers and instruct patients on difficult concepts and challenging instructions. The efficacy of their instructions is extremely important for optimal patient outcomes. For example, if a patient leaves the hospital or clinic setting without full comprehension of the plan of care then they may return to the hospital or have worsening symptoms or complications. Poor comprehension comes with a high burden of decreased patient outcomes, increased financial ramifications for patient and healthcare system, and decreased patient satisfaction. It is extremely important that the nurse learns to communicate with the patient and family in a way that they understand and can implement.
"I review the instructions before I give them to the patient, and I always make certain that I have written ones for them as well. When I review instructions, I decrease the stimulation in the room and make certain I have there attention, and they are not hungry or tired or something else. I look at their faces when I am talking and sometimes you can see the confusion even if they are saying that they understand. Even when they say they understand, I ask them to either show me or explain back to me what I need them to know. Watching them tells me what I missed, and then I keep instructing in different ways until they can explain it back to me."
"People learn in all sorts of different ways. If a patient's family was having a hard time understanding verbal information I'm giving them verbally, I can provide them with written information or with a picture guide. I can also use a hospital-approved patient education video if there is one relevant to the information I'm providing. Once I've switched to a different style or tool, I would request that the family 'teach back' to me the information I've provided them. Then I can assess their understanding and provide additional information as needed."
11. You are caring for a patient who is three-years-old and the physician has ordered a weight-based medication. When you look at the patient's records, you find the weight is documented in pounds. Explain how you proceed.
Many pediatric medications are weight-based, which means the dosage that the patient will receive depends on their weight. However, for most of these medications, the dosing guidance is listed in kilograms and not pounds, the common unit of weight in the United States. Because of this difference in weight units, medication dosing errors in pediatric patients is very common. The interviewer is asking this question to determine if the candidate is aware of the common issues regarding pediatric weight and medication dosing errors and to determine how they would respond in this situation. To effectively answer this question, the candidate should indicate that they would convert the patient's weight to kilograms in order to determine the correct dosage of the medication for the child. A more successful answer to this question would include an example of when the candidate successfully mitigated such a situation during their nursing career.
"If the child's weight was documented in pounds and I had to administer a weight-based medication, the first thing I would do is convert the weight to kilograms so I could determine the correct dosage of medication. While I have always been aware that pediatric medications were dosed based on kilograms, early in my nursing career, I was busy and distracted and nearly overdosed a child with medication because I had forgotten to convert their weight to kilograms. Luckily, one of my colleagues, who saw me draw up the dose, stopped me, or I would have committed the medical error. Ever since this day, I have always been very cognizant of weight documentation when administering pediatric medication."
"If the physician orders a weight-based medication for a 3-year-old, and the child's weight is documented in pounds, I would convert the weight to kilograms and document the weight in kilograms in the appropriate area of the patient's medical record. That way, the doctor, the pharmacist, myself, and anyone else using the patient's weight to ensure the correct medication dose would be working with the patient's weight in the correct format."
12. A patient on your unit you are caring for has had his peripheral venous catheter in place for approximately 100 hours. The catheter looks normal and the vein is open. Tell me how you proceed with administering more IV medications.
In order to help prevent nosocomial infection, which is an infection a patient acquires while receiving care in a hospital, peripheral catheters should be replaced every 72-96 hours. If not changed, the IV catheter may become infected and cause the patient's hospital length of stay to increase or could even cause death in extreme cases. Although a peripheral catheter may look normal and the vein may be open, it is imperative the catheter be changed. The interviewer is asking this question to determine if the candidate understands the importance of changing peripheral catheters on time in order to prevent infections. To successfully answer this question, the candidate should indicate they would change the catheter, specifically noting that the catheter should have been changed at a maximum of 96 hours.
"This patient's peripheral venous catheter needs to be changed, no matter how good it may look. Unfortunately, you can't see bacteria, and these types of catheters are prone to infection, so they must be changed often. In fact, this patient's IV catheter should have been changed prior, as they shouldn't be inserted more than 96 hours. I typically change my patients' IV catheters every 72 hours, which is at the low-end of the suggested range for changing, just as a precautionary measure. So in this case, I would change this patient's IV catheter before administering anymore medication and change it every 72 hours after that."
"Although I would be glad that the patient's peripheral venous catheter site does not show signs of infection, this site can't be used anymore. It's an infection risk to keep the same peripheral venous catheter in place for over 96 hours. Before administering IV medication to the patient, I would change the site, making sure to place the date and time both on the dressing and in the electronic medical record. Because I may or may not be the patient's nurse it's time to change the IV catheter, I could also write 'change by ___ date at ___ time' on the dressing, to better ensure that the IV catheter would be changed within 96 hours, or sooner if that is unit policy. Changing IV catheters per unit policy is one of the important ways that we as nurses can prevent infections and phlebitis in our patients."
13. You are conducting intake on a patient who was just seen at your facility earlier in the week. After you enter the patient's vital signs, you see their medication list, which was updated earlier in the week. Tell me how you proceed.
Because patient medications can change very quickly, even over a few days, it is important that nurses verify current medications for every patient at the beginning of every patient visit. If a patient's medication list is not verified and accurately updated, they are at risk of being prescribed a new medication that could interfere with one they are taking. If the nurse does not verify and update the patient medication list, the prescribing provider will not be aware of undocumented medications and will not be able to avoid prescribing errors. The interviewer is asking this question to assess whether or not the candidate understands that medication must be reviewed and verified with the patient or a caregiver during each encounter. To effectively answer this question, the candidate should indicate that they would review and verify the medications with the patient. A more successful answer to this question could include an example of how the candidate has dealt with a similar situation in the past, learned from a mistake that was made because they did not verify the medication, or spearheaded a policy change at their facility to ensure medications are verified during each patient visit.
"I would review and verify the patient's medication with them again, even though they were just seen in the facility a few days prior. It is too risky to assume that the patient's medications have not changed, as the provider may prescribe a medication that interferes with something the patient is taking that is not documented. Unfortunately, I had to learn this lesson the hard way early in my career. It was a similar situation, where a patient had just been seen a few days earlier, and I assumed their medication list was the same, so I did not ask about it. The next day, I learned that the patient had a bad reaction due to a medication interaction from something they were taking that wasn't documented and a new medication that was prescribed by the doctor during the appointment the previous day. Luckily, the patient was okay, but after this happened, failing to verify medications was a mistake I only had to make once."
"When when reviewing any kind of intake record with the patient, it's important to read to the patient what is already in our record, rather than just saying 'Has anything changed since your last visit?' We can't assume the patient knows what is written in their electronic medical record, or that everything was documented completely the last time. Therefore, after I entered the patient's vital signs, I say to the patient, 'Okay, now we're going to update your medication list.' I would read the list to the patient to have her confirm each medication/dose and make any changes as needed. Then I would ask if she is on any additional medication."
14. We are work with difficult and uncooperative coworkers, at times. How do you handle uncooperative coworkers?
Nursing is challenging and stressful sometimes. People get cranky, machines break, trays are late, and families are needy. Nurses are human beings and have off days. However, the goal for excellent patient outcomes must take precedence over bad days and bad moods, and the interviewer is looking for a candidate who can weather the storm, hold their own, and get the job done for the patient, without adding stress or chaos to the situation.
"I have learned to work out my emotions first, before I address issues. I take a minute to think things through. Sometimes you only have a minute, but I take it. I ask myself if I was reasonable. Was there anything else going on? Was I clear in my communication as to what I needed? Is this a pattern or is the coworker just having a busy or off day? I assume best intentions and own my part of the interaction before I address it, or do the best I can, but I don't let it wait. Patient care cannot wait, and if it's something clinical that needs done, I figure out how to get it done or get what I need from that worker right then and ask if there is a time when I could speak with them later in more detail. I don't think it benefits anyone to get angry or frustrated, but it doesn't help to not address problems either."
"I generally get along well with most coworkers because I have a calm attitude and I always offer to help my colleagues when I am able. However, everyone can have a bad day, including me. If a coworker seems to be grouchy or having a bad day, I would give them more space than usual while still offering my assistance whenever possible. If I noticed a pattern where a certain coworker always seems to be rude or curt to me, I would probably ask her if I could talk to her privately. Then, I would ask if I have done anything offensive or if there is anything I could do differently to be more helpful to her. I would attempt to take any input my coworker gives and implement it. It may not improve her attitude, but I think it's important to try."
15. How would you handle a coworker who is habitually late, which causes you to leave work late?
This is a management and leadership issue which impacts other staff members' lives and team morale. However, it's worth taking the opportunity to address it with the coworker individually before elevating it to leadership. There is something happening if leadership is not addressing it, as they would be alerted if they were chronically punching or signing in late. It may be that the time clock is a distance walk to the unit, or they stop at the cafeteria on the way for coffee and the result is they are late for their shift. It is not helpful to be passive-aggressive and complain to other staff members. Learn to have the uncomfortable conversation directly, kindly, and professionally with the person or people that need to hear it.
"Laine, can I speak to you privately for a minute? Is something going on? I am a little concerned. This is the third time this week you have been at least 10 minutes late, and it's really affecting me, as I have to leave to get my kids on the bus. I've not mentioned this to leadership. I wanted to talk to you first and ask you to be here on time to relieve me. Will you please do that? I would appreciate that very much."
"After a few instances, I would address this issue with my coworker directly. I would let her know that her coming in late is causing me to be late to take my daughter to school, and the situation can't continue. If it continues after this point, I would bring it up to the charge nurse on my shift."
16. Tell me about a time you were uncomfortable with a colleague. How did you handle the situation?
The interviewer asks about a time when you felt uncomfortable with a colleague to gauge your communication, critical thinking, and problem-solving/conflict-resolution skills. They want to know how you handle difficult situations and whether you can work effectively with others. It's important to be honest about the situation and explain how you approached it in a professional and respectful manner. This shows that you can resolve conflicts and maintain positive working relationships. There are, unfortunately, many ways that a colleague could make their coworkers feel uncomfortable. This can range from making inappropriate comments or jokes, invading personal space, or displaying aggressive or threatening behavior. It's essential to address any behavior that makes you uncomfortable and communicate your boundaries clearly with your colleagues. If that does not solve the problem, the interviewer wants to hear that you would report the situation to a supervisor or HR.
"When I first started at my current job, a colleague made inappropriate comments about my appearance. I found it uncomfortable and unprofessional. I decided to address the situation privately by calmly expressing my discomfort with their behavior and explaining that it was not acceptable. I also made it clear that I expected to be treated with respect and professionalism in the workplace. The colleague apologized and we were able to move forward with a more positive and respectful working relationship. It was important for me to address the issue in a mature and professional manner to ensure a safe and comfortable working environment for everyone involved."
"To be honest, there was only one time in my career when I felt uncomfortable with a colleague. During a team meeting, my colleague made inappropriate comments about my sexuality that made me feel uneasy. I didn't feel comfortable confronting my colleague in front of everyone, so I talked to them privately after the meeting. I approached my peer and calmly explained how their comments made me uncomfortable and why it was inappropriate. My colleague seemed surprised and apologized immediately. They also thanked me for bringing it to their attention and promised to be more mindful in the future. In fact, they apologized for their remarks at the next team meeting, which I appreciated. After that conversation, I felt much better and was able to continue working with my colleague without any further issues. It was definitely a difficult situation, but I'm glad I addressed it directly and respectfully."

Jaymie's Feedback
17. Describe how you handle and interact with hostile or aggressive patients.
No matter where you work as a nurse, you will encounter aggressive or hostile patients throughout your career. Patients may become aggressive or hostile due to a medical emergency, intoxication, head injury, or cognitive disorders, to name a few. The interviewer asks you to describe how you handle and interact with hostile or aggressive patients to gain insight into how you handle difficult situations. It's crucial to maintain a calm and professional demeanor when dealing with patients who may be upset or aggressive while still providing the necessary care and attention. This skill is essential in any healthcare setting, and the interviewer wants to ensure you have the necessary experience and qualities to handle the job effectively. Be sure to give specific examples of how you have handled similar situations in the past and demonstrate your ability to remain calm and collected under pressure. You also want to stress how you know when to call for security or outside assistance when needed to protect yourself and your patients.
"My top priority is always safety when dealing with hostile or aggressive patients. I remain calm and composed and try to defuse the situation by listening carefully to the patient's concerns and providing reassurance. I try to determine if the patient is sick or injured or if they are having a mental health crisis so I can call for the appropriate help. If necessary, I may need to involve other healthcare professionals or security personnel to ensure everyone's safety. Regardless of the situation, I treat the patient with respect and empathy and strive to find a solution that meets their needs while maintaining a safe and secure environment for everyone involved."
"Working in the emergency department most of my career, I deal with hostile and aggressive patients daily. First, I always prioritize safety for everyone involved. I remain calm and composed, using a reassuring tone of voice and body language to de-escalate the situation. I listen attentively to their concerns and validate their feelings while setting clear boundaries and expectations for respectful behavior. If needed, I involve other healthcare professionals or security personnel to ensure the safety of everyone involved. My ultimate goal is to provide all patients the best possible care and support, even in difficult situations."
Creative Thinking
18. What are some action steps you could take to alleviate stress in patients in an ER waiting room?
Emergency room waiting rooms are stressful places. After all, everyone in that waiting area is experiencing some kind of emergency and many of them feel their need is just important as anyone else's. Time slows down when someone is frightened, sick, or in pain, so even the shortest wait can get tempers flaring. People who are sick do not have an expansive world view but naturally are narrowly focused on their situation. They may have no ideas of the car crash victims arriving via ambulances through the back but only know that they are waiting. There are a limited number of things that you can do to shorten the wait, but you can humanize the experience by letting them know that they are seen and valued. When they come in, explain the wait time because knowledge is power. Check in with them every so often. Remind the individuals who accompany them where the cafeteria is. There really is nothing you can do to lessen their wait, but you can reduce their frustration by acknowledging their wait time and providing information in a friendly and respectful manner.
"Although it's difficult to face angry and frustrated people, I think it's important to lean in and acknowledge their frustration and give them updates. They are in the ER, so nurses should be checking on them; even just a little bit goes a long way. It is good nursing. I also think it's important to let them know where the comfort stations and cafeteria are located."
"The ER waiting room is usually a stressful place, especially if the ER is busy and the waits will be long. Although some patients and companions will still feel frustrated after I do so, I will make sure to provide as accurate an estimate of their wait time as possible. I will make sure to check in with patients and their companions when I can and update them if their wait time is going to be longer than we originally anticipated. I will allow them to vent their frustrations and let them know I understand that it's stressful. I will also remind the patient's companions where the cafeteria and closest restrooms are."
Critical Thinking
19. You are rounding on your patients on your inpatient unit, and as you enter an elderly woman's room, you find her sitting up and alert. Tell me what steps you take to prevent her from falling between now and the next time you round.
Falls are a common risk for patients who are receiving inpatient care, particularly among the elderly or patients with decreased mobility. Because of this, falls prevention is a common initiative at most hospitals and care facilities. Most nurses are expected to round on their patients hourly, at a minimum, and during these rounds, they are expected to ask their patients about the four P's - Pain, Potty, Positioning, and Possessions. By ensuring the four P's are covered, the nurse is ensuring the patient is comfortable and has everything they need, which will likely prevent them from attempting to get up on their own, hence preventing falls. The interviewer is asking this question to determine if the candidate has an understanding of falls prevention and the four P's of nursing. To effectively answer this question, the candidate should describe how they would check on the patient using the four P's. A more successful answer to this question can include a situation of how the candidate has used the four P's to prevent a patient from falling in their nursing career, how they trained a colleague on the four P's, or even how they implemented a falls prevention program at their facility using the four P's.
"In this situation, I would go through the four P's with the patient to prevent her from attempting to get up and falling between then and the next time I rounded on her. I would first assist her to the restroom then help her relieve any pain she was having. Then, before I left the room, I would ensure she was in a comfortable position and had everything she needed near her. This is something I do with all my patients, even if they seem well enough and able bodied, because failing to do so could mean they may attempt to get up on their own and fall. This is a part of my job as a nurse that I take very seriously because I know how serious patient falls are."
"Early in my nursing career, I had an alert and oriented patient fall when trying to get up himself to use the bathroom. Although the patient didn't sustain any injury, that incident really drove home to me how important it is to work to prevent falls for my patients. Before I leave this patient's room, I will assess to make sure all of her needs are met. Does she need to go to the bathroom? Is she sitting comfortably? Does she have her water, any other needed possessions, and her call light all within easy reach? Does she need any pain medication? Once I have addressed all of these concerns, I will reiterate to the patient to please call if she needs anything, rather than trying to get up herself."
20. You are currently in a patient's room during hourly rounds and although she is not due for another dose of pain medication for two more hours, she is complaining of increased pain. Tell me how you proceed.
The interviewer is asking this question for two reasons - first, to ensure the candidate will not give the patient a dose of pain medication before it is due; and second, to see if the candidate will attempt to lower the patient's pain using other comfort measures. While the administration of pain medication will relieve a patient's pain, it is important that pain medication is administered as directed by the physician, in order to avoid patient overdose or other negative side effects. Although patients may ask for pain medication in advance of their scheduled dose, nurses can help reduce their pain using other comfort measures, such as repositioning, offering heated blankets or warm compresses, helping them stretch, or getting them up for a walk. To effectively answer this question, the candidate should indicate that they would avoid giving the patient their pain medication early and instead use alternative comfort measures to help reduce the patient's pain. A more successful answer to this question would include an example from the candidate's nursing career where they helped a patient manage their pain using comfort measures rather than pain medication.
"Unfortunately, since the patient is not due for their medication for a couple of more hours, I would not be able to administer it to them. But, I would be able to help reduce their pain using other comfort measures. So, instead of simply telling the patient that they could not have any medication, I would work with them to see what I could do to make them comfortable in the meantime. Having many years of experience as a nurse in the emergency department, I have a lot of experience helping patients manage their pain when they do not get the desired relief from pain medications that were administered, and I would be able to draw from this experience to help this patient get relief until their next dose of medication."
"If a patient is not due for their pain medication for two more hours, I would explain to the patient when they can next have their pain medication. I would explore non-medication measures, such as heat, cold, repositioning, massage, or other options. Many patients that I've worked with over the years have found relief with non-medication interventions. During this time, I would also be reassessing the patient to see if any changes have occurred in the patient's condition--for example, if a surgical site looks reddened when it hadn't before, or if a patient was complaining of increased pain in their foot and their pedal pulse was weakened or absent when it had previously been palpable or audible by doppler. If any changes have occurred in the patient's condition, I would contact their doctor and report these changes."
Customer Service
21. Everyone on your unit is busy and you requested that your unit's nursing assistants bathe one of your patients earlier today. The patient has yet to be bathed and she is upset about it. Tell me how you proceed.
Inpatient nursing is very much a team effort, and while nursing assistants and care partners are typically available to assist with tasks such as bathing patients, they are sometimes at capacity and are unable to take on all the requests. In these situations, it is a requirement of all members of the care team, including nurses, to care for the patient, and this includes changing, bathing, or otherwise cleaning them. To effectively answer this question, the candidate should indicate that they would take initiative and bathe the patient rather than allowing the patient to wait even longer and become even more upset. A more successful answer to this question would include a specific example from the candidate's nursing career where they provided similar care for a patient when nursing assistants were unavailable.
"In this situation, it sounds like the nursing assistants are very busy and are unable to get to the request put in for the patient. So, I would cancel the request I previously sent to the nursing assistants and bathe the patient myself. Not only would this help my patient feel more comfortable, it would help my nursing assistant team members out as well because it would be one less thing they would need to do. I know I am a nurse, but I do not feel I am above doing things like changing and bathing patients. To me, these tasks are part of providing adequate care to my patients, and I will always do what is needed."
"If the patient had not yet had her bath, I would apologize and let her know I would help her with her bath right away. Then I would set up the bath and assist my patient. Having the help of a nursing assistant is so useful, but sometimes a nursing assistant gets too busy with other tasks to complete every request. Helping my patient with her bath is a great time to assess her skin and any lines, wounds, or surgical sites. It's also a time I can get to know the patient better, reiterate any teaching we're working on, and find out if there are other needs she has."
22. Tell me a time when you went above and beyond for a patient.
The interviewer wants to gauge your commitment and passion for the nursing profession and learn more about your dedication to providing exceptional patient care. They want to know if you will go above and beyond the call of duty to ensure patients receive the best possible care. By asking this question, they hope to hear a specific example of a time when you went above and beyond for a patient and how it positively impacted their care and overall experience. One example of going above and beyond for a patient would be taking extra time to sit and talk with them, providing emotional support and reassurance during a difficult time. Another example could be staying late to ensure your patient receives the necessary treatment and care, even if it means sacrificing your own personal time. Overall, going above and beyond for patients involves showing empathy, compassion, and a willingness to go the extra mile to ensure their well-being and comfort.
"Last week, I had a patient who was feeling very anxious and nervous about their upcoming surgery. Despite my busy schedule, I took the time to sit with them and listen to their concerns. I reassured them that everything would be alright and answered all of their questions to the best of my ability. I even stayed with them after my shift ended until their family arrived to provide additional support. The patient later wrote a note to the hospital praising the care they received, and it was gratifying to know that I was able to make a positive impact on their experience. To me, it didn't seem like I went above and beyond, but the patient sure thought I did!"
"Recently, one of my patients was feeling very down and missing their dog they hadn't seen in weeks due to being hospitalized. I knew how much their dog meant to them and how it could help lift their spirits, so I went above and beyond my duties and sought permission to bring their dog into the hospital. After obtaining the necessary permissions, I arranged for the patient's dog to visit them in their room. The patient's face lit up with joy, and they were so grateful for the opportunity to see their longtime companion. It was a heartwarming moment, and I was glad to be able to bring some happiness into their day."
23. You are assisting a physician to perform a procedure when you are asked to retrieve a bottle of acetic acid that can be used on the patient. After retrieving the bottle from its normal location, what do you do before passing it to the physician?
The interviewer is asking this question to determine if the candidate would verify that they retrieved the correct chemical before passing it to the physician. This confirmation is important, as the nurse may have accidentally retrieved the incorrect bottle or a bottle containing a different chemical may have been in the place where the requested chemical was typically kept. If either of these were the case, and the incorrect chemical was passed to the physician and used on the patient, significant consequences could occur. Simply verifying that the correct chemical is being passed to the physician could help avoid a serious medical error. To effectively answer this question, the candidate should indicate that they would verify that they have the correct chemical by checking the label on the bottle. A more successful answer to this question would include a specific example from the candidate's nursing career where they avoided a medical error by verifying the name of a chemical or drug that was to be administered to a patient.
"I know exactly what I would do in this situation, as I have been in a situation almost identical to this. Before handing the bottle to the physician, I would read details on the label to verify that I am handing them what they requested. This is similar to a situation I was in a few years ago, while I was working in an oncology office and was assisting a physician with a colposcopy, which requires acetic acid. During the procedure, I went and grabbed the bottle, which I assumed was acetic acid, from where it was normally stored on the shelf; but when I checked the label, I found that it was sulfuric acid, which would have burned the patient if applied. Someone had placed the sulfuric acid in the incorrect location, but since I verified I had the correct chemical, I avoided a medical error."
"In this situation, before I hand the bottle of acetic acid to the physician, I would read the label to make sure that I was actually giving the physician the medication she requested. Although it has not happened to me directly, in my hospital there was a situation where a concentration of heparin was stocked in a location where a different concentration was normally placed, and a nurse administered the incorrect concentration to a patient. During my orientation, this incident was brought up to us as an example of why we always have to verify the name and dose of a medication, even if we take a bottle or bag from its 'usual' place, and it's always stuck with me."
24. You just finished preparing IV medications for a patient, and you thoroughly washed your hands before doing so. As you enter the patient's room with the medication, describe the first thing you do to prevent patient infection.
While hospitalized or receiving outpatient medical treatment, patients are at significant risk of picking up an infection as a consequence of the care they are receiving. Although infection prevention measures in the healthcare industry have greatly improved over the years, the risk still exists and healthcare professionals must be vigilant in order to prevent healthcare-acquired infections. Although it may seem obvious, the simple task of handwashing is the first step in infection prevention. The interviewer is asking this question to determine if the candidate understands the importance of handwashing and is in the habit of washing their hands upon entering a patient's room and/or before administering IV medication. To effectively answer this question, the candidate should explain that the first step they would take to prevent infection would be to wash their hands thoroughly. A more successful answer to this question would include an example of how the candidate has helped train colleagues on handwashing in such situations and/or assisted in the development and implementation of handwashing policies for their nursing unit.
"The first thing I would do to prevent the patient from getting an infection is to wash my hands. There are other actions I would need to take in preventing infection, but handwashing is primary. I have always been an advocate of handwashing, even when many of my colleagues were not. When I found out that my nursing and care partner colleagues on my unit were not following handwashing protocols last year, I worked with my supervisor to develop a training on the importance of proper handwashing, handwashing technique, and infection prevention. After this training, handwashing compliance on my unit improved greatly, and the infection control nurse attributed it to a reduction in secondary infections."
"Upon entering the patient's room, it's very important for me to practice hand hygiene again, either by washing my hands or using the alcohol-based hand sanitizer available outside of the patient's room. Although I washed my hands prior to preparing the patient's IV medication, I have potentially touched other items on my way to the patient's room, and I had to knock on the patient's door and touch the door handle to enter. Hand hygiene is the number one way to prevent patient infections, and I demonstrate good hand hygiene at all times. When our hospital did an audit of nurses' hand hygiene using 'undercover' staff members to score the nurses, I scored a 100%, because I know how important hand hygiene is."
25. Describe a situation where it may be appropriate to use humor in the workplace.
Being sick is not funny business, and someone coming in cracking jokes under dire circumstances may find their humor is rejected. There is a time for humor in healthcare, but it must be mindful. What people think is funny can vary wildly. If humor is used, it should be very mild and universal. It's a good policy to be kind, tolerant, professional, and compassionate with your patients. Certainly, laugh at a child's joke, if appropriate, and acknowledge a patient's attempt to be cheerful, but follow rather than lead with humor and only support, chuckle or smile at anything that would be universally accepted as OK. Some people poke fun at themselves, but sometimes, it's a self-esteem issue so it's best to avoid playing along.
"I am not opposed to a funny nursing meme posted in the office away from patient eyes, but I feel that we should represent the hospital as compassionate, caring and professional individuals. There's a lot of room for smiling, but I personally save the humor for the comedians."
"If it seems it would help a patient to go along with their light-hearted attempts at humor, I will smile or laugh along. I would never laugh at an offensive joke, political humor, or any type of racism or bigotry, but something light like chuckling at a joke a patient makes about the reputation of hospital food can help the patient feel at ease."
26. What kinds of review questions do you ask yourself after dealing with a difficult and challenging patient situation?
All nurses desire to have positive and impactful shifts every day, but this is not a reality. Things happen, situations go awry, and it's important to reflect as an individual or a team and extract the lesson to learn how to be better. It's human nature to rationalize or justify and not face the difficult feelings or emotions of a situation gone bad, but this reflection is extremely important so that it doesn't happen again.
"I really like to go back and review with myself and the team what happened and ways to be better. I think it's important to distance myself a little bit from the emotions and try to review it logically. I think that when emotions run high, intelligence can run low, and we need to talk about situations and responses for what they are without blaming. That isn't helpful and impedes learning."
"I was a part of an initiative at my hospital called 'Dealing With Difficult Patients.' In this initiative, we learned techniques to help us identify possible situations in which patients or visitors were becoming agitated, and how we could diffuse the situation. Then, we gave presentations to help teach this information to our colleagues. In a case where a patient's anger escalated, I would ask myself, 'What early clue did I miss?' In that way, I will be better able to catch and react to a similar early warning sign next time, and I can hopefully help my coworkers be prepared to identify such a warning sign in the future, too."
27. How would you handle someone asking you for medical advice or diagnosis validation outside the workplace?
This is a difficult challenge for nurses who know things and also have a compelling need to serve others. It's easy and ego-boosting to become the resident 'expert', but that can backfire. There is a reason why when people call the ER for advice, the standard answer is to present for an evaluation and advice isn't given over the phone. We live in a litigious society, and you worked hard for your license. Protect it just as hard. What may seem to be benign advice to your neighbor may result in catastrophic consequences. Also, it is best to give advice that points people in the direction of great care, such as writing down all symptoms.
"Mrs. Lokley...I'm so sorry you're not feeling well. Do you need me to help call and schedule the earliest appointment with your PCP? Do you have a little notebook where you can write down all your symptoms? Sometimes people get overwhelmed at the doctor's and forget to tell them important things. I could help you write out your medication list to take to the PCP. Come, let's make that call now and get you an appointment. You seem very worried, so it's wise to be seen."
"If someone in my life asks for medical advice when they are not working, I offer to help them call their doctor's office or their insurance's nurse triage line. I have not encountered someone in my life asking for this type of advice who does not have insurance or an established doctor. However, if someone who doesn't have an established doctor or insurance asked for medical advice, I would offer to help them get to an urgent care clinic or the emergency department."
28. Describe a time when you had to step into a leadership role.
As a nurse, you are used to working as part of a multidisciplinary team but also know how to take charge when necessary. This question assesses your leadership skills and how you handle challenges and tasks that require you to take control. The interviewer wants to hear about when you stepped into a leadership role to understand your ability to lead in a healthcare setting. You can use this opportunity to showcase your skills and demonstrate how you have successfully led a team in the past, highlighting the skills you utilized to accomplish the goals set forth. It is important to be honest and specific in your response, clearly showing your leadership qualities and how they have benefited your patients and colleagues.
"As a nurse, I have had the opportunity to step into a leadership position on a few occasions. One particular experience stands out in my mind. I was working on a busy medical-surgical floor, and the charge nurse had to leave for a family emergency. I was asked to step in and take on some of her responsibilities. At first, I was a bit nervous about taking on such a big role, but I quickly realized that I had the skills and knowledge necessary to be an effective leader. I worked closely with the other nurses on the floor, delegating tasks and ensuring everyone had the support they needed. I also communicated closely with the doctors and other healthcare professionals to ensure our patients received the best possible care. It was a challenging experience, but it was also incredibly rewarding. I learned a lot about myself as a nurse and a leader, and I felt proud to have been able to step up and help out when needed most."
"I vividly remember the first day I stepped into a leadership role as a nurse. A few years ago, my unit was short-staffed, and I was asked to take charge for the day. At first, I was nervous and unsure if I was up for the task, as I only had six months of experience. But as the day progressed, I found myself stepping up to the challenge and taking charge of the situation. I delegated tasks, made critical decisions, and ensured patient care was at the forefront of everything we did. By the end of the shift, I felt proud of myself for rising to the occasion and leading my team through a difficult day. From that day forward, I knew that I had the potential to be a great leader and continue to strive towards that goal."
29. How would you handle a situation in which nursing leadership were to reject an idea you pitched to streamline your job?
It's difficult to be rejected in any way, and it's really difficult when you excitedly share something that you feel will be helpful and it is not received well. If you pitch an idea to a supervisor or leadership team, ask for good feedback and learn their perspective. While it's easy to become defeated and not want to contribute, nursing needs you on the leading edge of thought. Review your idea and your presentation. Revise your pitch, if necessary, and ask for another opportunity to present your idea after further considerations. Consider the real possibility that you may have not presented your idea in a way that resonated with the recipient.
"I know I would feel disappointed, but I would definitely go back and ask for feedback on my idea and be grateful for the feedback. I would ask for feedback from others to see if I presented my idea in a reasonable way. If I still thought it was a great idea, I would review how I explained it, simplify and reorganize the information, and ask for another opportunity to present. I once heard that Walt Disney applied to 302 banks before he got the loan for Disney Land, so I try to remember that success doesn't always happen right away, but it does leave clues. I would want to know what I did right and what I could improve upon and then learn from the rejection."
"If nursing leadership rejected an idea that I thought would really help streamline my job and the job of my coworkers, I would feel disappointed. But, I would try to figure out if something in my pitch was off or missing. I would ask some of my most straightforward coworkers if I could run my presentation by them to see how I could tweak it. I've always worked with people with amazing ideas about how we can make things safer and more efficient, so I know I would get useful feedback from coworkers. Then I would ask leadership when there will be another opportunity to present my updated idea."
Operational
30. You are preparing medication in your unit's med room when you are paged to the nurse's station. You plan to immediately return to the med room, which you can see from the nurse's station. Do you lock the door upon leaving the med room?
While most medication rooms in hospitals and clinical facilities automatically lock when closed with current technology, some do not, and in these cases, it is important that nurses and other clinical professionals keep the medication room secured at all times. Not only does leaving medications unsecured place the facility at significant financial risk, it also places patients and the public at risk as well. If an unauthorized individual enters an unlocked medication room and takes medications, these drugs will not be available to patients who need them and may end up being misused by those who end up receiving them. The interviewer is asking this question to ensure the candidate understands the importance of securing the unit's medications. To effectively answer this question, the candidate should indicate that they would ensure the medication room was secured. A more successful answer to this question would include a specific example from the candidate's nursing career where they were in a similar situation or when they helped develop or implement a new policy for securing medications for their unit.
"Even though I would only going to the nursing station and could see the medication room, I would lock the door behind me. You can't take chances with the medication room, and there is no guarantee that you are only being called away for only a moment. In my nursing career, I've learned that a quick page to the nursing station could mean I am away for a 15-minute period, or even longer. The environment on the nursing unit is too volatile to assume you can visually monitor an unlocked medication room, so it is best to ensure the room is secured at all times. Each time I leave the medication room on my unit, I ensure it is locked, and I will continue to do so no matter where I am working."
"In all of my previous inpatient nurse jobs, the medication room had an automatic lock so that every time the door closed, the med room door locked. I think this is an ideal setup, because the medication room always needs to be locked, even if a nurse thinks he or she will be away for 'just a minute.'. In this scenario, if the med room door doesn't automatically lock when shut, yes, I would lock the door upon leaving, no matter how short of a time I think I will be gone."
Performance Based
31. Your patient, who has just returned from surgery, now has multiple tubes and lines that you did not insert. You need to administer a drug into her central line, but are having a hard time finding this tube. As you are in a rush, tell me how you proceed.
When returning from the operating room, intensive care unit, or other units of the hospital, a patient may have many more tubes and lines inserted into their body than normal, and at times, it may be difficult for a nurse to differentiate the lines. This is especially the case if the nurse is in a rush. In this scenario, the nurse, in order to administer medication into the patient's central line, they should take time to ensure they have the correct tube. Administering the medication into the incorrect line or into a drain is a medical error that could have negative consequences for the patient. The interviewer is asking this question to determine if the candidate would take the time to confirm that they are using the correct tube to administer the medication in the patient's central line. To effectively answer this question, the patient should indicate that they would carefully ensure that they had the correct tube for the central line before administering the medication. A more successful answer to this question would include a specific example from the candidate's nursing career where they were in a similar situation, and they took time to ensure they were administering a medication in the appropriate line.
"I was in a very similar situation a couple of weeks ago when one of our patients returned from the ICU with a number of new tubes and lines that were all scattered around. When I received an order to flush one of the patient's lines, I had to take time to ensure I had the correct tube, as I did not one to mistakenly flush a drain or flush the wrong line. So, in the case of the patient you just described, even though I am in a rush, I would take the time needed to ensure I was pushing the medication into the patient's central line and not a different tube."
"In this scenario, I would need to make sure to identify the central line before doing anything else. Being in a rush, it may make me feel stressed to take this time, but administering the medication through an incorrect line could have big consequences.."
32. You are caring for a patient on your inpatient unit, and after making a call to the physician hospitalist on staff for support, you learn that the patient's medication regimen needs to be changed. Tell me the first steps you take.
While many individuals may believe the first step a nurse should take in this situation would be to give the patient the new drugs that were verbally ordered by the physician, this is not the case. The first step the nurse should take after receiving the verbal order by the physician is to document the medication change in the patient's electronic medical record. Documentation errors are very common among nurses, and these errors include failing to document medications, procedures, and/or nursing actions. Because nurses are extremely busy and often distracted by multiple tasks and demands, it is important for this type of information to be immediately be documented in the patient record. To effectively answer this question, the candidate should indicate that they would document the changes in the patient's medication regimen before administering medications to the patient. A more successful answer to this question would include specific details from a similar situation from the candidate's nursing career where they ensured changes to the patient's care regimen were documented before administering care to the patient.
"I actually dealt with a similar situation last week. It wasn't medications in particular, but I had to call our hospitalist because one of my patient's pulse ox was getting very low, and I was beginning to worry about him. Once the hospitalist learned about the patient's condition, she ordered oxygen for the patient, and the first thing I did was document the verbal order in the patient's medical record. I knew if I didn't document the order immediately, there was a chance I would get busy and forget, which could have detrimental consequences for my patient."
"This is a scenario I encounter all of the time as an inpatient nurse. In my current hospital, we have physician order entry, so the physicians often enter their medication orders themselves. However, there are still times when a physician will need to give a medication order verbally. If the physician gives the order verbally to me over the phone, I will enter the order into the EMR under her name, repeat back the order out loud to verify all of the info is correct, and then sign the order. Then, once pharmacy has verified the order on their end, I will be able to pull the medication from the Pyxis machine in the medication room and take the appropriate steps to administer the medication to the patient."

Marcie's Feedback
Problem Solving
33. During your shift in the ER, a patient presents with bruising from a fall. Her male companion answers questions for her, and she barely gives eye contact. What do you do in this situation to get the patient to answer independently?
Sometimes a domestic abuse victim's only connection to help might be a trip to the ER or urgent care. All patients should be screened for abuse whether man, woman, or child. A nurse needs to know the warning signs and learn how to assess and ask effective questions. The nurse needs to learn how to optimize the interview and assessment so that the patient (man, woman, or child) can express themselves in a safe space. In the above scenario, the nurse needs to separate the woman safely from the man, so that she can ask if the woman feels safe and assess her for abuse. It may be difficult to separate the individual from the companion, but it's best they be separated, as the potential abuse victim may not speak openly in front of the abuser.
"I would need to separate the potential abuse victim from the abuser, though I understand that it may be difficult. I could ask him to leave the room for the assessment and if he balked, I would probably take her to the bathroom for a urine sample to ask her questions. I would be careful not to judge or prejudge the situation, but I would do what I needed to do to assess the potential abuse victim thoroughly. I definitely would seek guidance from my shift leadership."
"It's possible that this patient is the victim of abuse. In order to make sure the patient can give honest answers about what caused her injury, I would ask the companion to leave the room so I can complete my assessment. If the companion refuses, I can explain that I need to get a urine sample from the patient and escort the patient to the bathroom so that we can talk privately. If the patient or companion refuses this as well, I would talk to my charge nurse about what other actions I can take."
34. You are caring for a patient on your inpatient unit who is bedridden and unconscious. When the patient came to you, they already had a bedsore. How do you prevent this from happening again?
For patients who are bedridden, bedsores can be a common, but avoidable, problem. If these sores become infected, the consequences for the patients can be severe, especially if they are in a weakened medical state. To prevent bedsores for their patients who are bedridden, nurses should ensure their patients are repositioned at least once every two hours. This repositioning may be completed by a care partner or nursing assistant, but it is ultimately the responsibility of the nurse to ensure their patients are properly cared for. The interviewer is asking this question to ensure the candidate understands it is their responsibility to protect their patients from hazards such as bedsores. To effectively answer this question, the candidate should indicate that they would ensure the patient was repositioned at least every two hours. A more successful answer to this question could include examples of how the candidate has worked with physicians and the physical therapy department to ensure the patient was properly moved, trained care partners or nursing assistants on proper patient repositioning, or helped their colleagues prevent bedsores in similar situations with their patients.
"To prevent additional bedsores, I would ensure the patient was moved and repositioned every two hours, at a minimum. If I am fortunate enough to have the support of a nursing assistant while caring for this patient, I would as for their help, but I would still ensure my patient was being moved, rather than assuming it was being done. I know how serious bedsores can be, and I do everything I can to prevent them. If the patient is unconscious for a long period, I will usually ask the physician if the patient needs an intervention from physical therapy, not only to prevent bedsores but to also prevent muscle atrophy."
"To prevent the bedridden patient from developing additional bedsores, I would work with my team to make sure the patient is turned every two hours. I will document the patient's turning and what position we moved the patient to. If available, I will try to get the patient a specialized hospital bed that uses air to help prevent further pressure ulcers. I would use either pillows or waffle boots to prevent pressure ulcers from forming on heels. I would use a foam dressing or other appropriate material to pad any bony prominences that are in danger of contributing to skin breakdown."
Role-Specific
35. Describe a time when you did not provide the type of patient care you normally would. What could you have done to improve care?
The interviewer is interested in your ability to recognize your shortcomings and that you learn from your mistakes. They want to see that you are self-aware and constantly strive to improve your patient care skills. Discussing a time when you fell short demonstrates your willingness to learn and grow as a healthcare professional. Ultimately, the goal is to provide the best possible care for all patients, and being able to reflect on past experiences is a valuable tool in achieving that goal. Describe a time when you did not provide the care you normally would, the reason why, and what you learned from that experience.
"When I first started working as a nurse, there was a time I didn't provide the type of patient care that I normally would. I felt overwhelmed by the number of patients I had to take care of, and my energy levels were low as I felt like I was getting a cold. As a result, I wasn't as attentive as I could have been. Looking back, I realize I should have taken a break and refueled my energy or called in sick before my shift started, as I was not feeling well. I also could have asked for help from my colleagues or supervisor to ensure that all patients received the care they needed. Being new at the job, I did not want to appear as if I could not handle the work, even if a little under the weather. However, I now realize that I cannot help others unless I take care of myself, and I pay close attention to how I am feeling before each shift."
"I have always strived to maintain a professional demeanor while on duty. However, one time, my personal issues almost got the better of me. I was going through a rough patch in my personal life and was finding it hard to focus on my work. One day, I was assigned to care for a particularly challenging patient. Despite my best efforts, I became increasingly short with them and less patient than I should have been. It was only after a colleague pulled me aside and reminded me of my duty to my patients that I was able to put aside my personal problems and focus on providing the best care possible. It was a valuable lesson that I will never forget and has made me a better nurse. Looking back, I realize I should have taken time to deal with my personal issues outside of work and not let them interfere with my responsibilities. It's important to remember that our patients rely on us to provide the best care possible, and we need to be fully present and focused on their needs."
36. You are caring for a patient on your unit who is now resting well but has tried to get up and fallen multiple times over the past couple of days. As you prepare to leave the patient's room, do you restrain her to prevent her from falling again?
While it may seem like the most rationale step to take in this situation would be to restrain the patient, only current behavior should determine whether a patient should be restrained. The use of restraints can have physical and psychological consequences for the patient, so it is important that nurses and other medical professionals be very careful with their use. In this situation, since the patient is resting well and not agitated, the nurse should avoid using restraints. The interviewer is asking this question to determine if the candidate understands that restraints should be used judiciously, and to effectively answer this question, the candidate should indicate they would not restrain the patient in this situation. A more successful answer this question would include an example from the candidate's nursing career where they chose not to restrain a patient based on current behavior, despite previous history of falls, violence, and/or intentional or unintentional self-harm.
"Since I have been an inpatient nurse for many years, I have dealt with these types of situations many times, and in this situation, I would not restrain the patient. Even though the patient has fallen since she has been admitted, if she is currently resting well and isn't agitated, I would not restrain her. Restraints are very difficult for patients, and I will not use them unless it is absolutely necessary. This reminds me of a patient who I was caring for recently who had been violent and restrained while in the ICU, but when he was transferred to my unit, he was much calmer. The nurse who cared for him the shift prior to mine had kept him restrained, as she was fearful of him, but the patient was now much more lucid and the restraints were stressful to him. Once I took the handoff, I immediately removed the restraints from the patient, and from then on, he was able to relax."
"Restraints should be used as a last resort, as they can be upsetting to patients and their family members, and they may increase the risk of other types of injury, such as skin tears or pressure wounds. I would work with my patient care tech and other nurses to implement other measures, such as frequently rounding on the patient to make sure her elimination needs are met. We could also place a bed or chair alarm underneath the patient to make sure staff are alerted if she tried to get up, and we could place fall alert socks on her feet so that the color indicates to all staff that the patient should not get up by herself."
37. You are caring for a patient and the physician has ordered an IV medication for them. You have collected the medication and the supplies needed to administer the IV. Tell me how you will proceed from this point.
Before starting an IV and administering the medication, in this situation, the nurse should look in the patient's electronic health record and review the physician's medication order to verify they have the correct medication, dosage, and administration duration. This is a safety protocol that is standard in nursing practice to prevent medical errors, as administering the incorrect medication, incorrect dosage, and/or incorrect duration can have dire consequences to the patient. The interviewer is asking this question to assess the candidate's understanding and regular practice for such precautions. To effectively answer this question, the candidate should indicate that they would verify the medication, dosage, and administration duration by reviewing the order in the electronic health record. A more successful answer to this question could include examples of how the candidate prevented a colleague from committing a medical error by reminding them to review this information, helped develop training materials on the matter for their unit, or even helped change protocols to improve compliance and patient outcomes.
"Before I did anything to the patient, I would go to the patient's electronic record and verify the drug name, the dosage, and the administration duration. This is so important because so many times, nurses are busy or get distracted and accidentally grab the wrong medication, dosage, or set the incorrect administration duration. A couple of years ago, we had several new nursing graduates working on my unit, and we had several medical errors related to this issue take place. Because I am so passionate about this issue, I helped my supervisor develop training materials to help remind my colleagues to verify these medication elements before they administer IV drugs. While these materials did not eliminate medication errors, they helped reduce them."
"Before administering the IV medication, I would check the patient's wristband and/or verbally confirm the patient's name and date of birth with the patient. Then I would verify the medication order in the patient's electronic medical record, ensuring that the medication, dose, route, and duration all matched the information that I have."
38. In your inpatient unit, you are caring for a patient who is still weak from surgery. Upon reviewing physician orders, you see the patient is to get up and walk two laps in the hall. Tell me how you would proceed.
The interviewer is attempting to determine if the candidate would assess the patient's ability to participate in physical activity before getting her up to walk around the hall of the inpatient unit. Patient falls is one of the biggest patient safety concerns for hospitals, and it is the onus of the nursing staff to ensure they protect their patients from falls in all situations, even when there is a physician order stating otherwise. To effectively answer this question, the candidate should indicate that they would assess the patient's ability to participate in the physical activity, and if they, in fact, the patient was too weak, they would contact the physician for alternative orders. A more successful answer to this question would include a specific example from the candidate's nursing career where they prevented a patient fall by assessing their ability to participate in physical activity.
"If the patient was still weak from their surgical procedure, I would assess their ability to get up and walk, to ensure they are not at risk for a fall. This is something I deal with often at my current job as an inpatient nurse. Just recently, I was caring for a patient who had been admitted for a serious infection. When the patient seemed to be getting better, the physician ordered that he get up and walk, and he did well the first couple of days. However, on the third day, he was feeling worse, and when it was time for his walk, instead of just getting him up, I assessed his condition and found that getting him up for a walk would put him at risk. Upon calling the physician and updating him on the patient's condition, he came to check on him, and found that the patient needed emergency surgery as the infection had returned. Not only did my diligence prevent the patient from becoming injured, it also helped alert the physician of an emergent issue."
"When I worked on the post-op cardiac unit, we were constantly assessing if patients could safely walk around the unit with just a nurse to support them. Ambulating after surgery is very important to increase strength and decrease the chance of pneumonia, blood clots, and other complications. However, if a patient isn't ready to walk, even with a gait belt or a walker, they could risk falling and sustaining serious injury. In this case, I would assess the patient and see if he can safely walk 2 laps in the hall. If his assessment shows that he can walk 2 laps in the hall, I would walk with him. If the assessment did not show that he could safely do this yet, I would contact the physician, explain the scenario, and request an order for a physical therapist to come to evaluate and work with the patient."
Scenario Based
39. How would you handle a patient that assumes a 'helpless' role, does not do what is necessary for their treatment, and asks you to do certain tasks that they could and should perform for themselves?
A nurse cares about patients, so it's difficult sometimes to recognize when we over function for patients and do not encourage them to be their best. Doing too much for patients is as damaging as doing too little. Nurses need to learn the subtle dance between empathy and advocacy for patients helping themselves. You want to encourage without being demeaning or too harsh, but also push them to do what they can for themselves in every situation possible. A weight lifter doesn't bench press 200 pounds over night but adds weight little by little. Each time a patient swings his own leg out of the bed, or shuffles to the bathroom with the assist of two, wonderful things are building incrementally in his or her body. Sometimes, nurses do things for patients because they are busy and don't have time for the slower patient to do it. Occasionally, on a booming floor this may be necessary, but should be the exception, not the rule.
"Sally, today is bath day and it's a great day to get up and stretch your legs today. No bed bath today. I'll help you up and you can dangle at the edge of the bed while I turn the shower on. It will do you good to get up, and I'll help you so you don't fall, but we are going to try to walk independently to the bathroom today. Does that sound good?"
"When I work with a patient who seems to be acting helpless, I try to use motivational interviewing techniques to help them find a reason for why they might want to participate in their treatment plan. So, we might talk about their trying to get back to their apartment or home, their desire to be able to sit up at their grandchild's wedding, or another goal they want to reach. Then I help them see how taking a walk in the hall or using their incentive spirometer will help them get stronger and more likely to achieve their goal."
40. You have a coworker with a large following on TikTok, who brags constantly about her followers. One day you notice a video of her with one of her patients in the background. What would you do in this situation?
The interviewer asks what you would do if you saw a coworker with a patient visible in a TikTok video because it is imperative to maintain patient privacy and confidentiality. Suppose you were to come across such a video. In that case, the interviewer wants to see if you would immediately bring it to your coworker's attention and advise them to remove it or if you would first inform your supervisor and follow appropriate protocols to protect the patient's privacy. It is crucial to prioritize patient safety and confidentiality in any healthcare setting, and you must be committed to upholding these values. How you respond will give the interviewer insight into your communication, problem-solving, and critical-thinking skills.
Written by Krista Wenz on May 26th, 2023
"As a responsible nurse who takes my job very seriously, I would immediately report the situation to my immediate supervisor. Patient privacy and confidentiality are of the utmost importance in healthcare, and any breach of these principles must be taken seriously. It is important to ensure that all healthcare professionals understand the gravity of protecting patient information and upholding the profession's ethical standards."
"I would be very concerned if I saw a TikTok video featuring my coworker and a patient. It's crucial to prioritize the well-being and privacy of our patients above all else. Patient privacy and confidentiality are critical in this field, and violating them is a serious breach of ethics. I would first speak with my coworker privately to express my concerns and remind them of the importance of maintaining patient privacy. Depending on the severity of the situation, I may also need to report the incident to our supervisor or the hospital's compliance team. Of course, how I proceed also depends on the policies and procedures of my organization."
41. You are caring for a patient on your inpatient unit who is taking a turn for the worse. You decide you need to call the hospitalist physician. Tell me how you will proceed.
Before calling for the assistance of a physician, therapist, or nursing colleague, unless it is a dire emergency, nurses should gather as much pertinent information on the patient as they can so they can effectively and succinctly explain the situation and the needs of the patient. If the nurse does not collect this information in advance of making the call to the physician, the call will likely take additional time as they will have to look the information up and take more of the physician's time. While patients are not typically put at risk in these situations, having the information ready to report during the call assists nurses with building professional relationships with the many professionals the must consult with on a daily basis. The interviewer is asking this question to determine how important the candidate feels it is to collect information before calling the physician. To effectively answer this question, the candidate should indicate that they would collect all pertinent information on the patient, including diagnosis, condition, impression, test results, and vital signs. A more successful answer to this question can include experience from the candidate's nursing career, information the candidate typically relays during such a call, or how the candidate assisted a colleague with such a call.
"This is a very common situation that I find myself in, as I work in the inpatient environment, so I understand that it is important to gather as much information about the patient and the patient's current situation before making the call to the physician. Early in my nursing career, I sometimes would call before I had gathered the necessary information, and when I did so, it was very difficult to communicate the situation to the physician, and sometimes they would become frustrated. Now that I have more experience, I understand the importance of gathering information such as current impression, vital signs, test results, and other pertinent information, so the conversation can be efficient and brief."
"When I call the hospitalist to inform them of a downturn in my patient's condition, I make sure to go over my mental checklist first. Have I gathered all the needed information about the patient's history, current vitals/labs, and changes in condition? If so, I will call, and identify myself and the patient, and then make sure the physician is ready to hear the information I have. One of the first times I needed to call a physician about his patient's change in level of consciousness, I was so anxious that I started talking quickly and forgot to identify myself as the patient's nurse. In trying to get things moving quickly, I actually ended up taking more time than needed, because the physician wasn't clear on who I was. From that point on, I have always taken a breath and made sure to stay calm on calls to physicians."
42. You are alone in an elevator with two nurses from another floor who are talking about a patient. How would you respond?
Interviewers ask situational questions to test interviewees' people skills and their capacity to communicate and find optimal solutions. The answer here doesn't have to be work specific, unless it is apparent as in this question, but it's always a good idea to incorporate appropriate work behaviors in, when possible.
"My grandmother always taught me that when you are silent about questionable things, in a way you are agreeing with them, or people might think that you are. I feel strongly about protecting patient rights, and I would be very uncomfortable in that situation. I think that I would feel compelled to address it right on the spot and very pleasantly say that I don't feel comfortable with the conversation. If they were talking details and gossip, I would address it and definitely report it to supervisors. If it were a casual slip and vague in content, I would definitely report it to the supervisor if anyone else was on the elevator but if not, I would just address them directly."
"I encountered almost this same scenario, except it was two doctors that I recognized by sight but didn't know by name. I would handle this scenario in the same way I handled that situation. In that situation, I calmly said, 'Doctor, please don't discuss patient information in front of a person without a need to know this information.' The doctor nodded and said, 'Thank you,' and the conversation stopped. I think calmly and firmly reminding staff or physicians of a patient's right to privacy is the way to go, most of the time. If for some reason I saw a breach of confidentiality in front of a patient or visitor, I would report it to the unit manager in addition to my reminder to the staff."
43. You are working phone triage for your physician practice when a patient calls asking for advice as he is having chest pains. Tell me what you direct the patient to do.
In this situation there are multiple directions the nurse could give the patient, but in a situation when a patient is having chest pains, the patient should be directed to go to the emergency department. While care can be given at a physician office or urgent care center, a patient with chest pains could be in the midst of a medical crisis which requires the service of an emergency department. The interviewer is asking this question to determine if the candidate understands the clinical significance of chest pains and the fact that the patient needs to be evaluated in the emergency department. To effectively answer this question, the candidate should indicate that they would direct the patient to hang up and immediately go to the emergency department. A more successful answer to this question would include a specific example from the nurse's career where they directed a patient with chest pains to the emergency department.
"If a patient called with complaints of chest pains, I would tell them to go to the emergency department immediately after hanging up. Even though the patient's chest pains may not be from a heart condition, there is a chance that they could be, and an evaluation in an emergency department is necessary. In these situations, it is easy to assume the patient's symptoms or conditions may be caused by an ancillary condition, such as anxiety, but until they are properly evaluated, it is too risky to assume."
"When working phone triage, if a patient calls with chest pain, I would instruct him to go to the emergency department immediately. I would request verbal confirmation that the patient understands my instruction and will go to the emergency department immediately. Chest pain can indicate myocardial infarction, and delay in treatment can lead to heart failure or death. This isn't a time to take a chance that the chest pain might be caused by something else."
Situational
44. How would you handle a patient who is trying to manipulate you in some way or talks about the other shift to you?
This answer appears easy ,but it's not. Being a new nurse sometimes makes people over eager to please and hearing great things about yourself rarely falls on unappreciative ears. You want to help and be sympathetic, but it's not helpful to engage in any conversation that downgrades your coworkers in any way. Sometimes these conversations are subtle and sometimes they are not. The easiest way to circumvent these situations is to enter each room prepared and with a plan for the visit or encounter and perform that task in a professional and kind manner. If the patient begins to complain about another individual, handle it by stating that you're sorry they had the experience and ask if they'd like for you to get the nursing manager to speak to.
"If a patient starts to tell me something, I listen briefly and ask if she would like for me to get my nursing leader. I don't want to shut the patient down if she really had a bad experience, but I don't want to feed into it either and damage their view of my coworker. The best thing I can think of is to hear them out briefly but not agree. I'd say that I'm sorry they had the experience and ask if they would like me to get nursing leadership. Now if it's something horrible, of course I would report it directly, if it was a medical concern. It depends on the situation, but I know not to simply be silent because silence implies consent sometimes, so I would feel the need to say that I hear them, but I'm not the person who has the power to take action on that concern."
"When a patient has a legitimate complaint, I will attempt to rectify their problem myself or bring up their complaint to the charge nurse, the nurse manager, or another person in leadership. However, if a patient seems to be manipulative or complaining to try to start conflict, I usually use reflective listening. So, I reflect their statement back to them neutrally, such as saying, 'I hear you saying you were frustrated that the night shift nurse's aid didn't get you up to the chair at the time you wanted. What are the top 2 priorities I can address during my shift today to make you comfortable?' I don't feed into any negativity about another shift, and I focus on what I can do during my shift If the patient persists in complaining about something that happened earlier, I would offer to bring in my nursing manager."
45. If you have too many things on your to-do list, how to you decide which to do first and which to postpone?
A nurse shift is usually a very busy one, with few unimportant tasks. Taking the time to organize and frontload your day by doing the most important patient tasks first helps free up time later. Sometimes, it is helpful to delegate to others when possible, but it's never an acceptable answer if anything patient-care related is not done because there wasn't time. Future pace your day and sketch out a timeline for each activity. When you follow your plan and you realize at 10 AM that you are still dealing with some problems with your 8 AM task, then the best time to ask for support or help is at 10 AM. At 2 PM, it's too late to gather support and finish the shift completely and correctly.
"At work, I take a couple minutes to sketch out my day and I frontload the more important and difficult tasks in the morning, so I can complete them well. That gives me time to work through the rest of my shift, and if I end up having to ask for help, then the tasks that still need to get done are not the most difficult or important ones. In my personal life, when my to-do list gets too large, I sit down, weed it out, and focus on what moves my life forward and brings meaning and value."
"At the beginning of my shift, I use my shift 'cheat sheet' to help me organize and prioritize my day. This helps me determine which tasks should be done first, based on both how important they are and how long they might take. If tasks take longer than I anticipated, or I run into a situation where a patient's condition takes a downturn, I will need to ask for help. I can delegate tasks like blood glucose tests or a patient bath to a patient care tech. I can also ask my coworkers or the charge nurse to take on a task that only a nurse can do. In an inpatient unit, we have to work as a team to make sure all patient care tasks are completed. I am comfortable asking my colleagues for help because they know I always offer to assist them with tasks when I can."
46. What tools or techniques do you use to remember difficult information or instructions given verbally only?
Situational interview questions are designed to assess candidate competencies in more depth and to avoid rote, standardized answers. The interviewer is looking to observe how you would triage a problem and figure out how to handle it in an optimal way. Situational questions allow the interviewer to showcase unique talents and competencies. Situational interview questions challenge the interviewee to think about situations that they may have never experienced before.
"While I prefer to listen to instructions and have written instructions as well, I have a formula for remembering things verbally. I believe this is a good skill to have as a nurse. First, I listen to understand, and I listen attentively. I give the individual my full attention, particularly if it's new information. After I listen to them, I ask questions for clarity, and then I repeat back what they want me to do. Sometimes, I use imagery or acronyms to remember things when I am getting complicated directions."
"When I am given instructions verbally only, I repeat the information back to the source to ensure I have all of the information correct. Once the physician or other person has confirmed that I have all of the information correct, I break the steps down into sections or 'chunks' in my head, and then I repeat them to myself 5-7 times to ensure they stick. If there's an opportunity, I will also write down the instructions later; however, if there's not an opportunity, my chunking and repeating method works for me."
47. You are nearing the end of your 12-hour shift on your inpatient unit and you are exhausted from caring for eight high-acuity patients. As your colleague arrives to relieve you, tell me how you proceed.
When inter-shift information is involved, nurses must ensure that they properly handover information to their colleagues properly, even if this means they stay late to complete handover paperwork on each of their patients. Failing to properly handover information to the next nurse could have dire consequences to patients, making handovers a vital element of a nurse's set of responsibilities. Many facilities have standardized handover templates for nurses to complete before the end of their shifts, and these templates include elements such as: background, assessments, vitals, and recommendations. While many electronic health record systems pre-populate much of this information, it is imperative the remaining information is completed. The interviewer is asking this question to determine if the candidate understands the importance of completing handovers. To effectively answer this question, the candidate should indicate they would ensure handover information for all patients was completed before departing for the day. A more successful answer to this question would include an example from the candidate's nursing career where they ensured their handovers were completed despite being exhausted or dealing with other confounding factors.
"In this situation, even though I am exhausted, I would complete handover templates for all my patients, if I haven't already. This is especially true because you said the eight patients are high-acuity, which means there is a lot the next nurse needs to know about them. I could never leave my patients without completing handovers, because not only could I not leave my coworker in a bad situation, but I also don't want to put my patients at risk. Last week, I was in a similar situation, where I had been so busy that I didn't have time to complete handovers until my coworker arrived to relieve me. So, I stayed late and completed the templates for all my patients, despite the fact that I was tired and ready to go home."
"At shift change, it's so important to give a concise but thorough report to the oncoming nurse who will be caring for the patients I had during my shift. If these patients were high-acuity, that's all the more reason to make sure no important details are missed. I want to ensure the oncoming nurse has all of the information needed to provide safe care to our patients. I have a brief 'cheat sheet' that I keep for all of my patients throughout the shift. It keeps me on track for all of my patients' orders, vital signs, conditions, and charting. Therefore, regardless of how tired I am at the end of my shift, I have the information necessary to complete a safe handoff to my oncoming colleague or colleagues."
Amanda's Feedback
48. Your coworker forgot to sign off that she gave Tylenol as a PRN before she punched out and calls you from the car. She asks you to initial that it was given so nobody gives it again. What do you do?
It sounds like the right thing to do. After all, you don't want the patient to be given extra Tylenol, but you should never do this. It's illegal and forging the medical record. It's unethical and risks your nursing license. The correct thing to do is to write down the information about the dose and attach a sticky note to the MAR so that there is a visual reminder for the person administering medications. This information should be reported to the shift nurse manager and guidance received. Under no circumstances should the nurse sign off a medication that he or she did not administer.
"Sally, I'm sorry, but I'm not comfortable doing that. Thank you so much for calling and letting me know. I put a sticky note on the chart to remind myself of the time you gave the Tylenol and let Ruthann know, so we can follow her guidance. Call Ruthann tomorrow to figure out what you need to do about not signing that. Have a good night and drive safely!"
"Unfortunately, I can't sign off on a medication that you administered. That would put both of our licenses at risk. Do you have time to come back in and chart it yourself? If not, I will place a sticky note on my nurse cheat sheet to remind me what time you administered the Tylenol. Make sure you check with the manager tomorrow to see how you can chart a late entry. Good night!"
49. Have you ever caught a coworker stealing? If so, how did you handle it? If not, what would you do if you saw a colleague stealing?
Interviewers ask what you would do if you saw a colleague stealing for a few reasons. First, they want to gauge your sense of ethics and integrity. Nurses are held to high standards of moral and ethical conduct, and it is important to ensure the people working in this field meet these standards. Second, they want to see how you would handle a difficult workplace situation. It can be challenging to confront a colleague about unethical behavior, and interviewers want to know that you would handle the situation appropriately and professionally. Ultimately, it is essential to prioritize patient care and safety and to take action if you witness any behavior that could compromise these priorities.
"No, I have never caught a coworker stealing. However, if I witnessed such behavior, I would first approach my colleague privately and confront them about what I had seen. I would explain that stealing is unethical and illegal and that their actions could have serious consequences for both themselves and our workplace. Depending on their response and the hospital's policies, I would escalate the issue to our supervisor or HR department if necessary. As healthcare professionals, we are responsible for acting with integrity and honesty and holding our colleagues accountable when they fall short of these standards."
"Yes, unfortunately, I have witnessed a coworker stealing. When doing my rounds, I walked into a patient's room and saw a nurse's aide quickly put something from the patient's bedside table into their pocket. After checking on my patient, I asked the aide to speak privately with me outside the room. I asked what they put into their pocket, and they said they had not taken anything. I asked to look in their pocket, and they refused. Since I was sure the aide had taken something from the patient, I reported what I saw to the charge nurse. After an investigation, it was discovered the aide had a problem with prescription pills and had taken the patient's medications. Those who work with me understand my values and that I do not condone stealing of any kind."
50. How do you handle ethical or philosophical differences with a patient?
Nurses care for all patients, so they must have emotional mastery and cultural competence. It's difficult sometimes to separate our personal preferences and philosophies from our patients and not superimpose our cultural grid on their choices and feel disapproval. It is unprofessional and not optimal patient care to do so. Nurses must remind themselves when they enter the door to a patient's room that they do not need to know the whole story, and they can never know all the nuances that led to the belief or decision they disagree with. They must lead themselves to treat the individual in front of them as a human being who they are there to help, serve, and not to judge.
"When I feel judgement or disapproval welling up inside me, I do a quick mental inventory and check-in. It doesn't happen often, but I would not be human if I said it never has or will again. I don't know why the person made the choices they made, or what led up to it. I only know that my job is to help them, and I stay focused on that. I've worked with drug addicts and criminals, but my job is to be kind, provide excellent care, and maybe even learn something from them."
"In two of the hospitals I've worked out, I've taken care of prisoners that are recovering from heart surgery. I've never looked up or asked a patient what crime they are in jail for, but some have volunteered this information to me, and it can be momentarily disconcerting to learn that you're taking care of a person who has committed an assault. However, I know that all patients deserve safe and effective care. I can never know anyone's full story, so regardless of the circumstances, I provide my best care to all patients."
About the Author
I began my career in emergency medical services (EMS) over 30 years ago, working as a Firefighter-Paramedic, EMS Captain, Mental Health Technician, ER Technician, EMT and Paramedic Adjunct Instructor, and EMS Educator. During my career, I had the privilege of serving on over one thousand interview panels to help various organizations choose the right candidate for the job. I have created curricula and training materials to prepare candidates for interviews and held mock interview courses for all types of healthcare professionals. My interview experience includes hiring emergency medical technicians, paramedics, firefighters, nurses, medical assistants, home health aides, and physician assistants. As a coach and contributor for MockQuestions, I am excited to help you navigate your upcoming nursing interview. While these situational questions assess your critical thinking and communication skills, interviewers also ask these questions to gain insight into your personality to determine if you will be a good fit with the company culture. Remember to be relaxed and be your authentic self. Best of luck in nailing your interview!
Learn more about Krista Wenz
.png)
Six exercises for nurses to foster critical thinking
- Publish Date: Posted almost 5 years ago
- Author: by Kate Andrews
As a nurse, no matter what organization you work within, the ability to resolve issues before they turn into problems is crucial to ensure success in your role.
To prepare for your next nursing position, we detail some fundamental critical thinking exercises that can help develop those all-important problem-solving skills.
What is critical thinking?
During your nursing studies, you will have undoubtedly come across the term ‘critical thinking’. It is the process of applying intentional higher-level thinking to describe a patient’s problem and examining the evidence-based practice in caring for them to make the right choices on the type of care that they require.
Fostering the right attributes and attitude that encourages critical thinking will help you excel in your nursing role and develop your career long into the future. These include:
The confidence to challenge convention
By nature, the nursing profession is driven by process and best practice, but sometimes the opportunity arises for individuals to enrich and change the way that things are done. This does not mean you have to upset the system, but simply that you should be confident enough to speak up and be afforded the opportunity to improve upon existing workplace practices.
Working independently
When you embark upon your career in nursing, you are likely to work under close supervision; however, certain situations may arise where there is an opportunity for you to work independently. If you have a particular skill-set or interest in a niche area, why not ask to take ownership? Not only will this demonstrate initiative and your willingness to develop in your profession, but it also improves your critical thinking skills too.
Practical experience
Practical, hands-on experience is crucial to excelling in any nursing role. Developing critical-thinking skills starts at the beginning of your career, not just in your first position but also the experience you obtain while studying. Anyone will tell you that gaining essential and varied work experience will help you secure the role that you deserve.
Working alongside leaders
There is a lot to be said about great leadership. Learning from senior nurses, not only on the job but also enquiring about their past experiences, mistakes, and learnings will help you to develop your critical thinking skills in any role.
Situational analysis
Continued professional development is a vital part of career success. It is not uncommon to be tested on what you have learned in your job. Commonly senior staff nurses may create hypothetical situations to test your critical thinking and development since starting your position. If this is not a common practice in your place of work, it is always worth asking for more training to ensure your nursing aptitude and critical thinking skills continue to evolve.
Existing case studies
Any nurse should brush up on their skills by reading case studies. These can be found in academic books or learning from a vast breadth of academic papers from established educational institutions, which are often accessible online.
Our experienced team helps to place the very best international nurses and US-based overseas graduates that have the desire to work in the US. We partner with leading healthcare organizations across 25 states who are committed to ethical, best practice long-term care nursing through practical training and development. At Conexus Medstaff, we’re passionate about building healthcare careers in the US. We’re keen to help graduates (and experienced nurses) from overseas embark on a career in nursing in America. To help you recognize what to expect from a career in long-term care nursing, download our free Conexus MedStaff Guide to Long-Term Care Nursing Careers today.
- Login / Register

‘Sport has the power to unite people in a way that is almost unique’
STEVE FORD, EDITOR
- You are here: Archive
Thinking your way to successful problem-solving
13 September, 2001 By NT Contributor
VOL: 97, ISSUE: 37, PAGE NO: 36
Jacqueline Wheeler, DMS, MSc, RGN, is a lecturer at Buckinghamshire Chilterns University College
Problems - some people like them, some do not think they have any, while others shy away from them as if they were the plague. Opportunities, in the form of problems, are part of your life.
The most difficult decision is deciding to tackle a problem and implement a solution, especially as it is sometimes easier to ignore its existence. Problem-solving takes time and effort, but once a problem has been addressed the nurse can feel satisfied that the issue has been resolved and is therefore less likely to re-emerge.
Nurses make clinical decisions using two different approaches. The first is the rationalist approach, which involves an analysis of a situation so that subsequent actions are rational, logical and based on knowledge and judgement. The second approach is based on a phenomenological perspective, where a fluid, flexible and dynamic approach to decision-making is required, such as when dealing with an acutely ill patient.
Types of problems
Problems come in different guises and the solver can perceive them either as a challenge or a threat. One of the most common types of problem is when the unexpected happens. As a nurse you plan and implement care for a patient based on your knowledge and experience, only to find that the patient’s reaction is totally different from that expected but without any apparent reason.
Another type of problem is an assignment where others set a goal or task. Throughout your working life you will be required to undertake duties on behalf of other people. For some this is difficult as they feel unable to control their workload. Others see it as an opportunity to develop new skills or take on additional responsibilities. Opportunities can be perceived as problems by those who fear failure.
A third type of problem is when a dilemma arises. This is when it is difficult to choose the best solution to a problem because the nurse is confronted with something that challenges his or her personal and/or professional values.
Diagnosing problems
The sooner a problem is identified and solutions devised, the better for all involved. So try to anticipate or identify problems when they occur through continuously monitoring staff performance and patient outcomes.
Listening to and observing junior staff will help you to detect work or organisational concerns, because when there are problems staff are likely to behave in an unusual or inconsistent manner.
Initial analysis
Remember that people view things differently, so what you perceive as a problem may not be one to anyone else. So before you begin thinking about what to do - whether to keep it under surveillance, contain it or find a solution - you should undertake an initial analysis. This will help you to understand the problem more clearly.
An analysis will also enable you to prioritise its importance in relation to other problems as problems do not occur one at a time.
Routine problems often need little clarification, so an initial analysis is recommended for non-routine problems only. Even then, not all problems justify the same degree of analysis. But where it is appropriate, an initial analysis will provide a basis from which to generate solutions.
Perception is also important when dealing with patients’ problems. For example, if a patient gives up reading because he or she cannot hold the book (objective), the nurse may assume it is because the patient has lost interest (subjective, one’s own view).
Generating solutions
It is essential for the problem-solver to remember that, where possible, solutions must come from those connected with the problem. If it is to be resolved, agreement must be owned by those involved as they are probably the best and only people who can resolve their differences. The manager should never feel that he or she must be on hand to deal with all disputes.
To solve a problem you need to generate solutions. However, the obvious solution may not necessarily be the best. To generate solutions, a mixture of creative and analytical thinking is needed (Bransford, 1993).
Creativity is about escaping from preconceived ideas that block the way to finding an innovative solution to a problem. An effective tool for assisting in this process is the technique of lateral thinking, which is based largely on the work of Edward de Bono, who regards thinking as a skill.
There are several ways to encourage creative decision-making. One method that works best for specific or simple problems is brainstorming. If the ground rules of confidentiality and being non-judgemental are applied, it will produce a free flow of ideas generated without fear of criticism (Rawlinson, 1986).
Time constraints and staff availability may make it difficult for all those involved in a problem to meet. In such cases an adaptation of brainstorming - where a blank piece of paper is given to those involved and each writes down four solutions to the problem - may be the answer. A similar technique is the collective notebook, where people are asked to record their thoughts and ideas about a problem for a specified period.
An alternative is where one person writes down a list of solutions in order of priority, which is then added to by others. This helps to prioritise the ideas generated. All these methods produce data that can then be analysed by the problem-solver.
When the problem affects people in different geographical areas, solutions can be generated by obtaining the opinion of experts through the use of a questionnaire, which is known as the Delphi technique (McKenna, 1994).
When an apparently insurmountable problem presents itself, it is often useful to divide it into smaller pieces. This is known as convergent thinking. Using divergent thinking - where you consider a problem in different ways to expand your view - may also help.
A final alternative is the stepladder technique, which is time-consuming but effective if the issue is stirring up strong feelings. This requires the people involved in the problem to be organised into groups. First, two people try to solve the problem, then a third member is drawn in, to whom the solution reached by the first two is presented. All three then try to agree a solution. More people are added to the group, if necessary, in a similar way, until there is agreement of all involved. Provided the individuals are motivated to solve the problem, this technique creates ownership and commitment to implementing the agreed solution.
Analytical thinking, which follows a logical process of eliminating ideas, will enable you to narrow the range down to one feasible solution.
Although someone has to make the ultimate decision on which solution to implement, there are advantages to group decision-making: a greater number of possible solutions are generated and conflicts are resolved, resulting in decisions being reached through rational discussion.
This does, however, require the group to be functioning well or the individuals involved may feel inhibited in contributing to the decision-making. One individual may dominate the group or competition between individuals may result in the need to win taking precedence over deciding on an agreed practical solution.
As nursing becomes less bureaucratic individuals are being encouraged to put forward their own ideas, but social pressures to conform may inhibit the group. We do not solve problems and make decisions in isolation, but are influenced by the environment in which we work and the role we fulfil in that environment. If group members lack commitment and/or motivation, they may accept the first solution and pay little attention to other solutions offered.
Making a decision
There are three types of decision-making environments: certain, risk and uncertain. The certain environment, where we have sufficient information to allow us to select the best solution, is the most comfortable within which to make a decision, but it is the least often encountered.
We usually encounter the risk environment, where we lack complete certainty about the outcomes of various courses of action.
Finally, the uncertain environment is the least comfortable within which to make decisions as we are almost forced to do this blind. We are unable to forecast the possible outcomes of alternative courses of action and, therefore, have to rely heavily on creative intuition and the educated guess.
Taking this into consideration, you should not contemplate making a decision until you have all the information needed. Before you make your decision, remind yourself of the objective, reassess the priorities, consider the options and weigh up the strengths, weaknesses, opportunities and threats of each solution.
An alternative is to use the method that Thomas Edison used to solve the problem of the electric light bulb. Simply focus on your problem as you drift off to sleep, and when you wake up your subconscious mind will have presented you with the answer. But bear in mind that this is not a scientific way of solving problems - your subconscious can be unreliable.
If you are not sure about your decision, test the solution out on others who do not own the problem but may have encountered a similar dilemma. Once you have made your choice stick to it, or you may find it difficult to implement because those involved will never be sure which solution is current. They will also be reluctant to become involved in any future decision-making because of your uncertainty.
The next step is to ensure that all the people involved know what decision has been made. Where possible, brief the group and follow this up with written communication to ensure everyone knows what is expected of them. You may need to sell the decision to some, especially if they were not involved in the decision-making process or the solution chosen is not theirs.
Implementing the solution
Finally, to ensure the solution is implemented, check that the people involved know who is to do what, by when and that it has happened. Review the results of implementing your solution (see Box) and praise and thank all those involved.
- Part 1 of this series was published in last week’s issue: Wheeler, J. (2001) How to delegate your way to a better working life. Nursing Times; 97: 36, 34-35.
Next week. Part three: a step-by-step guide to effective report writing.
- Add to Bookmarks
Have your say
Sign in or Register a new account to join the discussion.
Find Study Materials for
- Explanations
- Business Studies
- Combined Science
- Computer Science
- Engineering
- English Literature
- Environmental Science
- Human Geography
- Macroeconomics
- Microeconomics
- Social Studies
- Browse all subjects
- Read our Magazine
Create Study Materials
- Flashcards Create and find the best flashcards.
- Notes Create notes faster than ever before.
- Study Sets Everything you need for your studies in one place.
- Study Plans Stop procrastinating with our smart planner features.
- Problem Solving in Nursing Management
Dive deep into the multifaceted world of nursing management with a special focus on problem-solving. This comprehensive guide presents a detailed look at the process, importance, and challenges of problem-solving in nursing management. By highlighting essential skills, neurologically based frameworks, and the relationship with decision-making, it offers both theoretical understanding and practical solutions. Explore real-life case studies, leadership's role, and the link with critical thinking. This is an enriching journey towards developing strategic competencies and achieving effective problem-solving in a vital healthcare sector.
Create learning materials about Problem Solving in Nursing Management with our free learning app!
- Instand access to millions of learning materials
- Flashcards, notes, mock-exams and more
- Everything you need to ace your exams
- Clinical Placement
- Human Anatomy
- Intensive Care Nursing
- Mental Health Nursing
- Nursing Management
- Antimicrobial Stewardship
- Audit Compliance Nursing
- Billing Practices for Hospitals
- Biohazard Management
- Budget Management
- Budget Planning
- Capital Resources
- Care Evaluation
- Clinical Pathways
- Communication Skills
- Crisis Management
- Customer Service in Nursing
- Delegation of Nurses
- Disinfection Techniques
- Emergency Drills
- Emergency Preparedness
- Expense Management
- Financial Management in Nursing
- Fiscal Responsibility
- HIPAA Compliance
- Hazard Identification
- Healthcare Technology
- Hospital Asset Management
- Hospital Contract Negotiation
- Hospital Funding Sources
- Hospital Revenue Cycle
- Hygiene Protocols
- Insurance Relations Hospitals
- Interdisciplinary Team
- Labor Relations
- Nurse Staff Training
- Nursing Data Analysis
- Nursing Grant Writing
- Nursing Scheduling
- Operational Efficiency
- Patient Flow
- Patient Loyalty
- Reimbursement Strategies
- Retention Strategies
- Revenue Generation
- Sanitation Practices
- Staff Development
- Staffing Models
- Staffing in Nursing
- Stakeholder Engagement
- Strategic Planning in Nursing
- Time Management
- Waste Disposal in Hospital
- Worker Safety
- Workforce Planning
- Workplace Harmony
- Nursing Theories
- Types of Nursing
Understanding Problem Solving in Nursing Management
Problem solving in nursing management is a crucial process that you need to grasp as a prospective or current nurse. This involves using a logical, systematic approach to resolving issues encountered in a nursing environment, focusing on maintaining quality patient care .
Problem Solving: This is identifying and overcoming obstacles to achieving a goal. In nursing, this generally revolves around improving patient health outcomes and ensuring efficient healthcare facility operations.
Importance of Problem Solving in Nursing Management
Nursing professionals are constantly faced with intricate issues that require decisive and effective solutions. The ability to implement problem-solving is crucial in maintaining optimal patient care , operational efficiency , and fostering team collaboration.
For instance, suppose a sudden shortage of resources like catheters or syringes is experienced in a healthcare facility. In such a case, the nursing manager will need to swiftly solve the problem either by reallocating resources, timely ordering supplies, or finding a temporary alternative, ensuring the patients' needs are continually met.
Key Skills Required for Problem Solving in Nursing Management
Effective problem-solving in nursing management is anchored on a set of key skills. These abilities equip you to navigate complex situations and formulate impactful solutions. They include:
- Critical Thinking: This is your ability to analyse situations in detail and understand their implications.
- Decisiveness: The readiness to make important decisions swiftly and confidently.
- Communication: Sharing and receiving information clearly and effectively.
- Collaboration: Working effectively as part of a team.
These skills are interconnected. For example, your ability to think critically informs your decisiveness. Your decisions are then made clear to your team through effective communication, and together, through collaboration, the problem is solved.
Common Challenges in Problem Solving in Nursing Management
In your nursing management journey, you will come across multiple challenges when attempting to solve problems. These obstacles might occur due to several factors, such as resource limitations, personnel issues, and complex patient needs .
| Resource Constraints | Shortage of essential medical supplies or understaffing. |
| Personnel Issues | Conflicts among team members or unforeseen absence of staff. |
| Complex | Patients with rare medical conditions that require specialized care. |
While these challenges can be daunting, equipping yourself with robust problem-solving skills will help you navigate these complications and maintain high standards of patient care.
Scrutinising the Problem Solving Process in Nursing Management
Delving deeper into the problem-solving process in nursing management, you get to navigate its intricacies and mechanisms. This exploration can bolster your abilities to resolve complex situations in your nursing career.
Steps involved in the Problem Solving Process
Problem-solving in nursing management is a multifaceted task that often involves several steps. To understand how to tackle issues expertly, you will need a clear understanding of each stage.
Problem-Solving Process: A systematic approach used to address complications and make decisions. In nursing, it’s composed of several steps, each essential to the resolution of issues.
Here are the key steps:
- Identification: In this stage, you recognise the existence of a problem. It is essential to understand the barriers to your goals and spotlight areas that require improvement.
- Definition: You clearly articulate the problem. By understanding its nuances, magnitude, and implications, you can efficiently tailor a solution.
- Analysis: This involves examining the problem closely from different perspectives, which includes understanding the cause and effect, stakeholders involved, and potential impacts.
- Development of Solutions: Here you brainstorm possible solutions. It's essential to contemplate multiple alternatives to ensure the most effective resolution is chosen.
- Decision Making: In this step, you select the best solution based on the gathered information and analysis. Considerations may include effectiveness, resources needed, and potential side effects.
- Implementation: You put the chosen solution into action, carefully monitoring its effectiveness and making necessary adjustments.
- Evaluation: Finally, you assess the outcome. This helps to determine the effectiveness of your solution and informs future problem-solving efforts.
Neurological Framework for Problem Solving in Nursing Management
Many problem-solving methods exist, but one valuable perspective is through understanding the neurological framework in nursing management. This biological approach delves into how your brain processes information and develops solutions.
Neurological Framework: A biological perspective that explains how a nurse's brain processes, analyses, and responds to problems encountered in the nursing environment.
This framework refers to cognitive processes which involve:
- Critical thinking: This involves actively and skillfully conceptualising, applying, analysing, and evaluating information gathered from observation, experience, reflection, or communication.
- Decision making: This is the cognitive process of selecting a course of action from multiple possibilities. It's based on both intuition and logical reasoning.
- Problem-solving: This involves overcoming hurdles and finding a conclusion, and it usually includes decision-making. It involves creativity and critical thinking to arrive at effective solutions.
Role of Creativity in the Problem Solving Process
Nursing management often involves complex and unique problems. To effectively tackle these challenges, it's crucial to breed creativity in the problem-solving process.
Imagine there's a sudden surge in patient intake due to a local health crisis, resulting in a bed shortage. A creative solution might be to convert other non-critical spaces such as conference rooms temporarily into patient monitoring units, thereby managing the surge effectively.
Importance of Team Collaboration in the Problem Solving Process
In a nursing environment, you are not working in isolation. Collaboration is a critical aspect of problem-solving in nursing management, as diverse insights can lead to innovative and effective solutions.
Consider a scenario where there's a need to implement a new system for managing patient records. To effectively solve potential issues in system implementation, you might need input from various team members including nursing staff, IT specialists, and data management experts. Each member's contribution, based on their expertise and perspective, is crucial in charting a comprehensive problem-solving strategy, ensuring the successful implementation and integration of the new system.
Decision Making and Problem Solving in Nursing Management
Decision making and problem-solving are two interconnected aspects in the realm of nursing management. Understanding their correlation and distinctiveness is key to effectively managing issues and improving patient outcomes in a healthcare setting.
The Interplay between Decision Making and Problem Solving
The connection between decision making and problem solving in nursing management is truly significant. In almost every situation where a problem arises, decision making is an inseparable component of the problem-solving process.
Decision Making in Nursing: This involves selecting a course of action from different alternatives. It is the bridge connecting problem analysis with implementing solutions, and it requires evaluation of information, predicaments, and possible outcomes.
Once you have identified and defined a problem, analysed it, and developed potential solutions, the next step involves decision making. This is where you select the most suitable solution among the alternatives.
For instance, if you are dealing with a bed shortage problem in your healthcare facility, some possible solutions could be outsourcing to other healthcare facilities, using other spaces such as conference rooms as makeshift wards, or deploying portable hospital beds.
Each of these solutions has its pros and cons, and it's here that decision-making skills come into play. You'll need to compare and contrast each option, considering factors like cost, time, resources available, and the overall impact on patient care. The chosen solution is then implemented, and the effects are evaluated for future reference.
Distinguishing Decision Making from Problem Solving in Nursing Management
Though inherently connected, problem solving and decision making are distinct processes within nursing management. Where problem-solving is a comprehensive process that entails identifying, analysing, and solving issues, decision making is a component nested within this process, acting as the transition point from analysis to action.
Problem Solving in Nursing: This is a broader process involving the identification of an issue or obstacle, systematic analysis to understand it, devising potential solutions, choosing the most suitable through decision making, implementing it, and finally reviewing the effectiveness of the implemented solution.
Consider a real-life scenario such as medication errors. If these errors are occurring frequently in your healthcare setup, the problem-solving process will involve identifying the issue (increased medication errors), defining and analysing it (finding the root causes, such as miscommunication or system glitches). This would then lead to brainstorming potential solutions, like improved communication systems or enhanced employee training. The decision-making process would then come into play when choosing the best solution to implement.
Techniques for Effective Decision Making in Problem Solving Scenarios
Effective decision making underpins successful problem solving in nursing management. Implementing the right techniques can enhance your decision-making process, thus leading to more effective problem resolution.
Some proven techniques include:
- Pros and Cons Analysis: List the advantages and disadvantages of each solution to help you visualise the impacts of each decision.
- Decision Matrix: Establish criteria and rate potential solutions. The choice with the highest score is then considered the best decision.
- Cost-Benefit Analysis: Determine the financial implication of each decision and compare it to the benefits. Solutions with a high benefit-cost ratio are preferred.
Working collaboratively to brainstorm and analyse solutions promotes critical thinking and creativity, ensuring that the chosen solution maximises the use of resources and improves patient outcomes .
In unavoidable circumstances where decisions have to be made rapidly and with limited information, using intuition, a nurse's experience, and insights combined with analytical thinking can be beneficial. This is where the balanced blend of clinical expertise and effective risk-taking come into play.
Decision making is never static in nursing management. The cyclic nature of the decision-making process, where outcomes of decisions are continually assessed and feedback is used to improve future decision making, showcases its dynamic and iterative nature. This reinforces the vital role decision making plays in the problem-solving process.
Unpacking Examples of Problem Solving in Nursing Management
By exploring various examples and case studies, you gain a practical view of problem-solving in nursing management. These insights can better equip you to tackle real-life challenges in a healthcare setting.
Case Study Analysis of Problem Solving Scenarios
Case studies provide a thorough view of how problem-solving strategies are applied in various nursing management scenarios. Analysing such cases exposes you to diverse methods and solutions and encourages you to think critically and innovatively.
Case Study Analysis: A detailed examination of a particular instance or event to draw conclusions, develop solutions, or learn from the situation.
Let's investigate a case concerning patient waiting times. In a healthcare facility, it is observed that patients often have to wait for prolonged periods to receive care, leading to dissatisfaction and affecting the overall quality of service. The problem-solving steps might look like this:
- Identification and Definition: The problem is identified as long patient waiting times. It is defined as patients waiting more than 45 minutes to receive care.
- Analysis: The cause of the problem is found to be a shortage of nursing staff during peak hours.
- Development of Solutions: Several possible solutions emerge, such as recruiting additional staff, offering overtime to existing staff, or streamlining operational processes to reduce inefficiencies.
- Decision Making: After careful analysis, it is decided to hire additional part-time staff to handle peak hours.
- Implementation: The recruitment process is initiated and new members integrated into the team.
- Evaluation: After a few months, waiting times are reassessed. A significant reduction is observed, confirming the effectiveness of the solution.
Case study analysis provides a rich source of knowledge and transferable insights that can be helpful in similar or entirely different scenarios. Drawing parallels from varying contexts and understanding how solutions are adapted to unique situations helps bolster your problem-solving skills and adaptability in nursing management.
Varied Approaches to Problem Solving in Different Nursing Scenarios
Different nursing scenarios call for diverse problem-solving strategies. Understanding the varying approaches, from algorithm-based to intuition-driven, equips you to manage multidimensional and intricate issues effectively.
Algorithm-based Approach: This involves following a clearly defined set of rules or procedures to solve a problem. It can be applicable in situations with defined parameters and scope, such as diagnosing a health condition based on a specific set of symptoms.
Intuition-driven Approach: This combines a nurse's experience, knowledge, and instinct to solve a problem. It applies to ambiguous scenarios where conventional rules may not be applicable, such as managing a patient's fear or anxiety.
Problem-solving in nursing management is all about adapting to the environment and the situation. The right approach may vary, calling for flexibility, creativity, critical thinking, and a deep understanding of the issue for successful resolution.
Real Life Applications of Problem Solving Strategies in Nursing Management
The real world of nursing is complex and dynamic, and various problem-solving strategies can apply on any given day. To navigate smoothly, you need to understand how the various approaches can be adapted to specific situations.
Consider solving a recurrent communication issue within your nursing team. The algorithmic approach might involve establishing clear communication protocols or using digital tools to streamline interaction. However, the intuition-driven approach might involve informal team-building meetings to foster better personal connections. In this situation, the best solution might be a blend of the two approaches to ensure both procedural clarity and improved team relationships.
The key takeaway here is that there is no "one-size-fits-all" solution in nursing management. Problem-solving requires flexibility, openness, and the ability to judge which strategy will perform best in a particular scenario.
Exploring Nursing Management Problem-Solving Strategies
Problem-solving strategies in nursing management form the backbone of effective healthcare services. By ensuring that nursing personnel can tackle issues with aplomb and proficiency, these strategies contribute significantly to patient satisfaction and positive outcomes.
Development of Strategic Problem-Solving Competencies
The first step towards demystifying problem-solving processes in nursing management is the development of strategic problem-solving competencies. The journey from novice to expert involves honing these skills and integrating them into your practical work.
Strategic Problem-Solving Competencies: These are a set of core skills that facilitate effective problem-solving in nursing management, including critical thinking, innovative thinking, collaboration, adaptability, leadership, and decision-making.
Acquiring these skills involves both academic learning and practical experiences. Gaining theoretical knowledge lays the foundation, while integrating this knowledge within a clinical context enriches and refines these competencies.
- Critical Thinking: This involves analysing situations from multiple perspectives, evaluating different solutions, and making informed decisions.
- Innovative Thinking: Innovative thinking pertains to thinking outside the box, especially when conventional solutions are inadequate.
- Collaboration: In nursing, effective problem-solving often requires collaborative efforts, valuing diverse ideas and working towards common goals.
- Adaptability: Healthcare settings are continually changing, and the ability to swiftly adapt to new situations is crucial.
- Leadership: Good leadership skills facilitate effective management of teams and ensuring that everyone is following the established problem-solving process.
- Decision Making: Ability to implement effective decisions is vital for successful problem solving.
Role of Leadership in Implementing Problem Solving Strategies
The role of leadership in implementing problem-solving strategies must not be understated. Effective leadership not only guides teams through problem-solving processes but also fosters a supportive environment where team members feel safe to contribute ideas and question assumptions.
Leadership in Nursing: This involves guiding, motivating, and supporting nursing staff to deliver quality healthcare services. Also, it encompasses enhancing team cooperation, improving communication, and fostering a culture of continuous learning.
Leadership employs a variety of approaches in implementing problem-solving strategies. Different leadership styles can be applied based on the nature of the problem and the team dynamics. Transformational leadership, for instance, inspires others to exceed their personal goals and work for a collective purpose. On the other hand, participative leadership encourages open discussions and collective decision-making, promoting a more inclusive and democratic problem-solving process.
Leadership is also instrumental in creating an environment that encourages the sharing of problems openly, without fear of judgment, hence facilitating early identification and efficient resolution of issues. By also ensuring that learning opportunities are provided to enhance team problem-solving capabilities, leadership positively influences problem-solving outcomes.
Use of Resources in Problem Solving Strategies
Effective resource utilization is a critical component of successful problem-solving strategies in nursing management. The term 'resources' in this context includes human resources such as nursing staff and doctors, as well as material resources like medical supplies, equipment, and facilities.
Resource Utilisation: This refers to the efficient and effective use of available resources to achieve desired outcomes. In nursing, it involves ensuring that staff, equipment, and supplies are optimally used to deliver quality healthcare services and solve arising problems.
Problem-solving often necessitates the optimal use of available resources. For example, if there is an issue of high patient-to-nurse ratio, one of the possible solutions could be redistributing nursing staff according to workload and patient needs, or hiring additional staff if finances permit.
Every solution should be weighed based on its resource implications. The best solution is often the one that optimally utilises available resources to provide the maximum benefit. For example, while hiring additional staff might solve the problem, it might not be the best solution if the budget is very limited. In such a case, reallocation of existing staff may be a more practical solution.
Similarly, if there is a shortage of a particular supply, then alternatives may need to be sought, or rationing implemented. A critical analysis of such situations is necessary to ensure that the solutions proposed and implemented do not create other problems related to resource allocation and use.
It's also important to remember to continuously evaluate the impact of your solutions on resource utilisation. This will not only help you ensure sustainable use of resources but also contribute to continuous improvement in problem-solving strategies.
Understanding the stages of problem-solving in nursing practice is fundamental to addressing various challenges that arise in the healthcare sector. These problem-solving stages enable you to identify issues, create and implement solutions, and review the outcomes for improvement purposes.
Initial Assessment and Identification: The First Stage of Problem Solving
The initial phase of problem-solving in nursing management involves the assessment and identification of the issue at hand. This stage is critical as the correct identification of the problem lays the foundation for effective solution design and implementation.
Initial Assessment: This is the preliminary evaluation of the situation, leading to the recognition of existing problems. This stage involves observation, questioning, and data gathering to understand the issue better.
This initial step requires keen observation skills and critical thinking. While observation helps in gathering relevant details, critical thinking enables you to scrutinize this information and identify potential problems. You could also use feedback from your team and other relevant stakeholders to gain a comprehensive understanding of the issue.
For instance, suppose you discover unusually high levels of patient discomfort during specific hours. The initial assessment might involve examining patient records during these hours, observing nursing practices in these time frames, and seeking feedback from both patients and nursing staff. This comprehensive approach could potentially reveal the issue, like a shortage of staff during peak hours, leading to delayed or inefficient care.
Formulating Actionable Solutions: The Mid Stages of the Problem-solving Process
Once the problem is identified, the next phase is generating actionable solutions. The validity and effectiveness of these solutions significantly influence the problem-solving process's success, thus necessitating careful deliberation and thorough evaluation.
Actionable Solution: A practical, feasible strategy that can be implemented to resolve the problem. It's typically developed through brainstorming, analysis, and evaluation of various alternatives.
The process of formulating actionable solutions involves brainstorming potential remedies, evaluating these against a set criteria, and choosing the most viable option. Ideally, this should be a collaborative effort involving all relevant stakeholders. Collaborative problem-solving encourages diversity in ideas and promotes inclusivity.
| Careful Analysis | Evaluation Against Set Criteria | Choosing Viable Option |
| Gather as many potential solutions as possible through brainstorming sessions | Evaluate potential solutions based on criteria such as feasibility, efficiency, and impact | The most suitable solution is chosen after careful evaluation |
Innovation is a key driver in formulating actionable solutions. Traditional problem-solving methods might fail in the face of complex or unique problems, necessitating innovative ideas. Remember, the most effective solutions often result from 'thinking outside the box'.
Evaluation and Reflection: The Final Stage of Problem Solving
The final stage of problem-solving is evaluation and reflection. After implementing the chosen solution, it is essential to assess its effectiveness in solving the identified problem. This stage offers an opportunity to learn from the implemented action and make necessary adjustments for future improvement.
Evaluation and Reflection: This stage involves reviewing the implemented solution to assess its effectiveness. Reflection involves learning from the process and experiences to ensure continuous improvement.
To achieve meaningful evaluation and reflection, a systematic approach must be adopted. Begin with the assessment of the effect of the solution on the original problem. Have the waiting times reduced following the staff adjustments? Is there an improved level of patient comfort? These are the kind of questions you need to address.
Following the evaluation, it's crucial to reflect on the entire process. Consider what worked well and what didn't. Reflecting on these experiences offers valuable insights that can be used to improve future problem-solving processes.
Take the earlier example of high levels of patient discomfort due to staff shortage during peak hours. Suppose, after implementing the solution of adjusting staff schedules, you find that there's a significant improvement in patient comfort levels. This shows that your solution worked. However, during reflection, you realise that the process took more time than necessary due to delayed decision-making. For future improvement, you could consider setting specific timelines for each stage of the problem-solving process.
In conclusion, problem-solving is a cyclical process. It doesn't end with implementing a solution; instead, it opens doors for continuous learning and improvement. Adapting to this cycle is key to honing your problem-solving proficiency in nursing management.
Critical Thinking and Problem Solving in Nursing
Problem solving in nursing management is underpinned by the practice of critical thinking. An understanding of the delicate interplay between these two capabilities is central to the enhancement of nursing management and the ultimate delivery of efficient patient care.
The Connection Between Critical Thinking and Problem Solving in Nursing
There is a strong relationship between critical thinking and problem solving in nursing, evidenced by the significant role each plays in the healthcare sector. Critical thinking provides the foundation upon which problem-solving strategies are built.
Critical Thinking: This is the disciplined process of analysing, interpreting, evaluating, and drawing conclusions from varying levels of data, information or experiences. It involves a deeper level of thinking to understand, evaluate and resolve complex issues or situations.
The process of problem-solving often begins with an evaluation of the situation, gathering data, appraising the data, and coming with strategic solutions. By applying critical thinking, you can get a clear understanding of the problem, which helps devise more effective solutions.
For example, in implementing new protocols in a nursing unit, critical thinking may involve evaluating the necessity of the change, the potential effect on the nursing staff’s workflow, and patient care. The ability to think critically facilitates well-informed decisions, thereby enhancing the problem-solving process.
Beyond problem identification and solution generation, critical thinking is also instrumental in the review phase of the problem-solving process. It allows you to reflect on the effectiveness of implemented solutions, the overall process, and areas that could be improved. Therefore, the integration of critical thinking not only enriches problem-solving but also contributes to continuous learning and improvement in nursing management.
Enhancing Critical Thinking for Effective Problem Solving in Nursing Management
Enhancing critical thinking skills in the nursing workforce enriches problem-solving efforts and ultimately results in improved patient outcomes and service delivery. This strengthening could be achieved through several strategies.
Enhancing Critical Thinking: The process of improving critical thinking skills to enhance one's ability to evaluate complex situations effectively and make informed decisions.
Firstly, continuous learning and professional development activities such as workshops, seminars, and online courses can provide essential tools for sharpening critical thinking skills.
Secondly, fostering a culture of open communication and collaborative problem-solving offers great benefits. These platforms facilitate the sharing of diverse perspectives, promoting deep analyses, and enriching the problem-solving process.
Lastly, reflective practice can also positively impact critical thinking abilities. Regular reflection on your practice, experiences, and learnings enables you to identify gaps in your thinking and areas of improvement. It encourages a deeper level of thinking that enriches the problem-solving process.
- Continuous learning and participation in professional development activities.
- Fostering a culture of open communication and collaborative problem-solving.
- Engaging in reflective practice regularly.
Examples of Critical Thinking Leading to Effective Problem Solving
The application of critical thinking skills often results in improved problem-solving outcomes in nursing management. Several instances illustrate this relationship.
For instance, consider a situation where a nursing unit has seen a significant increase in medication errors. The nursing manager applies critical thinking to evaluate the situation, identify potential causes, and devise solutions. Through an in-depth review of pharmaceutical administration procedures, team collaboration, discussion, and data evaluation, the nursing manager identifies the root cause - an overly complicated method of logging medication.
Armed with this information, they innovate a simpler, more effective system. By cutting down on needless complexity, the nursing unit sees a drastic decrease in medication errors. This example shows how the application of critical thinking streamlined a complex process, providing an effective solution to the problem at hand.
Another instance could be changing patient demographics, with more elderly patients requiring care. A nursing manager applies critical thinking to understand the unique needs of these patients and the potential challenges that might arise in catering to these needs. As a result, they develop tailored care plans and training programmes for the nursing staff to better care for elderly patients, resulting in improved patient satisfaction.
These examples highlight how critical thinking can lead to effective problem solving in nursing management, ultimately resulting in better service delivery and patient care. Therefore, enhancing critical thinking should be seen as a vital strategy for improving problem-solving proficiency in nursing management.
Problem Solving in Nursing Management - Key takeaways
- Problem Solving in Nursing Management: It is a thorough process involving the identification, analysis, and (de)cision-making to solve issues in nursing management. It also includes implementation and review of the effectiveness of the solutions.
- Decision Making Techniques: Different techniques such as Pros and Cons Analysis, Decision Matrix, and Cost-Benefit Analysis can enhance the decision-making process in problem-solving scenarios.
- Case Study Analysis: It involves the detailed examination of various scenarios to inform problem-solving strategies and practice.
- Approaches to Problem-Solving: Different approaches may apply in different nursing scenarios, such as the algorithm-based approach for well-defined scenarios and the intuition-driven approach for ambiguous situations.
- Strategic Problem-Solving Competencies: These are essential skills including critical thinking, innovative thinking, collaboration, adaptability, leadership, and decision-making, crucial in effective problem-solving.
- Leadership in Nursing: Leadership plays a key role in guiding, motivating, and supporting nursing staff. It influences the successful implementation of problem-solving strategies.
- Resource Utilisation: Efficient and effective use of available resources, such as nursing staff, equipment, and supplies, is vital in problem-solving in nursing management.
- Stages of Problem Solving in Nursing Practice: The stages include the identification, analysis, and resolution of problems, which are crucial in responding to challenges in the healthcare sector.
Flashcards in Problem Solving in Nursing Management 14
What is the significance of problem-solving in nursing management?
Problem-solving in nursing management is crucial in maintaining optimal patient care, operational efficiency, and fostering team collaboration by resolving intricate issues with decisive and effective solutions.
What are the key skills required for effective problem-solving in nursing management?
The key skills required are critical thinking, decisiveness, communication, and collaboration. Each skill is interconnected and helps in formulating impactful solutions.
What are the key steps involved in the problem-solving process in nursing management?
The key steps are identification, definition, analysis, development of solutions, decision making, implementation, and evaluation.
What does the neurological framework in nursing management involve?
This framework involves cognitive processes such as critical thinking, decision making, and problem-solving.
What is decision making in nursing management?
This involves selecting a course of action from different alternatives. It acts as a bridge, connecting problem analysis with implementing solutions and requires evaluation of information, predicaments, and possible outcomes.
What is problem solving in nursing management and how is it different from decision making?
Problem solving is a broader process involving the identification of an issue, systematic analysis to understand it, devising potential solutions, choosing the most suitable through decision making, implementing it, and finally reviewing the effectiveness of the implemented solution. Decision making, on the other hand, is a component nested within this process.
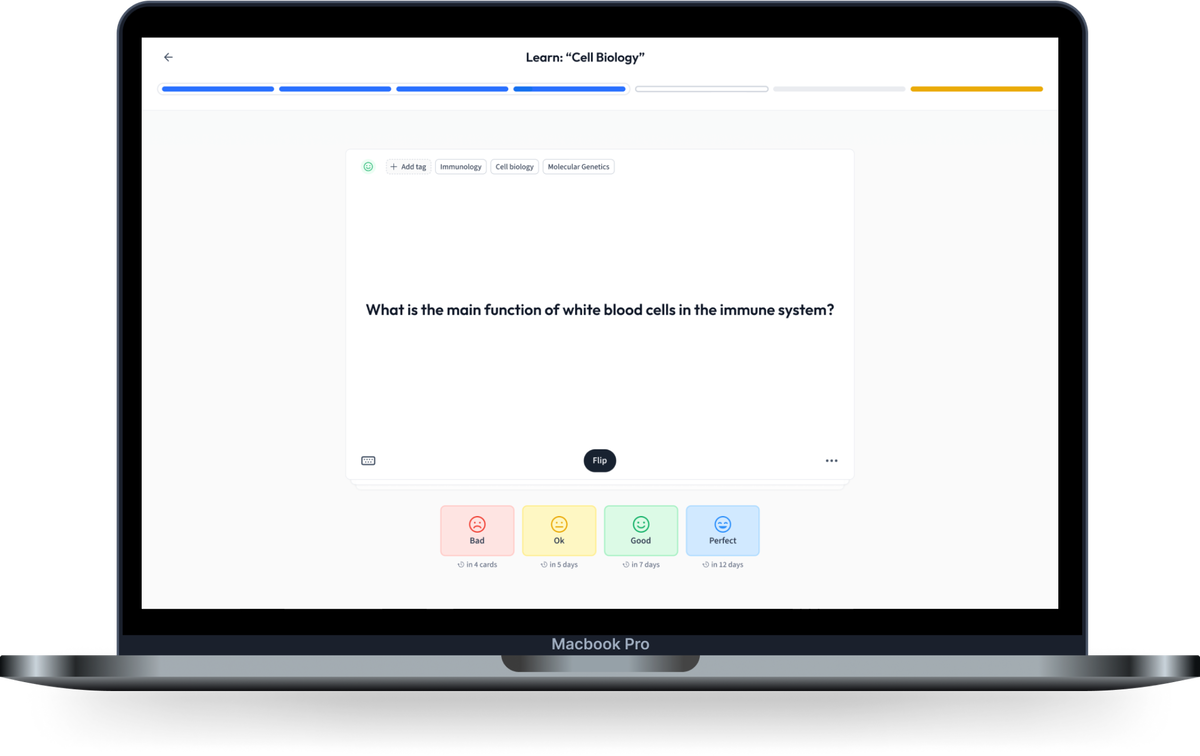
Learn with 14 Problem Solving in Nursing Management flashcards in the free StudySmarter app
We have 14,000 flashcards about Dynamic Landscapes.
Already have an account? Log in
Frequently Asked Questions about Problem Solving in Nursing Management
Test your knowledge with multiple choice flashcards.
Join the StudySmarter App and learn efficiently with millions of flashcards and more!
Keep learning, you are doing great.
Discover learning materials with the free StudySmarter app

About StudySmarter
StudySmarter is a globally recognized educational technology company, offering a holistic learning platform designed for students of all ages and educational levels. Our platform provides learning support for a wide range of subjects, including STEM, Social Sciences, and Languages and also helps students to successfully master various tests and exams worldwide, such as GCSE, A Level, SAT, ACT, Abitur, and more. We offer an extensive library of learning materials, including interactive flashcards, comprehensive textbook solutions, and detailed explanations. The cutting-edge technology and tools we provide help students create their own learning materials. StudySmarter’s content is not only expert-verified but also regularly updated to ensure accuracy and relevance.

StudySmarter Editorial Team
Team Problem Solving in Nursing Management Teachers
- 25 minutes reading time
- Checked by StudySmarter Editorial Team
Study anywhere. Anytime.Across all devices.
Create a free account to save this explanation..
Save explanations to your personalised space and access them anytime, anywhere!
By signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Sign up to highlight and take notes. It’s 100% free.
Join over 22 million students in learning with our StudySmarter App
The first learning app that truly has everything you need to ace your exams in one place
- Flashcards & Quizzes
- AI Study Assistant
- Study Planner
- Smart Note-Taking
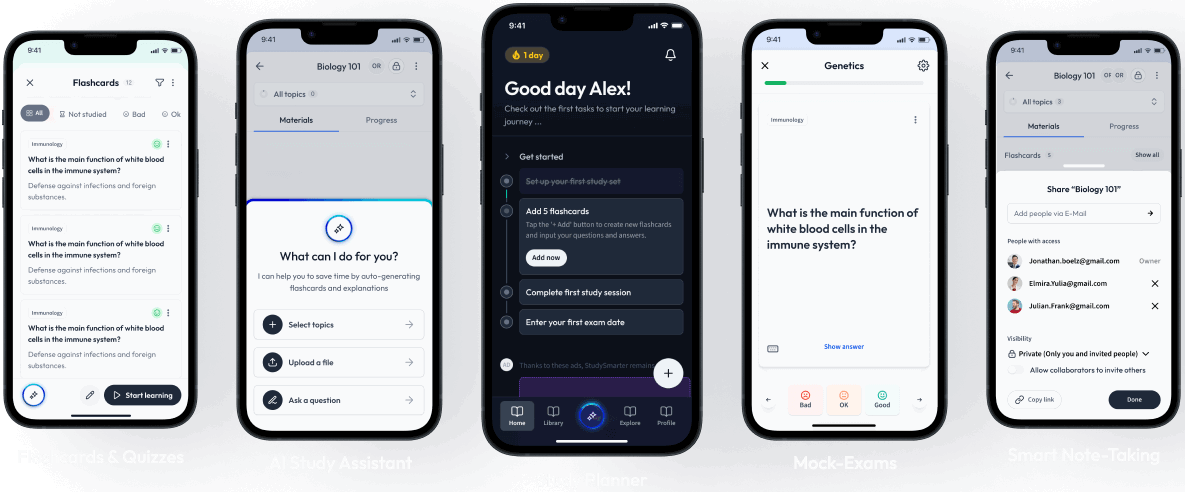

Two Examples of How I Used Critical Thinking to Care for my Patient (Real Life Nursing Stories) | NURSING.com

What are you struggling with in nursing school?
NURSING.com is the BEST place to learn nursing. With over 2,000+ clear, concise, and visual lessons, there is something for you!
Critical Thinking on the Nursing Floor
Critical thinking can seem like such an abstract term that you don’t practically use. However, this could not be farther from the truth. Critical thinking is frequently used in nursing. Let me give you a few examples from my career in which critical thinking helped me take better care of my patient.
The truth is, that as nurses we can’t escape critical thinking . . . I know you hate the word . . . but let me show you how it actually works!
Critical Thinking in Nursing: Example 1
I had a patient that was scheduled to go to get a pacemaker placed at 0900. The physician wanted the patient to get 2 units of blood before going downstairs for the procedure. I administered it per protocol. About 30 minutes after that second unit got started, I noticed his oxygen went from 95% down to 92% down to 90%. I put 2L of O2 on him and it came up to 91%. But it just sort of hung around the low 90s on oxygen.
I stopped. And thought. What the heck is going on?
I looked at his history. Congestive heart failure.
I looked at his intake and output. He was positive 1.5 liters.
I thought about how he’s got extra fluid in general, and because of his CHF, he can’t really pump out the fluid he already has, let alone this additional fluid. Maybe I should listen to his lungs..
His lungs were clear earlier. I heard crackles throughout both lungs.
OK, so he’s got extra fluid that he can’t get out of his body. What do I know that will get rid of extra fluid and make him pee? Maybe some Lasix?
I ran over my thought process with a coworker before calling the doc. They agreed. I called the doc and before I could suggest anything, he said “Give him 20 mg IV Lasix one time, and I’ll put the order in.” CLICK.
I gave the Lasix. He peed like a racehorse (and was NOT happy with me for making that happen!). And he was off of oxygen before he went down to get his pacemaker.
Badda Bing Bada Boom!
Critical Thinking in Nursing: Example 2
My patient just had her right leg amputated above her knee. She was on a Dilaudid PCA and still complaining of awful pain. She maxed it out every time, still saying she was in horrible pain. She told the doctor when he rounded that morning that the meds weren’t doing anything. He added some oral opioids as well and wrote an order that it was okay for me to give both the oral and PCA dosings, with the goal of weaning off PCA.
“How am I going to do that?” I thought. She kept requiring more and more meds and I’m supposed to someone wean her off?
I asked her to describe her pain. She said it felt like nerve pain. Deep burning and tingling. She said the pain meds would just knock her out and she’d sleep for a little while but wake up in even worse pain. She was at the end of her rope.
I thought about nerve pain. I thought about other patients that report similar pain. Diabetics with neuropathy would talk about similar pain… “What did they do for it? ” I thought. Then I remembered that many of my patients with diabetic neuropathy were taking gabapentin daily for pain.
“So if this works for their nerve pain, could it work for a patient who has had an amputation?” I thought.
I called the PA for the surgeon and asked them what they thought about trying something like gabapentin for her pain after I described my patient’s type of pain and thought process.
“That’s a really good idea, Kati. I’ll write for it and we’ll see if we can get her off the opioids sooner. ”
She wrote for it. I gave it. It takes a few days to really kick in and once it did, the patient’s pain and discomfort were significantly reduced. She said to get rid of those other pain meds because they “didn’t do a damn thing,” and to “just give her that nerve pain pill because it’s the only thing that works”.
And that we did!
She was able to work with therapy more because her pain was tolerable and was finally able to get rest.
What the HELL is Critical Thinking . . . and Why Should I Care?
What your nursing professor won’t tell you about critical thinking .
by Ashely Adkins RN BSN
When I started nursing school, I remember thinking, “how in the world am I going to remember all of this information, let alone be able to apply it and critically think?” You are not alone if you feel like your critical thinking skills need a little bit of polishing.
Let’s step back for a moment, and take a walk down memory lane. It was my first semester of nursing school and I was sitting in my Fundamentals of Nursing course. We were learning about vital signs, assessments, labs, etc. Feeling overwhelmed with all of this new information (when are you not overwhelmed in nursing school?), I let my mind wonder to a low place…
Am I really cut out for this? Can I really do this? How can I possibly retain all of this information? Do they really expect me to remember everything AND critically think at the same time?
One of my first-semester nursing professors said something to me that has stuck with me throughout my nursing years. It went a little something like this:
“Critical thinking does not develop overnight . It takes time. You don’t learn to talk overnight or walk overnight. You don’t learn to critically think overnight .”
My professor was absolutely right.
As my journey throughout nursing school, and eventually on to being a “real nurse” continued, my critical thinking skills began to BLOSSOM. With every class, lecture, clinical shift, lab, and simulation, my critical thinking skills grew.
You may ask…how?
Well, let me tell you…
- Questioning
These are the key ingredients to growing your critical thinking skills.
Time. Critical thinking takes time. As I mentioned before, you do not learn how to critically think overnight. It is important to set realistic expectations for yourself both in nursing school and in other aspects of your life.
Exposure. It is next to impossible to critically think if you have never been exposed to something. How would you ever learn to talk if no one ever talked to you? The same thing applies to nursing and critical thinking.
Over time, your exposure to new materials and situations will cause you to think and ask yourself, “why?”
This leads me to my next point. Questioning. Do not be afraid to ask yourself…
“Why is this happening?”
“Why do I take a blood pressure and heart rate before I give a beta-blocker?”
“Why is it important to listen to a patient’s lung sounds before and after they receive a blood transfusion?”
It is important to constantly question yourself. Let your mind process your questions, and discover answers.
Confidence. We always hear the phrase, “confidence is key!” And as cheesy as that phrase may be, it really holds true. So many times, we often times sell ourselves short.
YOU KNOW MORE THAN YOU THINK YOU KNOW.
In case you did not catch it the first time…
Be confident in your knowledge, because trust me, it is there. It may be hiding in one single neuron in the back of your brain, but it is there.
It is impossible to know everything. Even experienced nurses do not know everything.
And if they tell you that they do…they are wrong!
The key to critical thinking is not about knowing everything ; It is about how you respond when you do not know something .
How do you reason through a problem you do not know the answer to? Do you give up? Or do you persevere until you discover the answer?
If you are a nursing student preparing for the NCLEX, you know that the NCLEX loves critical thinking questions. NRSNG has some great tips and advice on critical thinking when it comes to taking the NCLEX .
There are so many pieces to the puzzle when it comes to nursing, and it is normal to feel overwhelmed. The beauty of nursing is when all of those puzzle pieces come together to form a beautiful picture.
That is critical thinking.
Critical thinking is something you’ll do every day as a nurse and honestly, you probably do it in your regular non-nurse life as well. It’s basically stopping, looking at a situation, identifying a solution, and trying it out. Critical thinking in nursing is just that but in a clinical setting.
We’ve written a MASSIVE lesson on Care Plans and Critical Thinking :
Mastering The COPD Nursing Care Plan in Just 10 Minutes!
Renal Failure Pt Care
4 "real world" examples of using clinical judgement to figure out what to do first as a nurse | nursing.com, 12 study tips for how to study for pharmacology in nursing school | nursing.com, similar blog posts.

Critical Thinking and Nursing Care Plans Go Together Like Chicken and Waffles | NURSING.com

Patients We Will Never Forget | NURSING.com
The Ultimate Guide to Creating an ICU Report Sheet (for new Critical Care Nurses and RN Students) | NURSING.com
Innovations in Teamwork for Health Care
Don’t leave teaming up to chance. Create better teamwork through science.
In this course, experts from Harvard Business School and the T.H. Chan School of Public Health teach learners to implement a strategy for organizational teamwork in health care.
What You'll Learn
Health care is a team effort. From the front desk administrators to the nurses, doctors, insurers, and even the patients and their families, there are many people involved in an individual’s care. To deliver quality care in today’s fast-paced environment, practitioners and caregivers must go beyond medical problem-solving and rely on effective collaboration and communication skills.
While other businesses may organize around a functional area or project, allowing team members to learn each other's working styles and strengths over time, health care workers often find themselves in ad hoc scenarios, coordinating with near-strangers on life and death situations. As a leader, how do you encourage trust and meet shared goals when teams are formed quickly? How do you strengthen flexibility and collaboration even as team membership and structures fluctuate across departments?
In Innovations in Teamwork for Health Care, leaders in the field of organizational behavior and teamwork, Amy Edmondson, Professor at Harvard Business School, and Michaela Kerrissey, Assistant Professor at the Harvard T.H. Chan School of Public Health, share their latest research and present their concept of "teaming" as it relates to the health care and life science industries.
In this course, you will explore the complexities of collaboration in dynamic cross-functional teams and its impact on quality of care. You will examine the theory of teaming – where individuals join together to lend their expertise – to appreciate what enables effective teamwork and why teamwork fails; articulate the importance of psychological safety and a joint problem-solving orientation; understand the particular needs of time-limited teams; and rethink the role of hierarchy and leadership in the context of teaming.
You’ll hear firsthand from experts with experience inside and outside the health care industry, from CEO and President of the Cleveland Clinic, Tomislav Mihaljevic, to Andres Sougarret, the engineer who led the miraculous rescue of 33 Chilean miners in 2011.
Ultimately, this course provides you with the tools needed to implement effective teaming strategies for patient-centered care and provides your organization with a framework to empower robust communication, improve efficiency, and elevate patient safety.
The course will be delivered via HBS Online’s course platform and immerse learners in real-world examples from experts at industry-leading organizations. By the end of the course, participants will be able to:
- Explore the science of teamwork, focusing on the psychological and sociological aspects of teaming, collaboration, and defining effective outcomes.
- Understand the complexity of building trust in ad hoc teams, including how to define purpose, build trust, and navigate interpersonal risks to reach common goals.
- Apply communication strategies that encourage psychological safety and create a safe space for all to contribute.
- Understand the value in adopting a model of joint problem-solving for patient care.
- Identify the distinct needs of time-limited project teams and how to incorporate effective and transparent feedback loops.
- Ensure accountability and identify leaders, breaking down hierarchy and encouraging the right person to step up at the right time.
- Implement a PDSA (Plan, Do, Study, and Act) framework for your organization.
Continuing Education Credits
In support of improving patient care, Harvard Medical School is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education.
The Harvard Medical School designates this enduring material for a maximum of 20 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. Harvard Medical School is accredited as a provider of nursing continuing professional development by the American Nurses Credentialing Center’s Commission on Accreditation.
This activity is approved for 20.00 contact hours. Contact hours are awarded commensurate with participation and completion of the online evaluation and attendance attestation. We suggest claiming your hours within 30 days of the activity date, after this time, the attendance attestation will still be required to claim your hours.
Groups of 10 or more receive Amy Edmondson's latest book!
A free, hard copy of right kind of wrong: the science of failing well for each participant. .
Your Instructors
Amy C. Edmondson is the Novartis Professor of Leadership and Management at Harvard Business School, a chair established to support the study of human interactions that lead to the creation of successful enterprises that contribute to the betterment of society. She has pioneered the concept of psychological safety for over 20 years and was recognized in 2021 as #1 on the Thinkers50 global ranking of management thinkers.
She is the author of Teaming: How Organizations Learn, Innovate, and Compete in the Knowledge Economy (2012), The Fearless Organization: Creating Psychological Safety in the Workplace for Learning, Innovation, and Growth (2018), and Right Kind of Wrong: The Science of Failing Well (2023).
Michaela Kerrissey is an Assistant Professor of Management at the Harvard T.H. Chan School of Public Health. She conducts research on how teams and organizations innovate, integrate, and perform, with a focus on health care. Dr. Kerrissey has authored over 30 publications on these topics and has won numerous best-paper awards, such as from the Academy of Management. She designed the Management Science for a New Era course at Harvard’s School of Public Health. In 2023, she was listed on Thinkers50 Radar, a global listing of top management thinkers.
Real World Case Studies
Affiliations are listed for identification purposes only.

Tomislav Mihaljevic, MD
Learn from the President and CEO of the Cleveland Clinic about how to implement joint problem solving in complex care organizations.
Maya Rupert
Hear from a top political strategist and campaign manager about how she leads within a teaming structure.
Trishan Panch, MD, MPH
Learn from Harvard faculty and founder of Wellframe about the importance of team learning.
Available Discounts and Benefits for Groups and Individuals
Experience Harvard Online by utilizing our wide variety of discount programs for individuals and groups.
Past participant discounts.
Learners who have enrolled in at least one qualifying Harvard Online program hosted on the HBS Online platform are eligible to receive a 30% discount on this course, regardless of completion or certificate status in the first purchased program. Past Participant Discounts are automatically applied to the Program Fee upon time of payment. Learn more here .
Learners who have earned a verified certificate for a HarvardX course hosted on the edX platform are eligible to receive a 30% discount on this course using a discount code. Discounts are not available after you've submitted payment, so if you think you are eligible for a discount on a registration, please check your email for a code or contact us .
Nonprofit, Government, Military, and Education Discounts
For this course we offer a 30% discount for learners who work in the nonprofit, government, military, or education fields.
Eligibility is determined by a prospective learner’s email address, ending in .org, .gov, .mil, or .edu. Interested learners can apply below for the discount and, if eligible, will receive a promo code to enter when completing payment information to enroll in a Harvard Online program. Click here to apply for these discounts.
Gather your team to experience Innovations in Teamwork for Health Care and other Harvard Online courses to enjoy the benefits of learning together:
- Single invoicing for groups of 10 or more
- Tiered discounts and pricing available with up to 50% off
- Growth reports on your team's progress
- Flexible course and partnership plans
Learn more and enroll your team !
Course Syllabus
Learning requirements: There are no prerequisites required to enroll in this course. In order to earn a Certificate of Completion from Harvard Online and Harvard Business School Online, participants must thoughtfully complete all 5 modules, including satisfactory completion of the associated assignments, by stated deadlines.
Download Full Syllabus
- Study the Mining Accident Rescue and Cleveland Clinic cases.
- Understand the concept of teaming and how it can be applied to the health care industry.
- Brainstorm how to organize with a team to rescue 33 trapped miners.
- Analyze the problems solved and new challenges created by organizational structures that were implemented to facilitate teamwork at the Cleveland Clinic.
- Outline and analyze an individualized teaming breakdown for your organization.
- Study the NASA and Google cases on psychological safety.
- Collaborate with team members and leadership to create a space of psychological safety.
- Identify the indicators of psychological safety in a group. Analyze data from Project Aristotle’s study of teams at Google.
- Consider how past experiences can affect current feelings of psychological safety.
- Study the Cleveland Clinic , Boehringer Ingelheim , and Cincinnati Children’s Hospital Medical Center cases.
- Implement a joint problem-solving orientation in which team members view problems as shared and solutions as requiring collaboration.
- Match different types of diversity in the workplace with the interpersonal boundaries that they imply.
- Articulate what you bring to a team and what you might need from others.
- Walk down the ladder of inference to get to the root of a problem.
- Study the Virginia Mason Medical Center and Institute for Healthcare Improvement cases.
- Cultivate an organization where team learning is valued and mobilized for improved performance.
- Identify different kinds of work on the process knowledge spectrum.
- Brainstorm how a nursing team could learn from an accidental morphine overdose.
- Study the cases of Julio Castro's Presidential Campaign and Wellframe .
- Practice leadership skills that include coaching, enabling, and ensuring that the right voices are present or represented within the team structure.
- Build a leadership workshop for your team using the concepts addressed in this course.
- Practice asking meaningful questions as a way to encourage input and express authentic humility.
- Learn the difference between confirmatory and exploratory responses.
Earn Your Certificate
Enroll today in this course.
Still Have Questions?
What are the learning requirements? How do I list my certificate on my resume? Learn the answers to these and more in our FAQs.
Related Courses
Health care economics.
Taught by Harvard Medical School faculty, this course provides insights into the interactions between industries in the US health care sector and teaches what economic forces are shaping health care.
Digital Health
Digital technologies and big data offer tremendous opportunities to improve health care.
Reducing Racial Disparities in Health Care
In partnership with the Disparities Solutions Center at MGH, this course will help you deliver high-quality health care to all through organizational change.

IMAGES
VIDEO
COMMENTS
They want to see your problem-solving style and get a sense of how you react and respond to the specific challenges nurses tend to face. A great way for your interviewer to assess your response is by asking you situational and behavioral questions. STAR: The #1 Strategy for Answering Scenario-Based Questions
Problem-solving occurs when nurses implement critical thinking measures to obtain information about a problem and suggest possible solutions. 6. Flexibility: ... The following are some examples of critical thinking in nursing with scenarios of poor critical thinking and excellent critical thinking responses. 1. Scenario: Patient/Caregiver ...
Problem-solving in nursing is the act of utilizing critical thinking and decision-making skills to identify, analyze, and address problems or challenges encountered by nurses in the healthcare setting. Problem-solving in nursing can be related to specific patient needs or may be related to staff issues. Either way, it is an important skill for ...
Sample Nurse Interview Questions: Time Management. Nurses are masters at multitasking - for example, managing multiple patients and administering medication on time while maintaining detailed notes. Tell stories about your punctuality, ability to meet deadlines, and how you remain organized through it all. 1.
• Discuss 7 steps to problem-solving. Introduction As medicine becomes more and more complex and nursing responsibilities increase, critical thinking—the ability to question and make rational decisions—becomes even more important. Too often, healthcare providers simply follow routines and accept the word of
Nurses can implement the original nursing process to guide patient care for problem solving in nursing. These steps include: Assessment. Use critical thinking skills to brainstorm and gather information. Diagnosis. Identify the problem and any triggers or obstacles. Planning. Collaborate to formulate the desired outcome based on proven methods ...
Learning to provide safe and quality health care requires technical expertise, the ability to think critically, experience, and clinical judgment. The high-performance expectation of nurses is dependent upon the nurses' continual learning, professional accountability, independent and interdependent decisionmaking, and creative problem-solving abilities.
Problem-solving skills. Practicing your problem-solving skills can improve your critical-thinking skills. Analyze the problem, consider alternate solutions, and implement the most appropriate one. Besides assessing patient conditions, you can apply these skills to other challenges, such as staffing issues. How to Develop and Apply Critical ...
8. Clinical Simulations: Learning through Virtual Scenarios. Clinical simulations provide nurses with a risk-free environment to practice decision-making and problem-solving skills. These virtual scenarios mimic real-life patient situations and allow nurses to test different approaches, assess outcomes, and reflect on their choices.
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood ...
01. INTRODUCTION. Each answer should start by establishing the problem or event you're going to talk about. If you're asked to describe a stressful event in your life and how you handled it, you will obviously start by introducing the problem. Example: "About two years ago my mother and father were both diagnosed with cancer.
Decision-making is a fundamental concept of nursing practice that conforms to a systematic trajectory involving the assessment, interpretation, evaluation and management of patient-specific situations (Dougherty et al, 2015).Shared decision-making is vital to consider in terms of patient autonomy and professional duty of care as set out in the Nursing and Midwifery Council (NMC) (2018)Code ...
The term 'critical thinking' is often used interchangeably with problem-solving and clinical decision-making in nursing literature. Problem-solving focuses on identification and resolution, whereas critical thinking goes beyond this and incorporates asking questions and critiquing solutions. The concept of clinical decision-making focuses ...
Nurse leaders perceive their role as a problem-solver, which is a necessary step in advocacy. 27 Problem-solving is a process that contains the elements of decision-making and critical thinking. 28. The theory that emerged from the core categories explicitly focused on the central phenomenon of LHV in the nursing work environment.
The nursing diagnosis in Scenario C will be related to the patient's response to heart failure. Additional Definitions Used in NANDA-I Nursing Diagnoses. The following definitions of patient, age, and time are used in association with NANDA-I nursing diagnoses: ... A lifelong problem-solving approach that integrates the best evidence from ...
17. Situational Questions. 18. Teamwork Questions. 19. Tough Questions. Situational questions are asked so the interviewer can gain insight into your thought process, how you problem-solve, and how you communicate in the workplace. Situational nursing questions can include inquiries about drug dosages, procedures, or specific signs and symptoms ...
A problem-based learning scenario and Kirkpatrick's model for evaluation were used to address incivility and the "reality shock" between what students learn about the practice of nursing and the interactions they may experience in the workplace. ... Solving real nursing problems through problem-based learning.
Practical experience. Practical, hands-on experience is crucial to excelling in any nursing role. Developing critical-thinking skills starts at the beginning of your career, not just in your first position but also the experience you obtain while studying. Anyone will tell you that gaining essential and varied work experience will help you ...
Using divergent thinking - where you consider a problem in different ways to expand your view - may also help. A final alternative is the stepladder technique, which is time-consuming but effective if the issue is stirring up strong feelings. This requires the people involved in the problem to be organised into groups.
Step 2: Analyze the Problem. Break down the problem to get an understanding of the problem. Determine how the problem developed. Determine the impact of the problem. Step 3: Develop Solutions. Brainstorm and list all possible solutions that focus on resolving the identified problem. Do not eliminate any possible solutions at this stage.
Dive deep into the multifaceted world of nursing management with a special focus on problem-solving. This comprehensive guide presents a detailed look at the process, importance, and challenges of problem-solving in nursing management. By highlighting essential skills, neurologically based frameworks, and the relationship with decision-making, it offers both theoretical understanding and ...
Critical thinking can seem like such an abstract term that you don't practically use.However, this could not be farther from the truth. Critical thinking is frequently used in nursing. Let me give you a few examples from my career in which critical thinking helped me take better care of my patient.
Understand the value in adopting a model of joint problem-solving for patient care. Identify the distinct needs of time-limited project teams and how to incorporate effective and transparent feedback loops. Ensure accountability and identify leaders, breaking down hierarchy and encouraging the right person to step up at the right time.
Image Register to Livestream FHFA's Generative Artificial Intelligence (AI) in Housing Finance TechSprint Register here to livestream Opening Day and Demo Day of FHFA's Generative AI in Housing Finance TechSprint. Opening Day, beginning at 10:30 am EST on Monday, July 22, will feature remarks from FHFA leadership and keynote speakers. Demo Day, beginning at 9:00 am EST on Thursday, July 25 ...