0078021332
2013 Chronic, non-communicable diseases such as cardiovascular disease, cancer, stroke, and type 2 diabetes are among the leading causes of death globally, resulting in untold human suffering from premature morbidity and mortality. Left unchecked, the economic burden of chronic disease has the potential to cripple national economies. Because unhealthful dietary patterns (along with tobacco smoking and physical inactivity) are major risk factors for chronic disease, assessing diet and nutritional status and the results of interventions to improve nutritional status is fundamental to our success at reducing chronic disease risk, promoting health, and managing heath care costs. , Sixth Edition explains the tools and techniques that nutrition practitioners and other health care providers can use to assess diet and nutritional status in instances of acute illness as well as chronic disease prevention and treatment. Key features of this edition include: , and MyPlate.
| |
| | | Instructors: To experience this product firsthand, contact your . | | |
Copyright
Any use is subject to the and | |
 Nutrition Assessment Forms: What to Include?- December 7, 2023
- Business Setup
 Written by Olivia Farrow, RD, MHScReviewed by Maria Dellanina, RDN In the realm of nutrition care, a well-structured nutrition assessment is key to understanding and addressing a client’s unique needs. In this blog post, we’ll delve into the intricacies of nutrition assessment forms; what nutrition assessment entails and what to include in effective intake forms and chart notes to simplify the process. Understanding Nutrition AssessmentNutrition assessment is the first part of the nutrition care process; the “A” in ADIME. At its core, nutrition assessment is a systematic methodology, encompassing the collection, classification, and synthesis of pertinent data ( 1 ). This process is not a one-time event, but rather an ongoing, dynamic journey that involves initial data collection, continual reassessment, and analysis of a client’s status in relation to accepted standards, recommendations, and goals ( 1 ). Key Components of Nutrition Assessment:The nutrition care process includes 9 categories of nutrition assessment data ( 1 ). Each of these categories should be included on nutrition assessment forms, however the examples of data collected will depend on the individual client and practice setting ( 1 ): - Food/Nutrition-Related History: Delving into food and nutrient intake, administration, medication use, beliefs, attitudes, behavior, and more.
- Anthropometric Measurements: Considering body height, weight, frame, changes, and growth patterns.
- Biochemical Data, Medical Tests, and Procedures: Incorporating lab data, medical tests, and procedures.
- Physical Exam Findings: Evaluating findings from physical exams, interviews, or health records.
- Client History: Exploring personal, family, and social history.
- Assessment, Monitoring, and Evaluation Tools: Utilizing tools for health or disease status assessment.
- Etiology Category: Categorizing the type of nutrition diagnosis etiology.
- Comparative Standards: Establishing benchmarks for data comparison.
- Progress Evaluation: Assessing progress toward nutrition-related goals and resolution of nutrition diagnoses.
Where to Find Nutrition Assessment Data?The nutrition assessment data in each of the 9 categories, can be sourced before interacting with the client, through intake forms, health records, or information from referring or team healthcare providers. Data obtained before interacting with the client should always be confirmed during direct client interaction (or interactions with their substitute decision maker). During client interactions, additional data can be obtained directly from the client or based on observations during the session. Your Nutrition Assessment FormsNutrition assessment forms can be broken down into different components, which will likely include: - A data collection form; such as an initial intake form.
- A dietary intake form; a space for the client or practitioner to fill in food intake data.
- A chart note; the formal documentation space where the complete nutrition assessment will be outlined.
Having detailed intake form and chart note templates can help to support optimal nutrition assessment data collection. DSC has collaborated with Practice Better to provide you with a FREE form template bundle including: - Adult intake form
- Pediatric intake form
- Initial chart note template
- Follow-up chart note template
- 24-hour recall template
- 3-day food record template
 Disclaimer: The form bundle was sponsored by Practice Better. Crafting Your Nutrition Assessment Forms The first part of your nutrition assessment forms is a space for gathering nutrition assessment data. This could be in the form of an intake form that the client fills out, a data collection form that you complete while interacting with the client and/or from the client’s data in their medical chart. To make your nutrition assessment simpler and more comprehensive, an intake or data collection nutrition assessment form might include: - Personal Information: contact details, reason for consultation (referral or request), relevant demographic and lifestyle information.
- Medical History: Conditions, surgeries, medications, allergies, supplement use, cognitive function data.
- Nutrition-focused physical findings: Physical symptoms related to nutrition such as appetite, swallowing, skin integrity, gastrointestinal symptoms, subjective global assessment.
- Biochemical Data : Including pertinent lab results and medical tests.
- Dietary Habits: Detailed insights into food preferences, meal patterns, and special dietary requirements. This might include a 24-hour recall, 3-day food record, or food frequency questions.
- Lifestyle Factors: Understanding physical activity (type and quantity of movement, sedentary activities, occupational related activity, ability to perform physical movements), sleep, and stress levels.
- Anthropometric Measurements: Height, weight (and source of data), weight history, how often weight is obtained, and relevant indices.
- S ocial and Cultural Factors: Factors affecting access to food, behaviors around food, social network, culturally related requirements around food or nutrition.
- Nutrition Knowledge and Attitudes: Level or areas of nutrition knowledge and food/health literacy, attitudes, beliefs, and relationship with food, readiness for change.
- Goals and Expectations: Exploring the client’s health and nutrition goals.
Your assessment might also include a validated screening tool such as a malnutrition screening tool, either as part of your nutrition assessment forms or separately.  Utilizing Your Nutrition Assessment DataAfter gathering all of the data you need for your nutrition assessment you will need to apply your critical thinking skills to interpret the data and conduct your assessment. Information gathering will also include meeting the client to understand and confirm the details of the pre-session data. Most of this part of your nutrition assessment will be housed in the assessment portion of your nutrition chart notes. A detailed chart note template can help you to ensure you don’t miss any important nutrition assessment details. An important part of your nutrition assessment is comparing the client’s data to comparative standards. These could be reference standards such as the dietary reference intakes (DRIs), recommendations (such as a practice guideline), or goals (i.e. the client has a specific habit or behavior they would like to modify). Once this step has been completed, you can put on your nutrition assessment hat and outline the main nutrition problem. This may require prioritization of the most severe problem if there are more than one. This nutrition problem will be directly used in your nutrition diagnosis; the “P” in PES Statement. For more information on PES Statements check out the blog article: How To Write a PES Statement (With Sample PES Statements!) and download our Free PES statement cheat sheet Key Takeaways- Nutrition assessment is a dynamic, systematic process and the first step in the nutrition care process.
- The nutrition care process includes nine categories, guiding the collection of important data.
- Effective nutrition assessment forms consist of a data collection form, dietary intake data form, and a formal chart note.
- Compare client data to standards, recommendations, or goals to identify and prioritize nutrition problems for effective intervention.
References:1. Academy of Nutrition and Dietetics. Nutrition Terminology Reference Manual (eNCPT): Dietetics Language for Nutrition Care. “NCP Step 1: Nutrition Assessment”. (2023 Edition) https://www.ncpro.org/pubs/2023-encpt-en/category-1 Related Articles © 2024 Dietitian Success Center Terms & Conditions Privacy Policy Learn more about the membershipDietitian Success Center is your one-stop-shop to access affordable, evidence based nutrition courses & resources, plus business building tools without the price tag of a high-ticket business coach. Student or Intern? Learn about our student rate . Already a member? - What is Nutrition Assessment? [Methods & Free Templates]
 What is Nutritional Assessment? The British Dietetic Association (BDA) defines nutritional assessment as the systematic process of collecting and interpreting information in order to make decisions about the nature and cause of nutrition-related health issues that affect an individual. It can be done by a healthcare professional or self-assessment using online tools. This assessment involves measuring body weight, height, blood pressure, heart rate, waist circumference, muscle mass, bone density, and other factors that may affect how much food you need to consume. Based on the data gathered, one can make an informed decision on what a person needs to eat in order to achieve and maintain health. The goal of nutrition assessment is to determine if your diet meets your nutrient requirements, which are based on your age, gender, activity level, current medical conditions, medications, and lifestyle choices. If your diet falls below these requirements, you can make any required changes to improve your eating habits. Try this out: Dietary Assessment Questionnaire Template Importance of Nutritional AssessmentYou are what you eat. Committing to nutritional assessment helps you know what you should and should not be eating if you want to live a healthy life. Let’s look at some other reasons why you should prioritize nutritional assessment. - Nutritional assessment helps people understand their own dietary intake and how it compares with the recommended daily allowances for nutrients.
- Regular nutritional assessment allows you to identify any potential risks associated with poor nutrition.
- It helps people make informed decisions about changes to their diets.
- A nutritional assessment provides information about whether or not there are specific foods that you shouldn’t eat.
- It helps you learn how to plan meals and snacks ahead so you don’t have to rely on fast food or convenience options.
- Regular nutritional assessment is the only way to ensure you’re getting enough nutrients from your meals and in the right quantities.
Explore: Nutritional Assessment Questionnaire Template How Often Should Nutritional Assessment Happen? A nutrition assessment should be performed at least once every year, depending on the individual’s health and lifestyle. For example, if you’re trying to lose weight , you may want to do an assessment more frequently than someone who’s maintaining their normal weight. Objectives of Nutritional AssessmentThe objectives of a nutritional assessment depend on the context of the program and what you want to achieve. In the case of a one-on-one program with an individual, the common goal should be improving the health habits and overall lifestyle of the patient. Nutritional assessment should also identify and address any cases of possible malnutrition. Other common objectives are: - Nutritional assessment evaluates a person’s overall health and nutritional status.
- It identifies possible nutrient deficiencies in an individual
- Nutritional assessment allows the experts to evaluate the effectiveness of prescribed treatments.
- It’s an effective way to monitor progress toward goals set during treatment.
- It helps you to prevent malnutrition.
- It provides an opportunity for the experts to educate their patients about proper nutrition.
- Nutritional assessment promotes healthy lifestyles.
- It encourages compliance with recommendations for treatment.
Use for Free: Macros Calories Diet Plan Template Types of Nutritional Assessment1. anthropometric nutritional assessment . Anthropometric measurements are noninvasive quantitative measurements of the body that provide valuable assessments of the nutritional status of children and adults. Typically, it involves the measurement of the size, weight, and proportions of the body. Anthropometric measurements are commonly used in the pediatric population to evaluate the general health status, nutritional adequacy, and the growth and developmental pattern of the child. An important part of this type of nutritional assessment is weighing the individual and calculating their body-mass index to know if they fall within the optimal range. Common anthropometric measurements include: - Body Mass Index
- Waist Circumference
- Skinfold thickness
- Bone Mineral Density
- Blood Pressure
- Body Fat Percentage
- Other measures of adiposity
- Muscle mass
- Lean Body Mass
- Fat-Free Mass
- Total Body Water
- Visceral fat
- Fasting Blood Glucose
- Lipid profile
Use for Free: Weight Loss Tracking Form Template Advantages of Anthropometric Assessment - It uses simple, safe, and non-invasive procedures.
- Anthropometric assessment techniques can be applied to a large sample size
- It is objective with high sensitivity and specificity.
- It can be done by healthcare providers without specialized training.
Disadvantages of Anthropometric Assessment - An anthropometric assessment covers limited nutritional diagnosis.
- Anthropometric measurements cannot identify protein and micronutrient deficiencies or detect small disturbances in nutritional status.
2. Biochemical AssessmentBiochemical assessment involves checking the level of nutrients in a person’s blood, urine, or stool, usually through a lab test. These lab tests can help a trained medical practitioner discover any medical problems affecting your nutritional status or appetite. For example, a lab scientist might take your blood sample to measure the level of glucose in your body. During a full biochemical assessment, the physician will screen the following biochemical parameters: albumin, prealbumin, CRP, transferrin, hemoglobin, urea and creatine, lymphocytes, and point deficiencies. Advantages of Biochemical Assessment - They pick up the earliest indication of malnutrition or any nutritional deficiencies in the body.
- Biochemical assessments also confirm the clinical diagnosis of nutritional status and/ or risk for a disease.
Disadvantages of Biochemical Assessment - It is time-consuming.
- The health practitioner needs to run multiple biological tests for a proper diagnosis.
Use For Free: Caloric Calculator For Fat Loss Form Template 3. Clinical Nutritional AssessmentClinical assessment is the simplest and most practical method of ascertaining the nutritional well-being of a patient. In this case, the physician examines specific areas of the patient’s body to discover any signs of deficiencies. A clinical nutritional assessment also involves asking the patient whether they have any symptoms that might suggest nutrient deficiency from the patient. Advantages of Clinical Assessment - It helps the health practitioner dictate changes in the body’s metabolism.
Disadvantages of Clinical Assessment - It is expensive.
- It only provides limited data on food composition.
4. Dietary Assessment Dietary assessment is the process of collecting information about what a person eats and drinks over a period of time. In other words, it is a record of the foods one eats in an attempt to calculate their potential nutrient intake. During a dietary assessment , the health practitioner analyzes the energy, nutrients, and other dietary constituents using food composition tables. The goal of dietary assessment is to identify appropriate and actionable areas of change in the patient’s diet and lifestyle and to improve the overall wellbeing of the patient. For a detailed analysis, the health practitioner can deploy one or more of these methods: - Diet Record
- 24-hour recall
- Food Frequency Questionnaire
Advantages of Dietary Assessment - It provides contextual information about a person’s nutritional intake.
- Results from the dietary assessment are largely accurate due to more detailed descriptions of foods and portion sizes.
Disadvantages of Dietary Assessment - It relies on accurate recall of dietary intake over a long period of time.
- It is prone to misreporting, especially when the health practitioner adopts food frequency questionnaires for data gathering.
Nutritional Assessment Tools Let’s look at some tools that health practitioners use to determine an individual’s nutritional needs. - Food Frequency Questionnaire
A food frequency questionnaire is a tool that helps you record how often you eat certain foods on a regular basis. It also asks questions about your eating habits. This information can then be compared to national guidelines or standards. A food frequency questionnaire will help you keep track of what you eat regularly. You can fill it out at home or take it to your doctor’s office. The answers provided will help your doctor make the right decisions about your nutritional health. When filling out a food questionnaire, write down everything you ate during the past 24 hours. Include all beverages, including water, milk, juice, soda, tea, coffee, alcohol, and any other drinks. Also, note if you skipped meals. If you’re not sure whether something was eaten, just put an “X” next to the item. A calorie calculator allows you to fill in the number of calories you consume in a day. Then, based on your weight, age, gender, height, and activity level, it determines the number of calories you need each day for a healthy life. A calorie calculator is only as good as the measurements you input. For instance, some people might forget to include snacks, such as cookies, crackers, chips, etc., when they count calories. And they might underestimate the calories they burn while exercising. These inaccurate measurements affect the quality of information you get from the calculator in the end. To use a calorie calculator, follow these steps: 1. Enter your current weight. 2. Choose from five different activities levels. The higher the level, the greater the intensity of exercise. 3. Select the number of days you’d like to calculate your daily calorie needs. 4. Click Calculate. 5. Review the results and adjust them as needed. 6. Print out your results. A food pyramid shows you how many servings of grains, vegetables, fruits, dairy products, meat, and oils you should eat every day. Each section represents a specific type of food. For example, the top part of the pyramid shows you how much whole grain bread, pasta, rice, cereal, oatmeal, and potatoes you should eat. The bottom part shows you how much fruit, vegetable, fish, meats, and eggs you should eat. Formplus is a data collection tool that allows you to create surveys and questionnaires for nutritional assessment. It has several features that help you collect data from respondents seamlessly and conveniently. Let’s look at a few reasons why you should use Formplus for nutritional assessment. 1. Create Mobile-Friendly Forms Formplus allows you to create mobile-responsive nutritional assessment forms that can be filled out on any device including smartphones, laptops, and notepads. Formplus forms offer an optimized user experience and fit into any devices they are viewed on. 2. Easy-to-use Drag and Drop Form Builder With Formplus, it is really easy for you to create your online interview form template in minutes in the drag-and-drop form builder; without any technical knowledge. All you need to do is click on your preferred form fields or drag and drop them into the form builder to add them to your nutritional assessment form. 3. Analytics and Reports The form analytics feature makes it easier for you to process form responses collected through your nutritional assessment form. You can view insights on form responses in the analytics dashboard including the total number of submissions, average form response time, and the devices used to fill out your form. 4. Multiple Form Fields Options Formplus has over 30 dynamic form fields that allow you to collect different information from patients; ranging from health information to file uploads. This means that you can now gather all the information you need to make an objective nutritional assessment in little or no time. Conclusion Nutritional assessment is important in maintaining fitness and general wellbeing. This is why it should be prioritized using all the tools and learnings that the 21st century offers  Connect to Formplus, Get Started Now - It's Free! - biochemical assessment
- calorie calculator
- dietary assessment
- dietary requirements
- food frequency questionnaire
- nutrition assessment
- busayo.longe
 You may also like: Training Survey: Types, Template + [Question Example]Conducting a training survey, before or after a training session, can help you to gather useful information from training participants....  Diet Planning For Weight Loss: Types, Tips & Free TemplatesIn this article, we would be exploring different types of diet planning along with templates you can use to quickly get started. Job Evaluation: Definition, Methods + [Form Template]Everything you need to know about job evaluation. Importance, types, methods and question examples 33 Online Shopping Questionnaire + [Template Examples]Learn how to study users’ behaviors, experiences, and preferences as they shop items from your e-commerce store with this article Formplus - For Seamless Data CollectionCollect data the right way with a versatile data collection tool. try formplus and transform your work productivity today..  Principles of Nutritional Assessment:3 rd Edition, April 2024 - Chapter 25b. Combs G.F. Jr. Selenium
Nutritional Assessment: Introduction1.0 new developments in nutritional assessment. “the use of emerging information and communications technology, especially the internet, to improve or enable health and health care” “those designed for delivery through mobile phones” ( Olson, 2016 ). 1.1 Nutritional assessment systems1.1.1 nutrition surveys, 1.1.2 nutrition surveillance. - Give timely warning of the need for intervention to prevent critical deteriorations in food consumption.
- communicated effectively.
1.1.3 Nutrition screening1.1.4 nutrition interventions. - Pathway 3: Increased knowledge and adoption of optimal nutrition practices, including intake of micronutrient-rich foods (knowledge–adoption of optimal health- and nutrition-related practices pathway) and improve delivery, utilization, and potential for impact of a Homestead Food Production Program in Cambodia.
 1.1.5 assessment systems in a clinical setting Table 1.1. Examples of personal goals in relation to personal nutrition. Data from van Ommen et al. ( ). | Goal | Definition |
|---|
Weight
management | Maintaining (or attaining) an ideal body weight
and/or body shaping that ties into heart, muscle,
brain and metabolic health | | Metabolic health | Keeping metabolism healthy today and tomorrow | | Cholesterol | Reducing and optimizing the balance between
high-density lipoprotein and low-density lipoprotein
cholesterol in individuals in whom this is disturbed | | Blood pressure | Reducing blood pressure in individuals who have
elevated blood pressure | | Heart health | Keeping the heart healthy today and tomorrow. | | Muscle | Having muscle mass and muscle functional abilities.
This is the physiological basis or underpinning of the
consumer goal of “strength” | | Endurance | Sustaining energy to meet the challenges of the
day (e.g., energy to do that report at work, energy
to play soccer with your children after work) | | Strength | Feeling strong within yourself,
avoiding muscle fatigue | | Memory | Maintaining and attaining an optimal short-term
and/or working memory | | Attention | Maintaining and attaining optimal focused and
sustained attention (i.e., being “in the moment” and
able to utilize information from that “moment”) | 1.1.6 Approaches to evaluate the evidence from nutritional assessment studies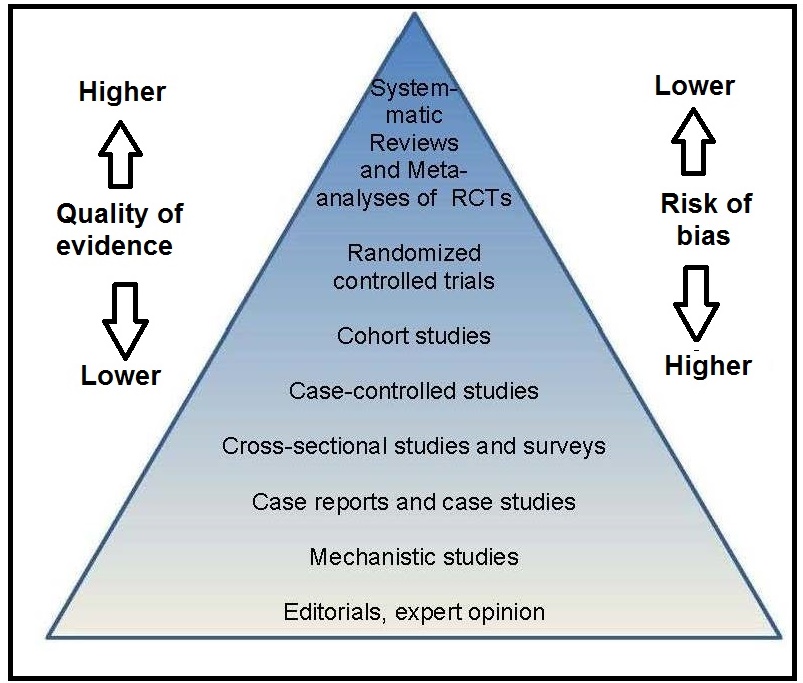 Table 1.2 Applying systemmatic reviews to nutrition questions: approaches to the challenges. Data from Brannon ( ). | Challenge | Approach |
|---|
| Baseline exposure | Unlike drug exposure, most persons have
some level of dietary exposure to the
nutrient or dietary substance of interest,
either from food or supplements, or
by endogenous synthesis in the case of
vitamin D, information on background
intakes and the methodologies used to assess
them should be captured in the
SR so that any related uncertainties can be
factored into data interpretation. | | Nutrient status | The nutrient status of an individual
or population can affect the response
to nutrient supplementation. | Chemical form
of the nutrient
or dietary substance | If nutrients occur in multiple forms, the forms
may differ in their biological activity.
Assuring bioequivalence or making
use of conversion factors can be
critical for appropriate data interpretation. | Factors that influence
bioavailability | Depending upon the nutrient or dietary
substance, influences such as
nutrient-nutrient interactions, drug
or food interactions, adiposity, or
physiological state such as pregnancy
may affect the utilization of the nutrient.
Capturing such information allows
these influences to be factored into
conclusions about the data. | Multiple and
interrelated biological
functions of a
nutrient or
dietary substance | Biological functions need to be understood
in order to ensure focus and to define
clearly the nutrient- or dietary
substance—specific scope of the review. | Nature of nutrient
or dietary substance
intervention | Food-based interventions require detailed
documentation of the approaches
taken to assess nutrient or dietary
substance intake. | Uncertainties in
assessing dose-
response
relationships | Specific documentation of measurement
and assay procedures is required to
account for differences in health outcomes. | 1.2 Nutritional assessment methods1.2.1 dietary methods. - An Overview of the Main Pre-Survey Tasks Required for Large-Scale Quantitative 24-Hour Recall Dietary Surveys in LMICs ( Vossenaar et al., 2020 )
1.2.2 Laboratory Methods“a biological characteristic that can be objectively measured and evaluated as an indicator of normal biological or pathogenic processes, and/or as an indicator of responses to nutrition interventions”. - Traditional dietary assessment methods
- Dietary biomarkers: indirect measures of nutrient exposure
- Biomarkers of “status”: body fluids (serum, erythrocytes, leucocytes, urine, breast milk); tissues (hair, nails)
- Functional biochemical: enzyme stimulation assays; abnormal metabolites; DNA damage. These biomarkers serve as early biomarkers of subclinical deficiencies.
- Functional physiological/behavioral: more directly related to health status or disease such as vision, growth, immune function, taste acuity, cognition, depression. These biomarkers impact on clinical and health outcomes.
1.2.3 Anthropometric methods1.2.4 clinical methods, 1.2.5 ecological factors.  1.3 Nutritional assessment indices and indicators Table 1.3. Examples of dietary, anthropometric, laboratory, and clinical indicators and their application. EAR, estimated average requirement; IDD, iodine deficiency disorders. | Nutritional indicator | Application |
|---|
| | | Prevalence of the population with zinc intakes
below the estimated average requirement (EAR) | Risk of zinc deficiency
in a population | Proportion of children 6–23mos of age who
receive foods from 4 or more food groups | Prevalence of minimum
dietary diversity | | | | Proportion of children age 6–60mos in the population
with mid-upper arm circumference < 115mm | Risk of severe acute
malnutrition in the population | Percentage of children < 5y with
length- or height-for-age less than −2.0 SD below
the age-specific median of the reference population | Risk of zinc deficiency
in the population | | | | Percentage of population with serum Zn concentrations
below the age/sex/time of day-specific lower cutoff | Risk of zinc deficiency
in the population | Percentage of children age 6–71mos in the
population with a serum retinol < 0.70µmol/L | Risk of vitamin A
deficiency in the population | Median urinary iodine <20µg/L based on > 300
casual urine samples | Risk of severe IDD
in the population | Proportion of children (of defined age and sex) with
two or more abnormal iron indices (serum ferritin,
erythrocyte protoporphyrin, transferrin receptor)
plus an abnormal hemoglobin | Risk of iron deficiency
anemia in the population | | | | | Prevalence of goiter in school-age children ≥ 30% | Severe risk of IDD among the
children in the population | | Prevalence of maternal night blindness ≥ 5% | Vitamin A deficiency is a severe
public health problem | 1.4 The design of nutritional assessment systems1.4.1 study objectives and ethical issues. - Determining the overall nutritional status of a population or subpopulation
- Identifying areas, populations, or subpopulations at risk of chronic malnutrition
- Characterizing the extent and nature of the malnutrition within the population or subpopulation
- Identifying the possible causes of malnutrition within the population or subpopulation
- Designing appropriate intervention programs for high-risk populations or subpopulations
- Monitoring the progress of changing nutritional, health, or socioeconomic influences, including intervention programs
- Evaluating the efficacy and effectiveness of intervention programs
- Tracking progress toward the attainment of long-range goals.
- Confidentiality is adequately protected.
- Describe the procedures that provide answers to any questions and further information about the study.
1.4.2 Choosing the study participants and the sampling protocol- Quota sampling involves dividing the target population into a number of different categories based on age, ownership of land, or occupations etc, and taking a certain number of consenting individuals from each category into the final sample.
- Selecting participants who are accessible by road introduces a “tarmac” bias. Areas accessible by road are likely to be systematically different from those that are more difficult to reach.
- random sampling requires defining a number of levels of sampling, from each of which is drawn a random sample.
1.4.3 Calculating sample size1.4.4 collecting the data, 1.4.5 additional considerations, 1.5 important characteristics of assessment measures, 1.5.1 validity.  1.5.2 Reproducibility or precision- Coefficient of Reliability
Table 1.4 Within-person and analytical variance components for some common biochemical measures. Abstracted from Gallagher et al. ( ). | Coefficient of variation (%) |
|---|
| Measurement | Within-person | Analytical |
|---|
| Serum retinol | | | | Daily | 11.3 | 2.3 | | Weekly | 22.9 | 2.9 | | Monthly | 25.7 | 2.8 | | Serum ascorbic acid | | | | Daily | 15.4 | 0.0 | | Weekly | 29.1 | 1.9 | | Monthly | 25.8 | 5.4 | | Serum albumin | | | | Daily | 6.5 | 3.7 | | Weekly | 11.0 | 1.9 | | Monthly | 6.9 | 8.0 | - Reducing the effect of random errors from any source by repeating all the measurements, when feasible, or at least on a random subsample.
1.5.3 Accuracy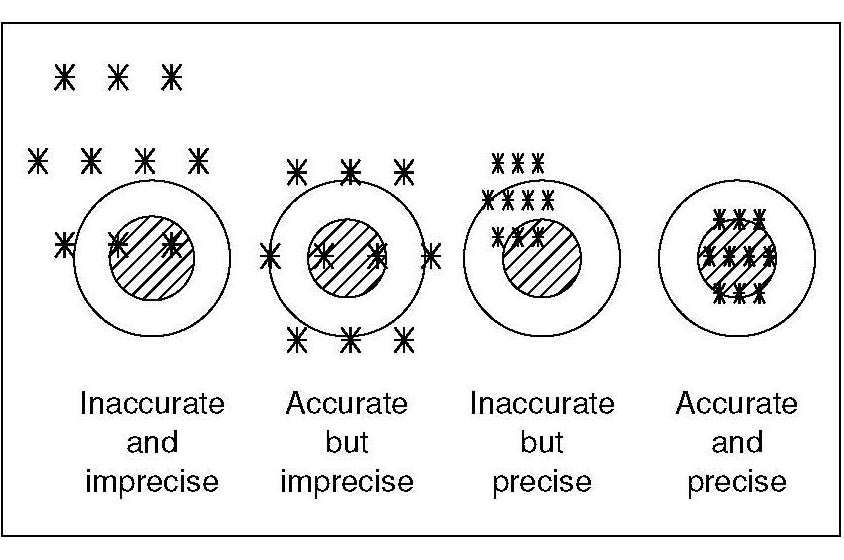 Table 1.5 Precision and accuracy of measurements. | Precision or reproducibility | Accuracy |
|---|
| Definition | The degree to which repeated measurements
of the same variable give the same value | The degree to which a measurement is close to
the true value | | Assess by | Comparison among repeated measures | Comparison with certified reference materials,
criterion method, or criterion anthropometrist | | Value to study | Increases power to detect effects | Increases validity of conclusions | Adversely
affected by | Random error contributed by
the measurer,
the respondent, or
the instrument | Systematic error (bias) contributed by:
the measurer,
the respondent, or
the instrument | 1.5.4 Random errors1.5.5 Systematic errors or bias- Drop-out bias is usually the result of ignoring possible systematic differences between those who fail to complete a study and the remaining participants.
1.5.6 Confounding- A confounder cannot be an intermediary step in the causal pathway from the exposure of interest to the outcome of interest.
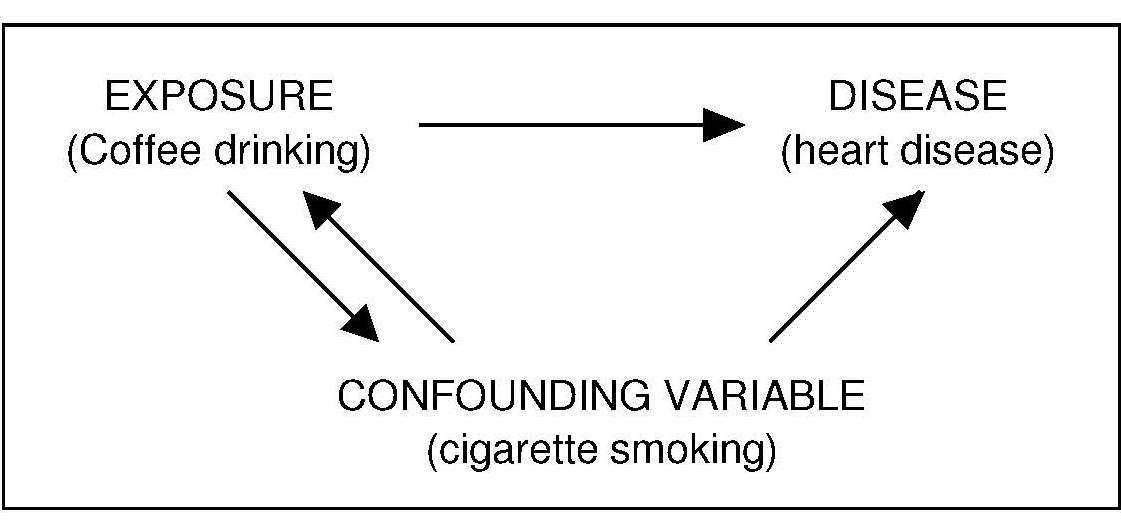 1.5.7 Sensitivity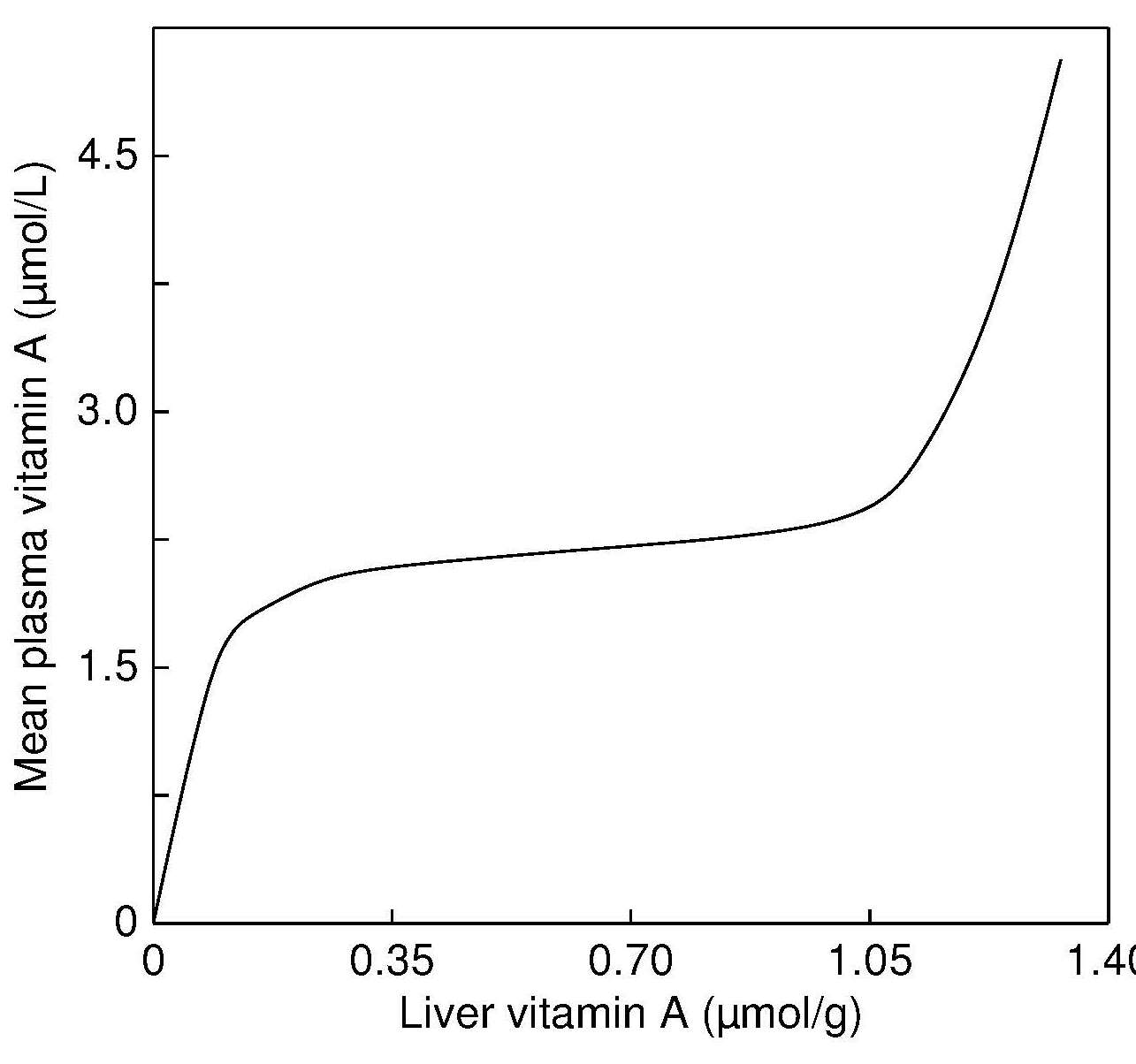 1.5.8 Specificity Table 1.6: Numerical definitions of sensitivity, specificity, predictive value, and prevalence for a single index used to assess malnutrition in a sample group.
Sensitivity (S ) = TP / (TP+FN)
Specificity (S ) = TN / (FP+TN)
Predictive value (V) = (TP+TN) / (TP+FP+TN+FN)
Positive predictive value (V+) = TP / (TP+FP)
Negative predictive value (V−) = TN / (TN+FN)
Prevalence (P) = (TP+FN) / (TP+FP+TN+FN)
From Habicht ( ). Test
result | The true situation:
Malnutrition present | The true situation:
No malnutrition |
|---|
| Positive | True positive (TP) | False positive (FP) | | Negative | False negative (FN) | True negative (TN) | Table 1.7. Sensitivity, specificity, and relative risk of death associated with various values for mid-upper-arm circumference in children 6–36mos in rural Bangladesh. Data from Briend et al. ( ). Arm circum-
ference (mm) | Sensitivity
(%) | Specificity
(%) | Relative Risk
of death |
|---|
| ≤ 100 | 42 | 99 | 48 | | 100–110 | 56 | 94 | 20 | | 110–120 | 77 | 77 | 11 | | 120–130 | 90 | 40 | 6 | Table 1.8. Impact of inflammation on micronutrient biomarkers of Indonesian infants of age 12mos. From Diana et al. ( ).
* Ferritin < 12µg/L
** RBP < 0.83µmol/L
*** Zinc < 9.9µmol/L | Biomarker in serum | Geometric mean (95% CI) | Proportion
at risk (%) | | Ferritin*: No adjustment | 14.5µg/L (13.6–17.5) | 44.9 | | Ferritin: Brinda adjustment | 8.8µg/L (8.0–9.8) | 64.9 | Retinol binding protein**:
No adjustment | 0.98 (µmol/L) (0.94–1.01) | 24.3 | Retinol binding protein:
Brinda adjustment | 1.07µmol/L (1.04–1.10) | 12.4 | | Zinc***: No adjustment | 11.5µmol/L (11.2–11.7) | 13.0 | | Zinc: Brinda adjustment | 11.7µmol/L (11.4–12.0) | 10.4 | 1.5.9 Prevalence1.5.10 predictive value. Table 1.9 Influence of disease prevalence on the predictive value of a test with sensitivity and specificity of 95%. From Dempsey and Mullen ( ). | Predictive Value | Prevalence
0.1% 1% 10% 20% 30% 40% | | Positive | 0.02 0.16 0.68 0.83 0.89 0.93 | | Negative | 1.00 1.00 0.99 0.99 0.98 0.97 | 1.6 Evaluation of nutritional assessment indices1.6.1 reference distribution. - REFERENCE INDIVIDUALS ↓ make up a
- REFERENCE population ↓ from which is selected a
- REFERENCE SAMPLE GROUP ↓ on which are determined
- REFERENCE VALUES ↓ on which is observed a
- REFERENCE Distribution ↓ from which are calculated
- REFERENCE LIMITS ↓ that may define
- REFERENCE INTERVALS
 1.6.2 Reference limits1.6.3 cutoff points.  1.6.4 Trigger levels for surveillance and public health decision making Table 1.10. Prevalence thresholds, corresponding labels, and the number of countries (n) in different prevalence threshold categories for wasting, overweight and stunting in children under 5 years using the “novel approach”. From de Onis et al. ( ). | Wasting | overweight | Stunting |
|---|
Prevalence
thresholds
(%) | Labels | (n) | Prevalence
thresholds
(%) | Labels | (n) | Prevalence
thresholds
(%) | Labels | (n) |
|---|
| < 2·5 | Very low | 36 | < 2·5 | Very low | 18 | < 2·5 | Very low | 4 | | 2·5 – < 5 | Low | 33 | 2·5 – < 5 | Low | 33 | 2·5 – < 10 | Low | 26 | | 5 – < 10 | Medium | 39 | 5 – < 10 | Medium | 50 | 10 – < 20 | Medium | 30 | | 10 – < 15 | High | 14 | 10 – < 15 | High | 18 | 20 – < 30 | High | 30 | | ≥ 15 | Very high | 10 | ≥ 15 | Very high | 9 | ≥ 30 | Very high | 44 | - Prevalence of serum zinc less than age/sex/time-of-day specific cutoffs is > 20%
- Prevalence of inadequate zinc intakes below the appropriate Estimated Average Requirement (EAR) is > 25%
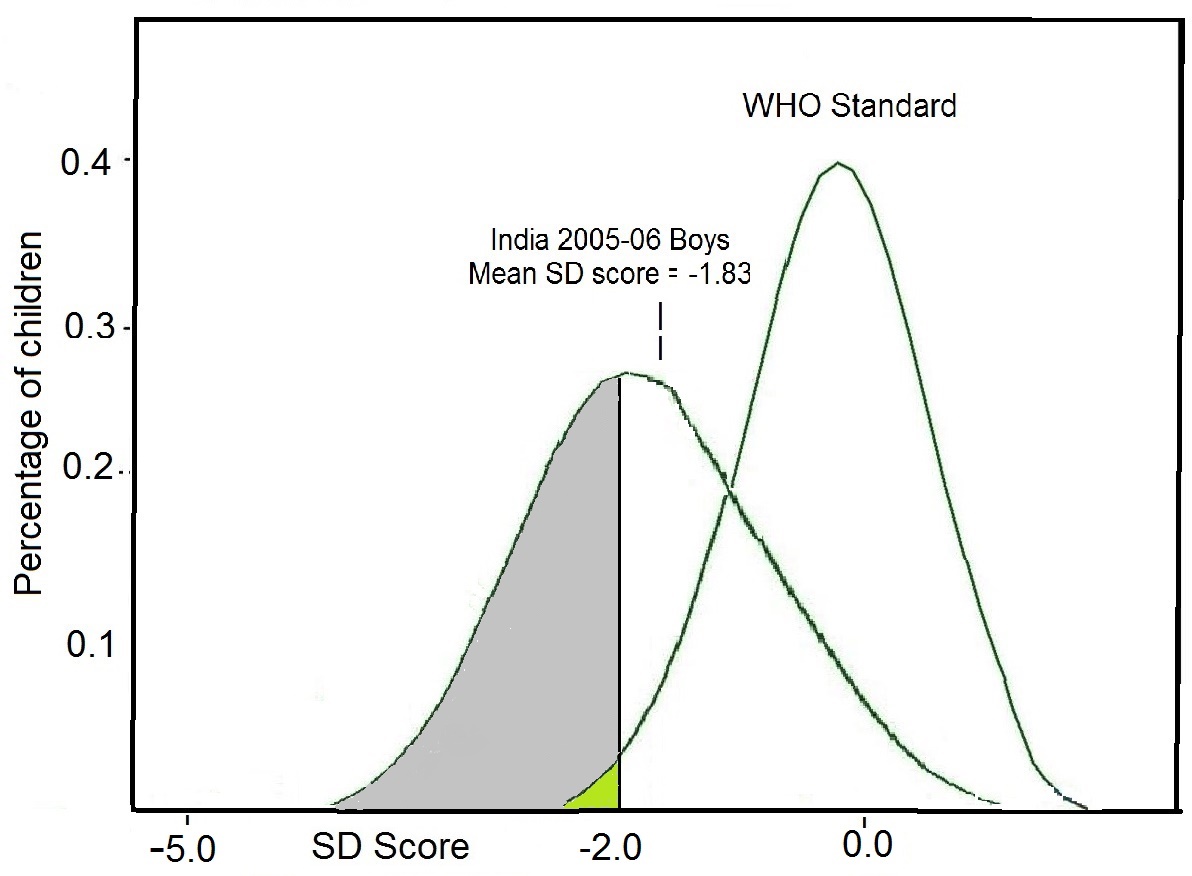
- Prevalence of low height-for-age or length-for-age Z‑scores (i.e., < −2SD) is at least 20%.
Nutritional Status: An Overview of Methods for Assessment- First Online: 02 April 2017
Cite this chapter - Catherine M. Champagne PhD (RDN, LDN, FADA, FAND, FTOS) 6 &
- George A. Bray M.D. 7
Part of the book series: Nutrition and Health ((NH)) 2389 Accesses This chapter focuses on the whole area of nutritional assessment and explores the wide spectrum of testing available that can aid in determining the health of an individual. This process typically includes in-depth evaluation of both subjective data and objective evaluations of an individual’s food and nutrient intake, components of lifestyle, and medical history. A nutritional assessment provides an overview of nutritional status; it focuses on nutrient intake analysis of the diet, which is then compared with blood tests and physical examination. With comprehensive data on diet and biological information, the physician can make an accurate estimate of that person’s nutritional status. Decisions can then be made on an appropriate plan of action to either maintain current health status or referral to counseling or other interventions that may enable the individual to reach a more healthy state. Only with sufficient anthropometric, biochemical, clinical, and dietary information can a plan be drafted. This is a preview of subscription content, log in via an institution to check access. Access this chapter- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
Tax calculation will be finalised at checkout Purchases are for personal use only Institutional subscriptions Similar content being viewed by others The Nutrition Assessment of Metabolic and Nutritional Balance Nutritional Status Evaluation: Body Composition and Energy BalanceOgden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–14. Article CAS PubMed PubMed Central Google Scholar Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011–2014. NCHS Data Brief. 2015;(219):1–8. Google Scholar Flegal KM, Panagiotou OA, Graubard BI. Estimating population attributable fractions to quantify the health burden of obesity. Ann Epidemiol. 2015;25:201–7. Article PubMed Google Scholar Blanton CA, Moshfegh AJ, Baer DJ, Kretsch MJ. The USDA automated multiple-pass method accurately estimates group total energy and nutrient intake. J Nutr. 2006;136:2594–9. CAS PubMed Google Scholar Ahluwalia N, Dwyer J, Terry A, Moshfegh A, Johnson C. Update on NHANES dietary data: focus on collection, release, analytical considerations, and uses to inform public policy. Adv Nutr. 2016;7:121–34. Article PubMed PubMed Central Google Scholar Bray GA. Review of: good calories, bad calories by Gary Taubes. New York: AA Knopf; 2007. Obes Rev. 2008;9:251–63. Article Google Scholar Archer E, Hand GA, Blair SN. Validity of U.S. nutritional surveillance: National Health and Nutrition Examination Survey caloric energy intake data, 1971–2010. PLoS One. 2013;8:e76632. Tooze JA, Vitolins MZ, Smith SL, et al. High levels of low energy reporting on 24-hour recalls and three questionnaires in an elderly low-socioeconomic status population. J Nutr. 2007;137:1286–93. Shaneshin M, Jessri M, Rashidkhani B. Validity of energy intake reports in relation to dietary patterns. J Health Popul Nutr. 2014;32:36–45. PubMed PubMed Central Google Scholar Scagliusi FB, Ferriolli E, Lancha Jr AH. Underreporting of energy intake in developing nations. Nutr Rev. 2006;64(7 Pt 1):319–30. Balkau B, Deanfield JE, Despres JP, et al. International Day for the Evaluation of Abdominal Obesity (IDEA): a study of waist circumference, cardiovascular disease, and diabetes mellitus in 168,000 primary care patients in 63 countries. Circulation. 2007;116:1942–51. Bray GA. Contemporary diagnosis and management of obesity. 3rd ed. Newtown: Handbooks in Health Care Co; 2003. Rothney MP, Brychta RJ, Schaefer EV, Chen KY, Skarulis MC. Body composition measured by dual-energy x-ray absorptiometry half-body scans in obese adults. Obesity. 2009;17:1281–6. Lazzer S, Bedogni G, Agosti F, De Col A, Mornati D, Sartorio A. Comparison of dual-energy x-ray absorptiometry, air displacement plethysmography and bioelectrical impedance analysis for the assessment of body composition in severely obese Caucasian children and adolescents. Br J Nutr. 2008;18:1–7. Shypailo RJ, Butte NF, Ellis KJ. DXA: can it be used as a criterion reference for body fat measurements in children? Obesity (Silver Spring). 2008;16:457–62. Nichols J, Going S, Loftin M, Stewart D, Nowicki E, Pickrel J. Comparison of two bioelectrical impedance analysis instruments for determining body composition in adolescent girls. Int J Body Compos Res. 2006;4:153–60. CAS PubMed PubMed Central Google Scholar Volgyi E, Tylavsky FA, Lyytikainen A, Suominen H, Alen M, Cheng S. Assessing body composition with DXA and bioimpedance: effects of obesity, physical activity, and age. Obesity (Silver Spring). 2008;16:700–5. Chen Z, Wang Z, Lohman T, et al. Dual-energy x-ray absorptiometry is a valid tool for assessing skeletal muscle mass in older women. J Nutr. 2007;137:2775–80. Neovius M, Hemmingsson E, Freyschuss B, Udden J. Bioelectrical impedance underestimates total and truncal fatness in abdominally obese women. Obesity (Silver Spring). 2006;14:1731–8. Drewnowski A. Obesity and the food environment. Dietary energy density and diet costs. Am J Prev Med. 2004;27(3S):154–62. Kant AK, Graubard BI. Energy density of diets reported by American adults: association with food group intake, nutrient intake, and body weight. Int J Obes. 2005;29:950–6. Article CAS Google Scholar Champagne CM, Casey PH, Connell CL, Lower Mississippi Delta Nutrition Intervention Research Initiative, et al. Poverty and food intake in rural America: diet quality is lower in food insecure adults in the Mississippi Delta. J Am Diet Assoc. 2007;107:1886–94. Stuff JE, Casey PH, Connell CL, et al. Household food insecurity and obesity, chronic disease, and chronic disease risk factors. J Hunger Environ Nutr. 2006;1:43–62. Hoy KM, Goldman JD. Fiber intake of the U.S. population: what we eat in America, NHANES 2009–2010. Food Surveys Research Group, Dietary Data Brief No. 12; 2014. Guenther PM, Casavale KO, Reedy J, et al. Healthy Eating Index 2010. Center for Nutrition Policy and Promotion. CNPP Fact Sheet No. 2. 2013. http://www.cnpp.usda.gov/sites/default/files/healthy_eating_index/CNPPFactSheetNo2.pdf . Accessed 22 Mar 2016. Suggested Further ReadingBray GA, Bouchard C. Handbook of obesity. Clinical applications. 4th ed. Boca Raton: CRC Press; 2014. Book Google Scholar Centers for Disease Control and Prevention . National Health and Nutrition Examination Survey (NHANES). Laboratory methods. http://www.cdc.gov/nchs/nhanes/nhanes2011-2012/lab_methods_11_12.htm . Food and Nutrition Board, Institute of Medicine—FNB. http://www.healthfinder.gov/orgs/HR0139.htm . Mahan LK, Raymond JL, Escott-Stump S, editors. Krause’s food & the nutrition care process. 13th ed. Philadelphia: W.B. Saunders; 2011. Schlenker E, Gilbert JA. Williams’ essentials of nutrition & diet therapy. 11th ed. Maryland Heights: Mosby; 2014. USDA, National Agricultural Library, Food and Nutrition Information Center. https://fnic.nal.usda.gov/ . Download references Author informationAuthors and affiliations. Department of Nutritional Epidemiology, Pennington Biomedical Research Center, Louisiana State University, 6400 Perkins Road, Baton Rouge, LA, 70808, USA Catherine M. Champagne PhD (RDN, LDN, FADA, FAND, FTOS) Pennington Biomedical Research Center, Louisiana State University, Baton Rouge, LA, USA George A. Bray M.D. You can also search for this author in PubMed Google Scholar Corresponding authorCorrespondence to Catherine M. Champagne PhD (RDN, LDN, FADA, FAND, FTOS) . Editor informationEditors and affiliations. Athabasca University Centre for Science, Athabasca, Alberta, Canada Norman J. Temple Winona State University Department of Biology, Winona, Minnesota, USA Louisiana State University Pennington Biomedical Research Center, Baton Rouge, Louisiana, USA George A. Bray Rights and permissionsReprints and permissions Copyright information© 2017 Springer International Publishing AG About this chapterChampagne, C.M., Bray, G.A. (2017). Nutritional Status: An Overview of Methods for Assessment. In: Temple, N., Wilson, T., Bray, G. (eds) Nutrition Guide for Physicians and Related Healthcare Professionals. Nutrition and Health. Humana Press, Cham. https://doi.org/10.1007/978-3-319-49929-1_35 Download citationDOI : https://doi.org/10.1007/978-3-319-49929-1_35 Published : 02 April 2017 Publisher Name : Humana Press, Cham Print ISBN : 978-3-319-49928-4 Online ISBN : 978-3-319-49929-1 eBook Packages : Medicine Medicine (R0) Share this chapterAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative Policies and ethics - Find a journal
- Track your research
BRILLIANT DIETITIANS A Registered Dietitian Resource The Dietitian’s Easy Guide To Nutrition Assessment [Free Pdf!]Updated: Feb 23, 2020 As a Registered Dietitian, I have to say that I LOVE doing Nutrition Assessments… Okay, I know not everyone shares my enthusiasm for this sometimes very tedious step of the Nutrition Care Process! Believe it or not, I used to dread the assessment, especially when the Nutrition-Focused Physical Exam (NFPE) became a “thing” for Dietitians. However, now that I really have it down to an organized and simple checklist, I really enjoy doing dietetic assessments! I promise to make this a very comprehensive, yet easy guide! My goal is to help you conduct an excellent nutrition assessment every time, and get really confident in your NFPE’s! Be sure to read on to the end of this post, because I have a totally FREE… Nutrition Assessment Checklist Pdf for you! In this comprehensive guide, you will learn: The Key Components of the Registered Dietitian’s Nutrition Assessment How to Easily Conduct a Patient Assessment of Nutrition Status And…You Will Take Home a FREE Nutrition Assessment Checklist (A Printable Pdf Just For YOU!)  Let’s start with the basics! Nutrition Assessment is the very first step in the Registered Dietitian Nutritionist’s Nutrition Care Process (NCP). The Two Purposes of the Nutrition Assessment: To collect as much data as possible about your patient. To interpret this data to help identify any nutrition-related problems, which leads into the second stage of the NCP, which is Nutrition Diagnosis. The Two Ways That Nutrition Assessment Data Are Collected: A Review Of The Patient’s Medical Records , including medical charts, nursing and physician assessments, and CNA records for food and fluid intake and any other details about feeding. You will want to check the diet order and any listed food allergies at admission (usually in the nurse’s assessment), and even call the dietitian at the previous facility the patient was at to determine the diet, nutritional diagnosis, and any nutrition interventions that may have previously been in place for the patient. A Patient Interview. During the interview, you will ask questions such as: what the patient’s usual body weight is, if there has been a recent weight loss, what the patient likes to eat, if they have been on a special diet order (to their knowledge), what foods they like and dislike, and if they have any food allergies. You will also want to ask about their appetite and if they have been eating less or more than usual. Often, it is helpful or necessary to involve the patient’s family members, especially if the patient is elderly and with any cognitive impairment, or if the patient is a child. Caregivers often provide useful information for your nutrition assessment. The 5 Categories of Nutrition Assessment 😀 One of the reasons I enjoy nutrition assessments is that they are like finding treasure that you can sort into 5 different categories. This is a fun process if you get the hang of it, and the organization of the 5 parameters helps you get all your ducks in a row before moving on to your nutrition diagnosis. 😀 I like to organize this data into an easy chart/checklist format, which, like I promised, I will provide to you for free at the end of this post! First, read on so you understand what a comprehensive assessment entails. For all 5 categories, you will gather information from both the medical records and the patient interview. 😀 TIP: Whenever possible, always review the records before seeing the patient! This will enable you to have a thorough picture of the medical status, diagnoses, medications, and more before you see the patient! Usually, you will already have some ideas in place before you see the patient (such as supplements that might be needed) that you will want to ask the patient about. This can save a lot of time , especially when there is a high RD-to-patient ratio, and you will not have to re-visit patient rooms so often! *Here are your 5 assessment categories: Category 1: Food/Nutrition-Related History Diet Order - written on medical record on nurse’s intake. Check medical records for continuity of previous diet if patient was transferred from another facility. Food Allergies and Intolerances - list any on medical record and verify with patient about food allergies. Food and Nutrient Intake - *ask the patient AND check the CNA records Food and Nutrient Administration - ex. oral, tube feeding, etc. Patient’s Appetite - including recent changes - ask the patient/caregiver Patient’s Usual Diet - ask the patient/caregiver Physical Activity Level - needed for nutrition needs calculation (ex. bed-bound, sedentary, light activity). Category 2: Anthropometric Measurements Current Body Weight (CBW) Body Mass Index (BMI) Ideal Body Weight (IBW) Percent of Ideal Body Weight (%IBW) Recent Weight Change & Weight History : ask patient and check medical records to identify a recent weight loss or gain. Estimated nutrition requirements: Total Calories, Protein needs, Fluid needs. Use Mifflin St Jeor or other appropriate equation with Injury or Activity Factor adjustment. Growth Charts & Percentile Ranks : for children Waist Circumference or Waist-to-Hip ratio/WHR (used in some outpatient or bariatric settings to evaluate as a parameter for metabolic syndrome and obesity-related disease risk) Category 3: Biochemical Data, Medical Tests, and Procedures Blood/Lab work : including electrolytes, blood glucose, lipid testing, visceral proteins. Examine and record findings of any available nutrition-related labs. Imaging : X-rays, MRIs, CT Scans and the related findings. Other testing : gastric emptying study, gallbladder testing, resting metabolic rate etc. Category 4: Nutrition-Focused Physical Findings Nutrition-Focused Physical Exam (NFPE) : includes oral health such as dentures and tooth pain, skin turgor and integrity, loss of subcutaneous fat/muscle mass, etc. Swallowing and Chewing Status - dysphagia, dentition, oral sores, etc. Physical Findings of Vitamin and Mineral Deficiencies Evaluate for Characteristics of Malnutrition : insufficient energy intake, recent weight loss, loss of subcutaneous fat, loss of muscle mass, fluid accumulation that may mask weight loss or be a sign of protein deficiency, diminished functional status, grip strength (if grip strength tools are available). Go to "A Guide to The Nutrition-Focused Physical Exam" to learn more! Category 5: Client History Here you will chart current and past Medical, Surgical, Family, and Social History, with a focus on identifying any nutritionally relevant medical issues. MEDICAL/HEALTH Diagnoses - list all you find on medical record Skin/Wound Status - nurse’s intake - this determines if supplementation may be needed to meet nutritional needs for wound healing (protein, vitamin C, zinc, etc). Recent Surgeries and Procedures - including colonoscopy, orthopedic surgery, etc) Past Medical History, Surgical History, Family Medical History MEDICATIONS Medications and Supplements - usually on medical record on nurse’s intake Allergies - list any on medical record and verify with patient. Note any nutritionally relevant drug side effects like loss of taste, smell, appetite, weight loss/gain, as well as potential drug/nutrient interactions. Any personal/social factors that may affect food intake and availability , such as cognitive capacity, communication or language barriers, income, occupation, education level, use of/eligibility for government programs, motivation level, person responsible for shopping, preparing food at home. FOOD AND NUTRITION Food intake : Dietary recall or food frequency analysis if appropriate setting and time allowance with patient. Knowledge and Beliefs about food; food availability; nutrition quality of life Eating habits and patterns : usual and current appetite, weight history, physical or mental abilities that may affect food intake and self-feeding, typical diet and meal pattern, ethic or religious food preferences. Lifestyle habits and patterns : Alcohol intake, smoking, frequency of dining out, physical activity type/frequency, previous diet education, interest in dietary change, complimentary and alternative medicine use. ARE YOU OVERWHELMED YET? I know, it really looks like a lot! However, I promise you that… Practice makes progress, and progress makes perfect! Over time, going through the assessment steps, you will be surprised at how well it becomes an automatic and easy process for you. In the meantime, I created a *FREE Nutrition Assessment Pdf* just for you! I organize the step sof assessment into actions that make sense. This blog contains the "textbook" description of nutrition assessment, but in practice most RDNs do not take the steps in the order they are written. THAT is why I created this Pdf for you! You can print it and go through the checklist with each patient until you get the hang of it. This is what I WISH I had when I stepped into my dietetic career! And it’s your’s free compliments of Brilliant Dietitians when you subscribe at the bottom of the page. We will deliver it straight to your inbox! Next, be sure to read: "A Guide to The Nutrition-Focused Physical Exam " “ Have a fantastic day and get out there and BE A BRILLIANT DIETITIAN! ” Your Brilliant Dietitian Coach Blog Sources: Width, M. & Reinhard, T. (2018). The Essential Pocket Guide for Clinical Nutrition, 2nd Ed. Philadelphia, PA: Wolters Kluwer. - Medical Nutrition Therapy
- Nutrition Care Process
Recent PostsNutrition Interventions and the Nutrition Prescription Nutrition Diagnosis and PES Statements A Guide To The Nutrition Focused Physical Exam  An official website of the United States government The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site. The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely. - Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now . - Advanced Search
- Journal List
- Clin Interv Aging
Assessment and management of nutrition in older people and its importance to healthNutrition is an important element of health in the older population and affects the aging process. The prevalence of malnutrition is increasing in this population and is associated with a decline in: functional status, impaired muscle function, decreased bone mass, immune dysfunction, anemia, reduced cognitive function, poor wound healing, delayed recovery from surgery, higher hospital readmission rates, and mortality. Older people often have reduced appetite and energy expenditure, which, coupled with a decline in biological and physiological functions such as reduced lean body mass, changes in cytokine and hormonal level, and changes in fluid electrolyte regulation, delay gastric emptying and diminish senses of smell and taste. In addition pathologic changes of aging such as chronic diseases and psychological illness all play a role in the complex etiology of malnutrition in older people. Nutritional assessment is important to identify and treat patients at risk, the Malnutrition Universal Screening Tool being commonly used in clinical practice. Management requires a holistic approach, and underlying causes such as chronic illness, depression, medication and social isolation must be treated. Patients with physical or cognitive impairment require special care and attention. Oral supplements or enteral feeding should be considered in patients at high risk or in patients unable to meet daily requirements. IntroductionMalnutrition is defined as a state in which a deficiency, excess or imbalance of energy, protein and other nutrients causes adverse effects on body form, function and clinical outcome. 1 It is more common and increasing in the older population; currently 16% of those >65 years and 2% of those >85 years are classed as malnourished. 2 These figures are predicted to rise dramatically in the next 30 years. Almost two-thirds of general and acute hospital beds are used by people aged >65 years. 3 Studies in developed countries found that up to 15% of community-dwelling and home-bound elderly, 23% to 62% of hospitalized patients and up to 85% of nursing home residents suffer from malnutrition. 4 Malnutrition is associated with a decline in functional status, impaired muscle function, decreased bone mass, immune dysfunction, anemia, reduced cognitive function, poor wound healing, delayed recovering from surgery, higher hospital and readmission rate, and mortality. 5 The etiology is multifactoral and will be discussed at length under several headings - Biological changes of the digestive system with aging
- Physiological changes of the digestive system with aging
- Nutritional assessment in older people
- Pathological and non-pathological weight loss in older people
Biological changes of the digestive systemThere are age-related changes in the gastrointestinal tract. The difficulty is that with age it can be difficult to exclude pathological factors such as diabetes, pancreatitis, liver disease and malignancy, since these factors will have potential adverse effects on the intestine. Selective neurodegeneration of the aging enteric nervous system can lead to gastrointestinal symptoms such as dysphagia, gastrointestinal reflux and constipation. 6 Caloric reduction in rodents can prevent neuronal loss, suggesting that diet may influence the aging gut. 7 Esophageal motility may reduce the reduction of neurons in the mesenteric plexus in older people. 8 Gastric motility is impaired with aging 9 but the small intestine is unaffected. 10 With age colonic motility can be influenced by signal transduction pathways and cellular mechanisms that control smooth muscle contraction which could lead to constipation. 11 Reduced gastric acid secretions have an increasing prevalence with aging. Hypochlorhydia occurs due to chronic gastritis. Consequently, proton pump inhibitors are frequently used for prolonged periods in older people leading to suppressed acid secretions. Procedures such as vagotomy and gastric resections (both seen in older people) cause reduced acid levels. The overall reduction in acid secretions predisposes the gut to small bowel bacterial overgrowth. 12 One study highlighted that 71% of patients on a geriatric ward had bacterial overgrowth of the small intestine and 11% were found to be malnourished. 13 Bacterial overgrowth has been proven to be associated with reduced body weight and reduced intake of micronutrients. 14 Structural changes of the pancreas are seen with aging, but no functional age-related changes are seen with the fluorescein dilaurate test. 15 Secretagogue-stimulated lipase, chymotrypsin and bicarbonate concentration in pancreatic juice have all been shown to decline with aging. 16 Other studies found little evidence of reduced pancreatic secretion with age-independent of factors such as disease and drugs. 17 The liver declines in size and blood flow with age but microscopic changes are subtle. 18 In mice with age it has been shown that changes in the expression of genes in the liver are involved in inflammation, cellular stress and fibrosis. 19 Caloric restriction in mice appeared to reverse age-related changes, indicating that diet influences age-related changes. 20 Changes can occur in the small intestine such as decline in the number of villi and crypts, 18 loss of villi and enterocyte height 21 and decline in mucosal surface. 22 However, there is no clear association between intestinal morphology and nutrient uptake with aging. 23 Physiological changes of digestive system and agingThe anorexia of aging. With increasing age appetite declines and food consumption declines. Healthy older people are less hungry and are fuller before meals, consume smaller meals, eat more slowly, have fewer snacks between meals and become satiated after meals more rapidly after eating a standard meal than younger people. The average daily intake of food decreases by up to 30% between 20 and 80 years. 24 Most of the age-related decrease in energy is a response to the decline in energy expenditure with age. However in many older people the decrease in energy intake is greater than the decrease in energy expenditure, and therefore body weight is lost. This physiological age-related reduction in appetite and energy intake has been termed the “anorexia of aging” ( Figure 1 ). 4  A depiction of the “anorexia of aging”. Abbreviation: GI, gastrointestinal. Changes in body weight and body compositionCross-sectional studies have shown that body weight and body mass index (BMI) increase with age until approximately 50 to 60 years, after which they both decline. 25 A 2-year prospective study showed that community-dwelling American men aged >65 years lost an average of 0.5% of their body weight per year and 13.1% of the group had a weight loss of 4% per year. 26 A prospective cardiovascular health study looked at 4714 home-dwelling subjects > 65 years who did not have cancer. 27 In the 3 years after the study entry 17% had lost 5% or more of their initial body weight. This group were shown to have increased risk-adjusted mortality over the next 4 years compared to the group with stable weight. There is a J shaped curve association with mortality and body weight with increased mortality with low and high BMIs. 28 At a BMI < 22 there is a steady increase in mortality and the combined effect of being underweight and increasing age has a deleterious effect on mortality. 29 With age, body fat increases and fat-free mass decreases because of loss of skeletal muscle, with a loss of up to 3 kg of lean body mass per decade after the age of 50. The mean body fat of a 20-year-old man weighing 80 kg is 15% compared to 29% in 75-year-old man of the same weight. 30 The cause of increase fat is multifactoral: reduced physical activity, reduced growth hormone secretion, diminished sex hormones and decreased resting metabolic rate. The distribution of fat in older people is different from that of younger people. A greater proportion of body fat is intra-hepatic and intra-abdominal, which is associated with insulin resistance 31 and higher risk of ischemic heart disease, stroke and diabetes. Etiology of weight lossThree distinct mechanisms of weight loss in older people have been identified 32 Wasting, an involuntary loss of weight, is mainly due to poor dietary food intake which can be caused by disease and psychological factor causing an overall negative energy balance. Cachexia is an involuntary loss of fat-free mass (muscle, organ, tissue, skin and bone) or body cell mass; it is caused by catabolism and results in changes in body consumption. An acute immune response occurs. Cytokines are released (interleukin [IL]-1, IL-6, tumor necrosis factor alfa [TNFα]) that have profound effects on hormone production and metabolism causing increased resting energy expenditure. 33 Amino acids from muscle to the liver, an increase in gluconeogenesis and a shift of albumin production to acute phase proteins causes nitrogen balance to become negative, so muscle mass is lost. Cachexia is seen in many chronic diseases such as heart failure and rheumatoid arthritis. It is also seen in malignancy. The major age-related physiological change in older people is a decline in skeletal muscle mass, known as sarcopenia. 34 Reduced physical activity has a crucial role since lack of exercise causes muscle disease and, with time, muscle loss. However, lack of exercise is not the only cause and it is thought that hormonal, neural and cytokine activities play a role. 32 Increased cytokine activity increases levels of acute phase proteins which break down muscle. Levels of sex hormones, glucocorticoids and catecholamines decline in older people which in turn increase pro-inflammatory cytokines. The central nervous system can play a part in sarcopenia. Neurones lost from the spinal cord will lead to loss of muscle. 35 Also the remaining neurones adopt muscle fibers and control larger units of muscle cells causing the units to become less efficient, which leads to weakness. Stroke and neural disease cause neurone cell death and result in muscle atrophy. Physiological anorexiaCauses of physiological anorexia are not fully understood, but the following are thought to contribute: - Diminished sense of smell and taste
- Increased cytokine activity
- Delayed gastric emptying
- Altered gastric distension
Taste and smell make food enjoyable. The sense of taste and smell deteriorate with age. In one study more than 60% of subjects 65 to 80 years and more than 80% of subjects aged >80 years had developed a reduced sense of smell and taste compared to less than 10% of those <50 years old. 36 The decline in sense of smell decreases food intake in older people and can influence the type of food eaten, and it has been shown that a reduced sense of smell is associated with reduced interest in and intake of food. Also, older patients with a reduced sense of taste tend to have a less varied diet and consequently develop micronutrient deficiencies. The loss of sense of taste is not understood fully but may be caused by a reduced number of taste buds. 37 Modifications in the olfactory epithelium, receptors and neural pathways may affect sense of smell. Drugs such as Parkinson’s medications and antidepressants affect sense of taste. Studies have shown that improving flavor of foods can improve nutritional intake and body weight in nursing-home patients. 38 The role of cytokines has been discussed earlier. Circulating levels of IL1, IL6 and TNFα have been shown to be higher in older people and associated with reduced muscle mass. Older people commonly complain of increased fullness and early satiation during a meal which may be caused by changes in gastrointestinal sensory function, as with age there is reduced sensitivity to gastrointestinal distension. Aging is associated with impairment of receptive relaxation of the gastric fundus, causing rapid antral filling and distension and earlier satiety. 39 In a study in which young and old men were underfed by approximately 750 kcal/day for 21 days, both groups of men lost weight. 40 After the underfeeding period the men were allowed to eat freely. The young men ate more than at baseline and quickly returned to their normal weight, whereas the older men did not compensate and returned to their baseline intake and did not regain weight. The combination of age-related physiological anorexia and impaired homeostasis means older people do not respond to acute undernutrition compared with young men. The hypothalamus controls hunger and satiety. The nucleus arcuatus has neurones that release neuropeptide Y (NPY), an agouti-related peptide, which mediates hunger and inhibit satiety. 41 Pro-opiomelacortin, which is produced in the nucleus arcuatus, stimulates satiety. 41 Peripheral hormones affect the hypothalamus hunger–satiety control regulation. Cholecystokinin (CCK) is released in the proximal bowel and is the protype satiety hormone. It is released in the response to nutrients from the antrum, particularly lipids and proteins. 42 It has been shown to be increased in older people and correlated with high levels of satiety and low hunger. 43 Pancreatic polypeptide (PPY) is released by the distal intestine in the presence of nutrients in the lumen. 44 PPY inhibits NPY and causes satiety. Both CCK and PPY are enteric peptides involved in gastrointestinal motility in response to eating. 45 High levels of fasting and postprandial CCK and PPY may cause prolonged satiety by slowing antral emptying. Leptin is a hormone produced by adipose cells whose main role is maintaining energy balance. Low leptin signals loss of body fat and a need for energy intake, while high leptin level implies adequate body fat and no need for further food intake. 41 Older people tend to have higher levels of leptin. 46 Insulin regulates glucose metabolism. It is a satiety hormone that works by enhancing the leptin signal to the hypothalamus and inhibiting gherlin, the only peripheral hormone known to stimulate appetite. 47 It is produced and secreted in the endocrine mucosa to enhance food intake. Aging is associated with reduced glucose tolerance and elevated insulin levels, which may amplify the leptin signal 48 and inhibit ghrelin. 49 Nutritional assessmentDietary assessment. Quantifying nutritional intake is best preformed by a dietitian. Different methods can be used. Twenty-four hour recall is commonly used and is based on an interview during which the patient recalls all food consumed in the previous 24 hours. 50 The main disadvantages are that it represents only food intake for 1 day and may not represent a patient’s typical intake. Data can also be affected if the patient has cognitive impairment. Food records for 7 days for all food and drink consumed can be used and help eliminate day-to-day variations. A food frequency multiquestion questionnaire is used to explore dietary intake over a period of time. 51 This is more suitable for evaluation of groups rather than individuals. Unintentional weight loss is one of the best predictors of worst clinical outcome and in older people is associated with significant morbidity and mortality. 52 Clinical assessmentA large number of clinical signs indicate nutritional deficiencies. The general impression is a wasted, thin individual with dry scaly skin and poor wound healing. The hair is thin and nails are spooned and depigmented. Patients complain of bone and joint pain and edema. Specific nutritional deficiencies are associated with specific clinical signs (see Table 1 ). Clinical signs and nutritional deficiencies | | | |
|---|
| Skin | Dry scaly skin | Zinc/essential fatty acids | | Follicular hyperkeratosis | Vitamin A, C | | Petechiae | Vitamin C, K | | Photosensitive dermatitis | Niacin | | Poor wound healing | Zinc, vitamin C | | Scrotal dermatitis | Riboflavin | | Hair | Thin/depigmented | Protein | | Easy pluckability | Protein, zinc | | Nail | Transverse depigmentation | Albumin | | Spooned | Iron | | Eyes | Night blindness | Vitamin A, zinc | | Conjunctival inflammation | Riboflavin | | Keratomalacia | Vitamin A | | Mouth | Bleeding gums | Vitamin C, riboflavin | | Glositis | Niacin, piridoxin, riboflavin | | Atrophic papillae | Iron | | Hypogeusia | Zinc, vitamin A | | Neck | Thyroid enlargement | Iodine | | Parotid enlargement | Protein | | Abdomen | Diarrhea | Niacin, folate, vitamin B12 | | Hepatomegaly | Protein | | Extremities | Bone tenderness | Vitamin D | | Joint pain | Vitamin C | | Muscle tenderness | Thiamine | | Muscle wasting | Protein, selenium vitamin D | | Edema | Protein | | Neurological | Ataxia | Vitamin B12 | | Tetany | Calcium, magnesium | | Parasthesia | Thiamine, vitamin B12 | | Ataxia | Vitamin B12 | | Dementia | Vitamin B12, niacin | | Hyporeflexia | Thiamine |
Screening toolsThe Malnutrition Universal Screening Tool (MUST) is a five-step screening tool to identify adults who are malnourished or at risk of malnutrition. 53 It includes management guidelines that can be used to develop a care plan. The tool is being used both in hospitals and in the community. The tool is easy to use and can be used by all care workers to derive a malnutrition risk score of either low, medium or high. It consists of three components: BMI, history of unexplained weight loss, and acute illness effect. Studies have shown that it has a high predictive validity in the hospital environment (length of stay, mortality in older people, and discharge destination in orthopedic patients). 54 It is more efficient and faster than most other screening tools (3 to 5 minutes). 55 It has been recommended as a screening tool by the National Institute of Clinical Excellence (NICE), the British Association for Parental and Enteral and Nutrition (BAPEN) and the British Dietitian Association (BDA). The Mini Assessment (MNA) and Malnutrition Risk Scale (SCALES) were specifically designed for older patients. The MNA test consists of 18 items and takes less than 15 minutes to perform. It has been shown to predict morbidity and mortality in a study of an elderly Danish population. 56 The SCALES (S-sadness C-Cholesterol A-Albumin L-Loss of weight E-Eating problem physical/cognitive S-Shopping problems) test was designed for outpatient screening. The subjective global assessment relies on physical signs of undernutrition and patient history and does not use laboratory findings. It is simple to use, quick (takes a few minutes) and has been shown to be reliable in elderly outpatients. 57 Anthropometric assessmentThe Quetelet index relates weight (kg) to the square of the height (m 2 ), which enables calculation of body mass index (BMI). 58 It predicts disease risk in those termed underweight and in those who are obese. The World Health Organization categorizes underweight as BMI < 18.5, normal 18.5 to 24.9, overweight 25 to 29.9 and obese 30 to 39.9, and extreme obesity > 40. 59 The further a patient moves outside the normal reference range the more the association with morbidity and mortality increases. 60 Measurement of BMI in older people has certain limits such as loss of height caused by vertebral collapse, change in posture and loss of muscle tone. In these cases height should be obtained from certain body segments, such as leg, arm and arm span. 61 BMI can be unreliable in the presence of confounding factors such as ascites and edema. In addition it does not identify unintentional weight loss as a single assessment. Skinfold measurement using tricipital skinfold is particularly important together with arm circumference, and can be used to calculate muscular circumference of the arm, which indicates lean mass. 62 Mid-upper arm circumference is a helpful indicator of malnutrition in ill patients (normal 23 cm in males, > 22 cm females). This measurement has been shown to be an independent predictor of mortality in older people in long-term institution. 63 A formula (Haboubi-Kennedy) has been devised using both BMI and mid-arm circumference to evaluate nutritional status. 64 Biometric impedance analysis is a simple, non-invasive and inexpensive method to estimate total body water, extracellular water, fat-free mass and body cell mass. It is a measurement of the resistance that the body provides against the passing of an electric current. Several studies have demonstrated that low body cell mass has a prognostic value in malnourished patients. 65 Using anthropometric data a study tried to obtain reference values for various body compartments. However the upper age group in the study was 64, and therefore at present there are a lack of data in older age groups. 66 Biochemical markersSerum proteins synthesized by the liver have been used as markers of nutrition albumin, transferrin, retinol-binding proteins and thyroxine-binding prealbumin. 67 Serum albumin is the most commonly used marker since it can predict mortality in older people. However albumin can be affected by not only nutritional state but by other factors, including inflammation and infection. This limits their usefulness especially in acutely unwell patients. Albumin has a long half-life and therefore is not useful for looking at short-term changes in protein and energy intake. 68 Transferrin is a more sensitive marker of early protein-energy malnutrition but is affected by a number of conditions including pregnancy, iron deficiency, hypoxia, chronic infection and hepatic disease. 68 Malnutrition impairs the immune system and decreases lymphocyte proliferation. 69 Low total serum cholesterol has been associated with increased risk of malnutrition. 70 Assessment of vitamins and trace elements is also important since deficiencies can lead to medical complications. To date there is no single biochemical marker of malnutrition as a screening test. The main value of biochemical markers is in a detailed assessment and monitoring. Pathological and non-pathological causes of weight lossPathological factors become more common with age and most causes are treatable. This treatment can be medical, social or psychological. - Cardiac eg, chronic heart failure
- Respiratory disease, eg, chronic obstructive pulmonary disease
- Gastrointestinal, eg, malabsorption syndromes, dysphagia, Helicobacter pylori , atrophic gastritis
- Endocrine disorders, eg, diabetes thyrotoxicosis
- Neurological, eg, stroke, Parkinson’s disease, motor neurone disease
- Infection, eg, pneumonia, urinary tract infection
- Physical disability, eg, arthritis
- Poor dentition
Drugs that may cause anorexia in older people | | |
|---|
| Cardiovascular | Amiodorone, frusemide, digoxin, spironolcatone | | Neurological | Levodopa, fluoxetine, lithium | | Gastrointestinal | H2 antagoinsts, PPI | | Antibiotics | metronidazole, griseofluvin | | Chemotherapies | Any | | Musculoskeletal | colchicines, NSAIDs, penicillamine, methotrexate |
Abbreviations: NSAIDs, non-steroidal anti-inflammatory drugs; PPI, proton pump inhibitors. Psychological- Dementia/Alzheimer’s disease
- Bereavement
- Inability to shop, prepare and cook meals
All the diseases mentioned above are associated with higher rates of malnutrition in older people. Many older people do not have their own teeth – 59% aged 65 to 74 use dentures according to one survery. 71 Poor dentition and ill-fitting dentures may limit the type and quantity of food they eat. Chewing problems are associated with a greater likelihood of poor health and decreased quality of life. 72 Depression is common in older people and can present in 2% to 10% of the community. 73 One of the most common presentations is loss of appetite and weight loss. It has been documented that 30% to 36% of weight loss seen in outpatients and the nursing home is due to depression. 74 An inverse relationship between energy intake and cognition has been shown in hospital patients with dementia. 75 Weight loss and changed behavior are associated with late stage disease. Fifty percent of patients with Alzheimer’s cannot feed themselves 8 years after their diagnosis. 76 Also olfactory changes occur in Alzheimer’s which may affect food intake. 77 Older people living on their own and socially isolated tend to eat less. These same people eat up to 50% more with company. 78 Macronutrients and micronutrientsThe recommended dietary allowance (RDA) for protein is 0.8 g protein/kg body weight per day for adults regardless of age. 78 This is the minimum amount of protein intake required to avoid progressive loss of lean body mass. Evidence has revealed that protein intake greater than the RDA helps to improve muscle mass, strength and function in older people. Furthermore this intake can improve immune status, wound healing and blood pressure. 79 Concerns about the detrimental affects of increased protein intake on bone health, renal function, neurological function and cardiovascular function are generally unfounded. It has been recommended that the RDA intake of 1.5 g protein/kg body weight per day is a reasonable intake in older people to optimize protein intake in terms of health and function. 80 Reduced intake and unbalanced diet predispose older people to vitamin and mineral deficiencies. Drugs can affect the absorption of vitamins, and can also interfere with hepatic metabolism, causing delayed elimination of vitamins. Smoking interferes with absorption of vitamins, particularly vitamin C and folic acid. Older people do not clear vitamin A well and are subsequently prone to hypervitaminosis. Reduced vitamin D can result from reduced dietary consumption, and gastrointestinal and renal disease. Vitamin D deficiency leads to osteomalacia, rickets and myopathy. It is associated with reduced bone density, impaired mobility, increased risk of falls and probably an increased risk for developing type 1 diabetes, cardiovascular disease and rheumatoid arthritis. 81 Dietary requirements in older people are higher due to reduced skin production, decreased exposure to sunlight and thinning of the skin. Vitamin B12 def iciency occurs in 12% to 14% of community-dwelling in people >60 years of age and up to 25% of institutionalized older people. 82 It can cause macrocytic anemia, subacute combined degeneration of the spinal cord, neuropathies, ataxia, glossitis and dementia. 83 It also causes an increased level of homocystine, which increases risk of cardiovascular disease, 84 and is associated with reduced bone density and increased hip fracture rate. 85 In older people atrophic gastritis and pernicious anemia are the most common causes of vitamin B12 deficiency; less common causes are a strict vegetarian diet over a period of time (10 to 30 years) or inadequate absorption after gastrectomy or illeostomy. Folate is present in orange juice, dark green leafy vegetables, peanuts, strawberries, dried beans and peas, and asparagus, among others. Four to 50% of older people have been reported with folate deficiency, with higher levels in those institutionalized. 86 It causes macrocytic anemia and increased homocystine level, and is associated with increased risk of colorectal cancer, possibly cervical cancer, and cognitive impairment and depression. 86 The main cause is due to diet insufficiency. Other causes are drugs (eg, methotrexate) and excess alcohol consumption. Mineral requirements in old age do not change. Zinc, selenium, chromium, copper and manganese levels are unchanged with healthy aging. Fluid and electrolyte regulationOlder people are more susceptible to develop problems with fluid and electrolyte balance due to physiological renal impairment and changes in thirst perception. Fluid deprivation and repletion studies comparing younger adults with the older population have demonstrated that despite physiological needs, older people do not consume adequate amounts of fluids to maintain ideal plasma electrolyte concentrations. 87 , 88 This impaired fluid and electrolyte balance is due to several factors, including reduced glomerular filtration rate, reduced ability to concentrate urine, less efficient sodium-conserving capacity, reduced ability to excrete water load and altered thirst sensation. 87 , 88 Fluid intake in older people can be further affected by physical disability and cognitive impairment. Adverse effects of drugs such as diuretics, either by altering thirst or prompting dieresis, cause dehydration. Nutritional therapy in older peopleReduced intake due to medical, social and physiological factors should be addressed. For example patients with difficulty chewing should have dental and oral care checked and possibly be given mushy food. Patients with difficulty swallowing, eg, stroke patients, need speech and language therapy and possibly percutanous endoscopic gastrostomy (PEG) feeding. Patients with physical difficulties should have nursing assistance and those with low mood should have their medication reviewed and, if needed, started on appropriate treatment. Older people in isolation should have social services assistance and ‘meals on wheels’ to help improve food intake. Older people in general have reduced oral intake. The main goal should be to help improve oral food intake. A study looking at hospital patients from different specialities demonstrated that 40% of food was wasted and that energy and protein intake was less than 80% of that recommended. 89 Forty-two percent of older patients stated meal sizes were too large. Another study looked at older people receiving either normal or a reduced portion size fortified menu which provided 14% more energy than the normal menu. Intake was 25% higher on the fortified menu. 90 A study using fortified menu demonstrated that between-meal snacks were also suitable to improve energy intake in older people in hospital. 91 Modifying the dining environment in care homes has been shown to improve dietary intake. For example providing cafeteria style meals over a course of 3 weeks compared to traditional meal delivery on trays at one long-term home significantly increased energy intake. 92 A 20-day trial at another care home showed that verbal cuing and individual physical guidance improved dietary intake by 29% to 56%. 93 Food texture preferences were felt to be beyond the scope of this review article. In patients with proven deficiencies of micronutrients, supplementation should be given. Calcium and vitamin D supplementation have been shown to reduce the incidence of hip fractures. 94 Oral liquid energy-dense and high-quality protein supplements have been shown to increase energy and protein intake in critically ill patients. 95 Supplements have also been shown to improve clinical and functional outcomes and reduce mortality rate. Enteral feeding is indicated if a patient is severely malnourished or if food cannot be taken orally due to medical illness, eg, stroke. In the short term, a nasogastric tube can be used and in the longer term PEG is indicated. Overnutrition in older peopleThe prevalence of overweight (using standard BMI criteria) older people in Westernized countries is increasing. In 2000, 58% of US citizens aged ≥65 years had a BMI of ≥25 96 and the prevalence of obesity (BMI > 30) in the US increased 36% from during 1991 to 2000. 97 The relative risk of death in older people with high BMI is not as great as in younger people, but nevertheless is associated with a similar increased risk of mortality from conditions such as diabetes, hypertension and cardiovascular disease. Also older people with high BMI suffer from symptomatic osteoarthritis, increased rates of cataracts, mechanical urinary and bladder problems, and sleep apnea and other respiratory problems. Although intentional weight loss by overweight older people is probably safe and beneficial, caution should be exercised in recommending weight loss to overweight older people on the basis of body weight alone. Methods of achieving weight loss in older adults are the same as in younger adults. 99 Weight loss diets should be combined with an exercise program to preserve muscle mass, as dieting results in loss of muscle as well as fat, and older people already have reduced skeletal muscle mass. Weight loss drugs have not been extensively studied in older people, and there is the potential for drug side effects and interactions. Weight loss surgery appears to be safe and effective, albeit slightly less so than in younger adults, but little is known about the outcomes of such surgery in those aged > 65 years. 99 Older people are at an increased risk of inadequate diet and malnutrition, and the rise in the older population will put more patients at risk. Inadequate diet and malnutrition are associated with a decline in functional status, impaired muscle function, decreased bone mass, immune dysfunction, anemia, reduced cognitive function, poor wound healing, delay in recovering from surgery, and higher hospital and readmission rates and mortality. Aging is associated with a decline in number of physiological functions that can affect nutritional status, including reduced lean body mass, changes in cytokine and hormonal levels, delayed gastric emptying, changes in fluid electrolyte regulation, and diminished sense of smell and taste. Pathological causes such as chronic illness, depression, medications and social isolation can all play a role in nutritional inadequacy. Screening is vital in identifying and monitoring patients. The MUST tool has been well validated and is easy to use. Management involves treating pathological causes such as poor dentition and optimizing the management of chronic diseases. Patients with physical or cognitive impairment require special care and attention. Oral liquid high-energy supplements or enteral feeding should be considered in high risk patients or in patients unable to meet daily requirements. The authors declare no conflicts of interest. Welcome to Microsoft Forms!- Create and share online surveys, quizzes, polls, and forms.
- Collect feedback, measure satisfaction, test knowledge, and more.
- Easily design your forms with various question types, themes, and branching logic.
- Analyze your results with built-in charts and reports, or export them to Excel for further analysis.
- Integrate Microsoft Forms with other Microsoft 365 apps, such as Teams, SharePoint, and OneDrive, so you can collaborate with others and access your forms from anywhere.
Explore templates- Template gallery
- Community volunteer registration form
- Employee satisfaction survey
- Competitive analysis study
- Office facility request form
- Vacation and sick leave form
- Post-event feedback survey
- Holiday Party Invitation
Content SearchRapid multi-sectoral needs assessment of populations affected by gu flooding - doloow district, somalia, may 2024, attachments.  KEY FINDINGS A total of 41,858 people are currently living in the flood-affected areas of Doloow district, with 796 people having moved into the affected location in the past two weeks. The survey analysis revealed, the top 3 most urgent NFI needs for the flood-affected people in Doloow district are Tents, Mosquito nets and Blankets. 29% Sites reported that the nearest markets were partially destroyed by floods. 29% sites, open defecation was reported as the prevailing practice for using latrines, which increases the risk of disease outbreaks such as Cholera. 71% sites reporting that only a few flood-affected people have access to sufficient quantities of drinking water. Due to the damage caused by the flooding, health facilities have been adversely affected, leading to an increased demand for health services in 29% sites. Related ContentRapid multi-sectoral needs assessment of populations affected by gu flooding - jowhar district, somalia, may 2024, rapid multi-sectoral needs assessment of populations affected by gu flooding - north gaalkacyo and jariiban district, somalia, may 2024, rapid multi-sectoral needs assessment of populations affected by gu flooding - kismayo district, somalia, may 2024, rapid multi-sectoral needs assessment of populations affected by gu flooding - afmadow district, somalia, may 2024.  |




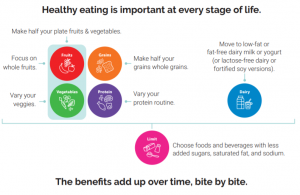

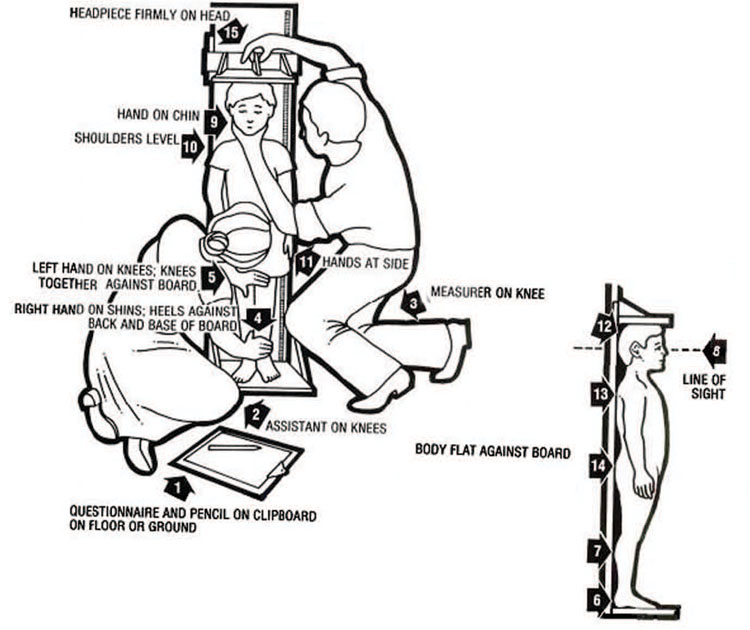
























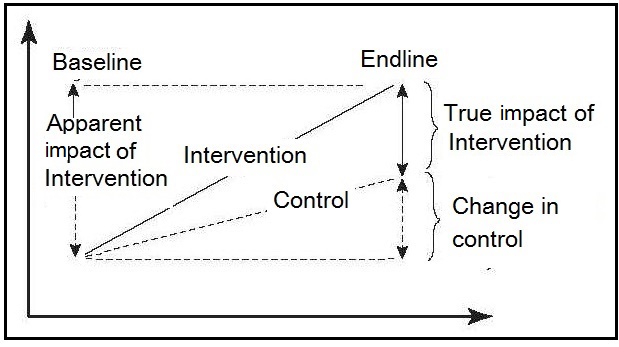
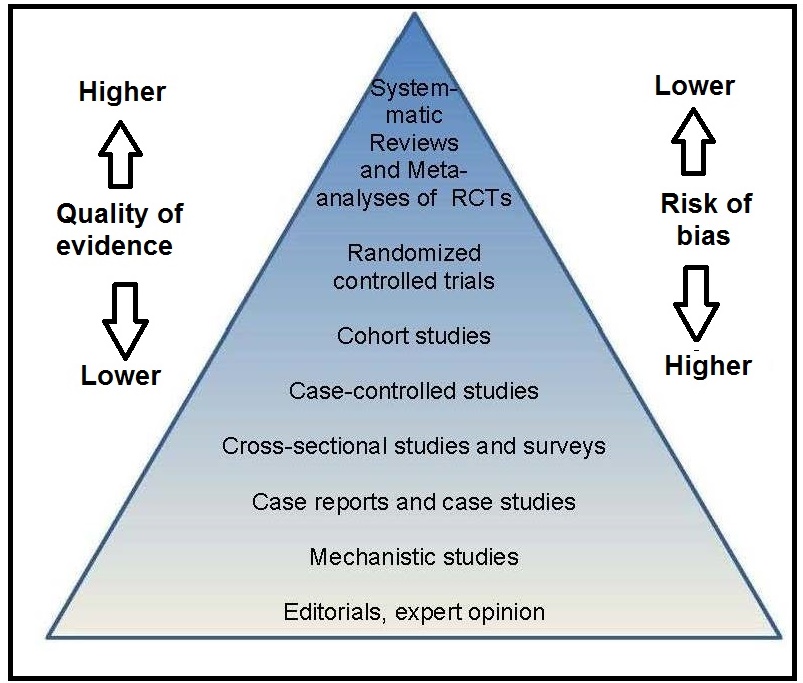

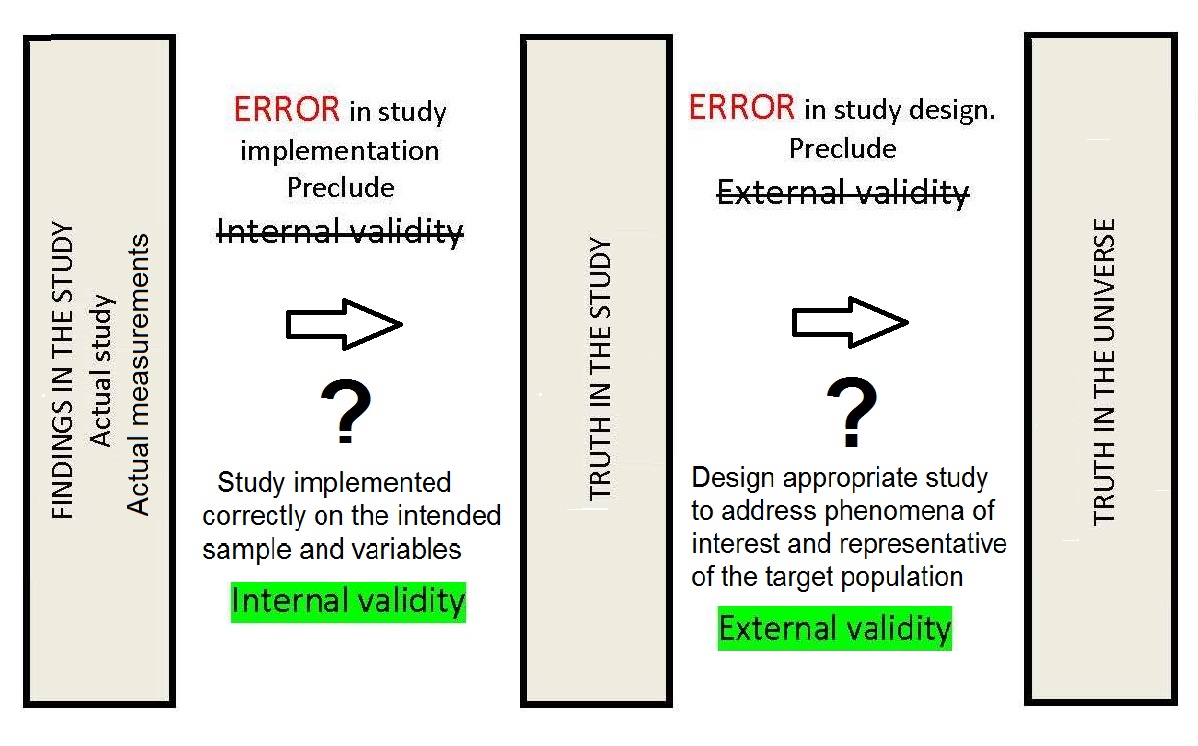
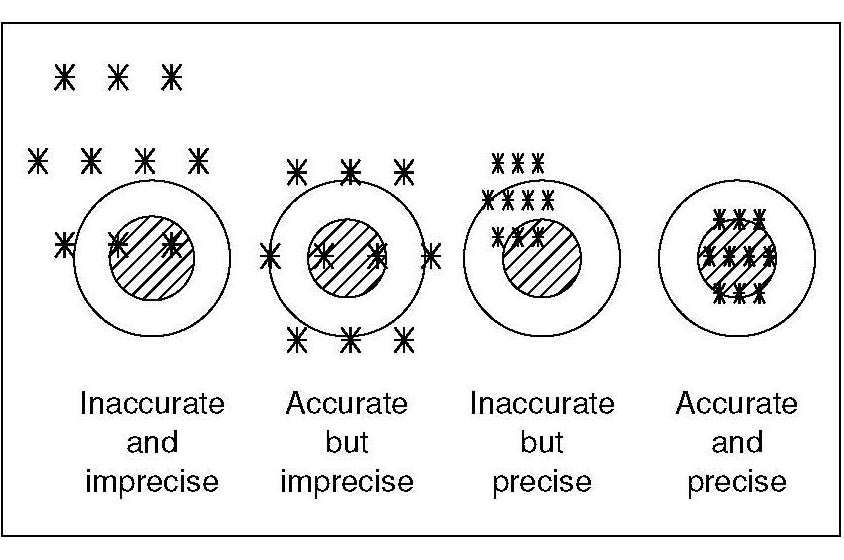
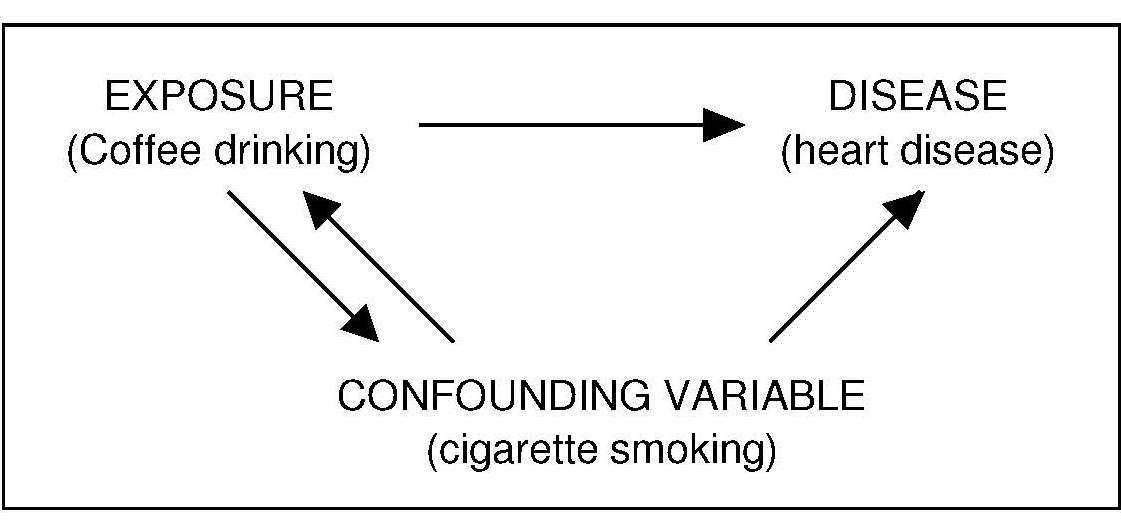
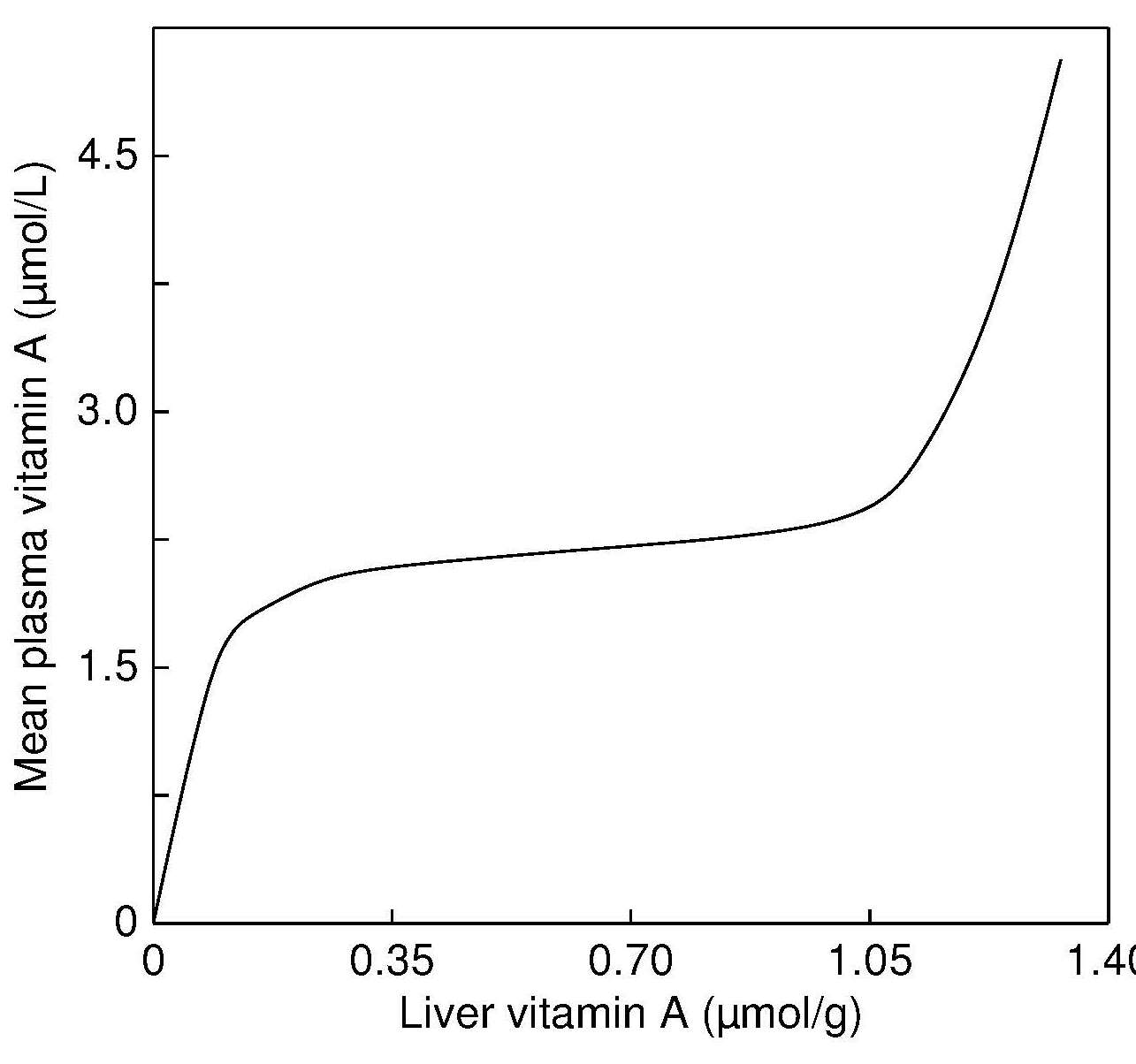
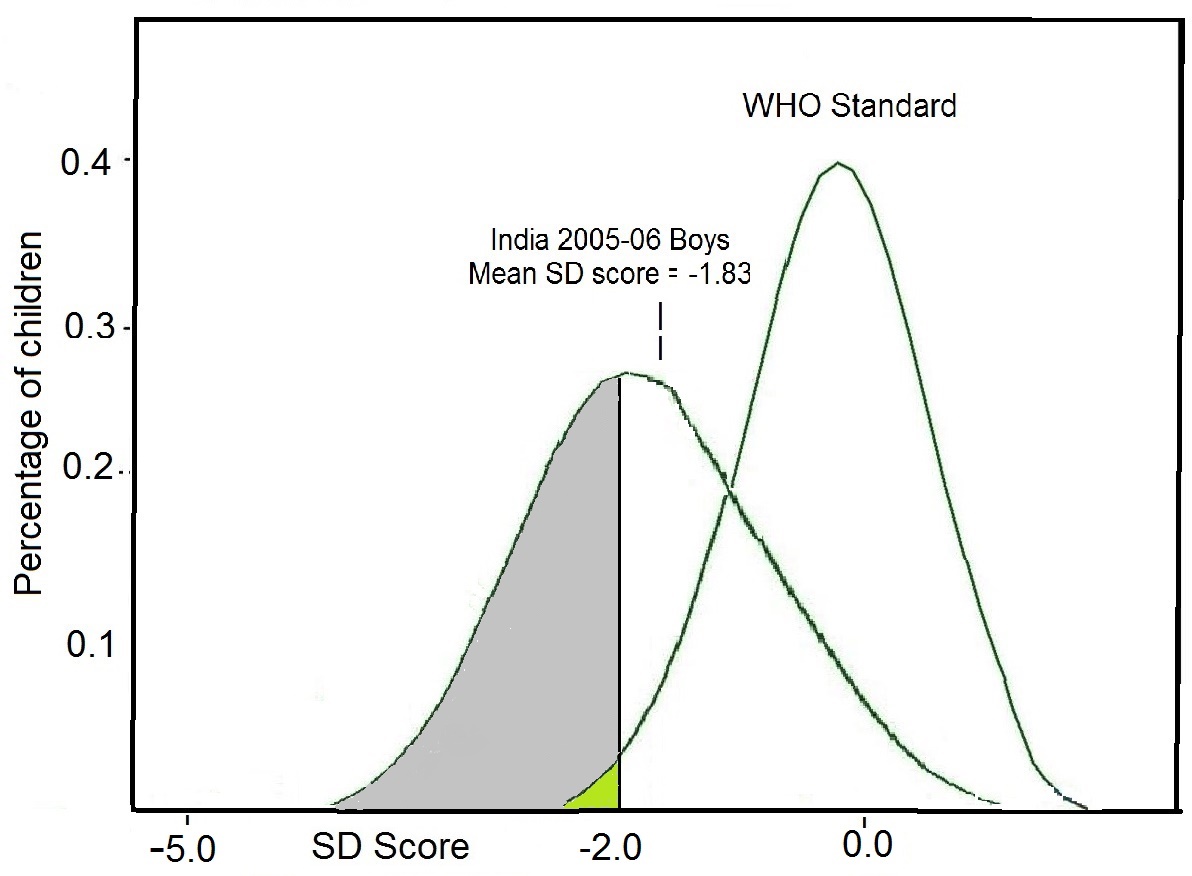
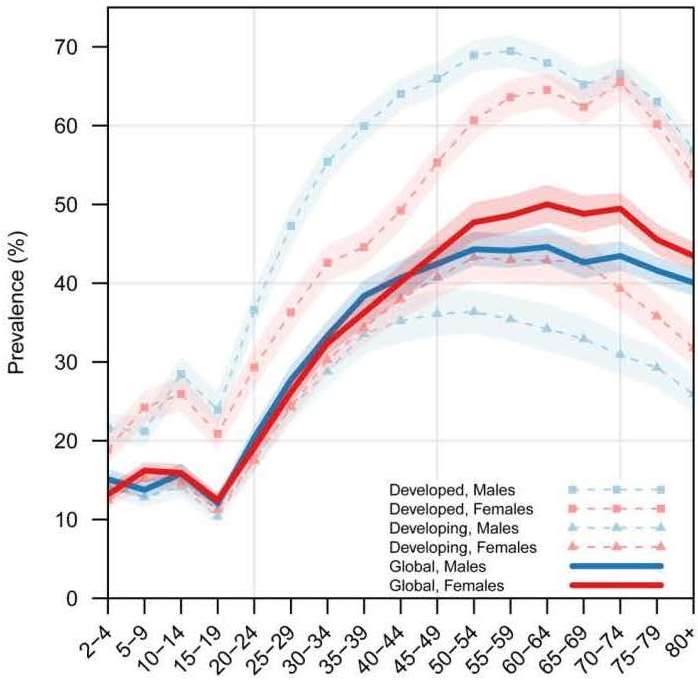






IMAGES
VIDEO
COMMENTS
Food and nutrition are basic indispensable needs of humans. Nutrition plays a critical role in maintaining the health and well-being of individuals and is also an essential component of the healthcare delivery system. The nutritional status of individuals affects the clinical outcomes. Essential nutrients are classified into six groups, namely carbohydrates, proteins, lipids, minerals ...
NACS USER'S GUIDE MODULE 2, VERSION 2. To detect practices that can increase the risk of malnutriion and infection. To inform nutrition education and counseling. To establish appropriate nutrition care plans. The results of a client's nutrition assessment and classification of nutritional status determine all the other elements of nutrition ...
The final part of writing the assessment summary is just plain good advice for your dietetic internship. As an intern, the best practice is to follow your preceptor's lead. If your preceptor likes to keep the summary box short and simple, then you keep the information you put in the summary section nice and short.
The Nutritional Assessment Form is one way to gather client information. While an interview during an initial consultation is crucial, this form can provide an overview of the client's status. Additionally, it can serve as a guide during the consultation for parts needing clarification and emphasis. It will also serve as a record of your ...
Problems with intake such as indigestion, heartburn, bloating, difficulty chewing or swallowing will affect nutritional status. If the patient has a specific concerns about hair, skin, or nails, a focused assessment regarding to the specific sign/symptom should be performed. 3. Check. Height and weight.
1.5 Nutrition Assessment University of Hawai'i at Mānoa Food Science and Human Nutrition Program. Nutrition Assessment. Nutritional assessment is the interpretation of anthropometric, biochemical (laboratory), clinical and dietary data to determine whether a person or groups of people are well nourished or malnourished (overnourished or undernourished).
To make writing these notes as easy as possible for you, use this complete guide on writing clear and simple nutrition notes. It's divided into 2 parts. Part 1: Structure of a nutritional assessment. Part 2: Phrasing in a nutritional assessment. In this post you'll:
Nutritional assessment in adults should begin on first contact with the patient, and is an ongoing process that can take place over several hours or days. A comprehensive nutritional assessment involves the nurse examining the patient's physical and psychological state, as well as considering any social issues that may affect their nutrition. ».
Such an assessment provides an overview of nutritional status; it focuses on nutrient intake analysis of the diet, which is then compared with blood tests and physical examination. With comprehensive data on diet and biological parameters, the physician or other healthcare professional can more accurately assess a person's nutritional status.
Nutritional assessment determines the factors that affect or reflect nutritional health and can be used to evaluate the status of individuals or populations. Food components are two main types, namely macronutrients which include carbohydrate, fat, and protein, and micronutrients comprising vitamins and minerals.
Dietary assessment is the fourth method of comprehensive nutritional status assessment. It evaluates the food and nutrient intake and dietary pattern of individual/s in the household or a population over a period of time. Methods of individual-based dietary assessment can be classified as shown below (Fig. 14.24 ):
1. Introduction. Nutritional assessment is a key process for collecting various information to determine whether a person is malnourished and to define the type and severity of malnutrition, which in turn allows deciding which intervention to perform and provides a starting point for the patient follow up [1].Therefore, nutritional assessment is key to achieving early diagnosis (2) and ...
Nutritional Assessment, Sixth Edition explains the tools and techniques that nutrition practitioners and other health care providers can use to assess diet and nutritional status in instances of acute illness as well as chronic disease prevention and treatment. Key features of this edition include: Detailed discussion of the role of nutritional ...
In the realm of nutrition care, a well-structured nutrition assessment is key to understanding and addressing a client's unique needs. In this blog post, we'll delve into the intricacies of nutrition assessment forms; what nutrition assessment entails and what to include in effective intake forms and chart notes to simplify the process. Understanding Nutrition Assessment […]
Dietary assessment is the process of collecting information about what a person eats and drinks over a period of time. In other words, it is a record of the foods one eats in an attempt to calculate their potential nutrient intake. During a dietary assessment, the health practitioner analyzes the energy, nutrients, and other dietary ...
Nutritional assessment systems involve the interpretation of information from dietary and nutritional biomarkers, and anthropometric and clinical studies. ... studies to estimate the effect of a treatment on an outcome when selection bias due to nonrandom treatment assignment is likely. By creating a propensity score, ...
A nutritional assessment provides an overview of nutritional status; it focuses on nutrient intake analysis of the diet, which is then compared with blood tests and physical examination. With comprehensive data on diet and biological information, the physician can make an accurate estimate of that person's nutritional status. Decisions can ...
Nutrition Assessment is the very first step in the Registered Dietitian Nutritionist's Nutrition Care Process (NCP). The Two Purposes of the Nutrition Assessment: To collect as much data as possible about your patient. To interpret this data to help identify any nutrition-related problems, which leads into the second stage of the NCP, which ...
Abstract. Nutrition is an important element of health in the older population and affects the aging process. The prevalence of malnutrition is increasing in this population and is associated with a decline in: functional status, impaired muscle function, decreased bone mass, immune dysfunction, anemia, reduced cognitive function, poor wound ...
Introduction. "Nutritional assessment can be defined as the interpretation from dietary, laboratory, anthropometric, and clinical studies. It is used to determine the nutritional status of individual or population groups as influenced by the intake and utilization of nutrients" ( Gibson, 2005 ).
State the purposes of a nutritional assessment. (p. 182) They are noninvasive, inexpensive, and easy to perform. Its easily based on obtained datat, nutrition screening is a quick and easy way to identify those at nutrition risk such as weight loss, inadequate food intake, or recent illness. Describe the components of a nutritional assessment. (p.
Assignments. 100% (25) 6. Discussion post week 2 . Nutrition. Assignments. 100% (4) 8. NURS 225 - Nutrition Assessment. Nutrition. Assignments. 100% (3) 5. Discussion week 1 N225 . ... The components of a nutritional assessment can include diet history and physical assessment to determine the status. Firstly, obtaining a diet history can help ...
Nutrition Assessment nurs 225: nutritional part 10 points subjective information. answer each question: family history: (check. Skip to document. University; High School. Books; ... Assignments. 100% (28) 6. Discussion post week 2 . Nutrition. Assignments. 100% (4) 2. Bowel Case Study - notes. Nutrition. Lecture notes.
Use Microsoft Forms to easily create online surveys, forms, quizzes and questionnaires. AI powered, free survey tool from Microsoft.
cultural orientation and develop goals for self-improvement (e.g., Tratify self-assessment, Implicit Activities, self-reflection assignments) KRDN 5.2: Identify and articulate one's skills, strengths, knowledge and experiences relevant to the position desired and career goals (i.e., self-reflection assignments, resume, e-portfolio).
Assessment in English on Somalia about Education, Food and Nutrition, Flash Flood, Flood and more; published on 18 Jun 2024 by iMMAP Inc.